Full Prescribing Information for BREYANZI
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bispecific T-Cell Redirection Versus Chimeric Antigen Receptor (CAR)-T Cells As Approaches to Kill Cancer Cells
Bispecific T-Cell Redirection versus Chimeric Antigen Receptor (CAR)-T Cells as Approaches to Kill Cancer Cells William R. Strohl 1,* and Michael Naso 2 1 BiStro Biotech Consulting, LLC, 1086 Tullo Farm Rd., Bridgewater, NJ 08807, USA 2 Century Therapeutics, 3675 Market St., Philadelphia, PA 19104, USA * Correspondence: [email protected]; Tel.: +1-908-745-8576 Received: 27 May 2019; Accepted: 24 June 2019; Published: 3 July 2019 Abstract: The concepts for T-cell redirecting bispecific antibodies (TRBAs) and chimeric antigen receptor (CAR)-T cells are both at least 30 years old but both platforms are just now coming into age. Two TRBAs and two CAR-T cell products have been approved by major regulatory agencies within the last ten years for the treatment of hematological cancers and an additional 53 TRBAs and 246 CAR cell constructs are in clinical trials today. Two major groups of TRBAs include small, short- half-life bispecific antibodies that include bispecific T-cell engagers (BiTE®s) which require continuous dosing and larger, mostly IgG-like bispecific antibodies with extended pharmacokinetics that can be dosed infrequently. Most CAR-T cells today are autologous, although significant strides are being made to develop off-the-shelf, allogeneic CAR-based products. CAR-Ts form a cytolytic synapse with target cells that is very different from the classical immune synapse both physically and mechanistically, whereas the TRBA-induced synapse is similar to the classic immune synapse. Both TRBAs and CAR-T cells are highly efficacious in clinical trials but both also present safety concerns, particularly with cytokine release syndrome and neurotoxicity. -

Breyanzi (Lisocabtagene Maraleucel)
Breyanzi (Lisocabtagene maraleucel) Commercial and Qualified Health Plans MassHealth Authorization required X X No Prior Authorization Breyanzi is a chimeric antigen receptor T cell therapy (CAR-T), designed to harness the power of the patient’s immune system to recognize and attack their cancer cells. CAR-T is a type of treatment where white blood cells (T cells) are modified in a laboratory to add a gene that helps the patient’s own T cells target their cancer. FDA-Approved Indication Breyanzi is a CD19-directed genetically modified autologous T-cell immunotherapy indicated for the treatment of: • Adult patients with relapsed or refractory large B-cell lymphoma (LBCL) after two or more lines of systemic therapy including: − Diffuse large B-cell lymphoma (DLBCL) not otherwise specified (including DLBCL arising from indolent lymphoma); − Primary mediastinal large B-cell lymphoma; − High grade B-cell lymphoma; and − DLBCL arising from follicular lymphoma grade 3B • Brenyazi is not indicated for the therapy of primary central nervous system lymphoma. Criteria 1. Criteria for Initial Approval Authorization of a single treatment may be granted to patients 18 years of age or older for treatment of Large B-cell lymphoma (including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, primary mediastinal large B-cell lymphoma, high grade B-cell lymphoma, and DLBCL arising from follicular lymphoma) when ALL of the following criteria are met: A. The disease is relapsed or refractory to treatment after two or more lines of systemic therapy. B. The patient has not received a previous treatment course of Breyanzi, Kymriah, or Yescarta. -

Lisocabtagene Maraleucel (Breyanzi®) Policy Number: 291 Effective Date: 07/01/2021 Last Review: 05/27/2021 Next Review Date: 05/27/2022
MEDICAL COVERAGE POLICY SERVICE: Lisocabtagene Maraleucel (Breyanzi®) Policy Number: 291 Effective Date: 07/01/2021 Last Review: 05/27/2021 Next Review Date: 05/27/2022 Important note Unless otherwise indicated, this policy will apply to all lines of business. Even though this policy may indicate that a particular service or supply may be considered medically necessary and thus covered, this conclusion is not based upon the terms of your particular benefit plan. Each benefit plan contains its own specific provisions for coverage and exclusions. Not all benefits that are determined to be medically necessary will be covered benefits under the terms of your benefit plan. You need to consult the Evidence of Coverage (EOC) or Summary Plan Description (SPD) to determine if there are any exclusions or other benefit limitations applicable to this service or supply. If there is a discrepancy between this policy and your plan of benefits, the provisions of your benefits plan will govern. However, applicable state mandates will take precedence with respect to fully insured plans and self-funded non-ERISA (e.g., government, school boards, church) plans. Unless otherwise specifically excluded, Federal mandates will apply to all plans. With respect to Medicare-linked plan members, this policy will apply unless there are Medicare policies that provide differing coverage rules, in which case Medicare coverage rules supersede guidelines in this policy. Medicare-linked plan policies will only apply to benefits paid for under Medicare rules, and not to any other health benefit plan benefits. CMS's Coverage Issues Manual can be found on the CMS website. -

Advances in Car T-Cell Therapy
12/15/2020 ADVANCES IN CAR T-CELL THERAPY Iris Isufi, MD Co-Director, Adult CAR T-Cell Therapy Program Yale Cancer Center/Smilow Cancer Hospital Assistant Professor, Medicine Yale University School of Medicine New Haven, CT 1 DISCLOSURES Advances in CAR T-cell Therapy Iris Isufi, MD, has affiliations with Astra Zeneca, Celgene, Kite Pharmaceuticals and Novartis (Consultant). 2 1 12/15/2020 Objectives • Why CAR T-cell (chimeric antigen receptor T-cell) therapy shows promise for blood cancers • Approved and emerging CAR T-cell therapies • Side effects of CAR T-cell therapy: what to expect • The future of CAR T-cell therapy for blood cancer patients 3 Multiple Mechanisms of Modulating Immune System to Treat Cancer • Monoclonal antibodies or antibody drug conjugates • Dual antigen re- targeting proteins • Immune checkpoint antibodies • Chimeric antigen receptor T cells Batlevi, C. L. et al, Nat. Rev. Clin. Oncol, 2015 4 2 12/15/2020 What is CAR T-cell therapy? CAR T-cell therapy is a type of cancer therapy that uses a patient’s own modified white blood cells to kill cancer cells. 5 CAR T-Cells are at The Intersection of Three Innovative Technologies Cellular therapy Using the patient’s own T- cells as therapy Cellular Gene therapy therapy Gene therapy Insertion of genes into a patient’s cells, thereby causing these cells to produce a new therapeutic protein (CAR) Immunotherapy Immunotherapy Harnessing the patient’s own immune system (T- cells) to treat his/her disease 6 3 12/15/2020 Tragedy, Perseverance, and Chance — The Story of CAR-T Therapy The emergence of CAR-T therapy, like most scientific advances, reflects the incremental insights of hundreds of scientists over decades. -

Breyanzi (Lisocabtagene Maraleucel) Medical Drug Program Summary
Breyanzi (lisocabtagene maraleucel) Medical Drug Program Summary For patients with late stage metastatic disease (Stage IV), please refer to MP 2.373 Step Therapy Treatment in Cancer, Including Treatments for Stage Four, Advanced Metastatic Cancer and Severe Related Health Conditions for additional guidance. FDA APPROVED INDICATIONS AND DOSAGE1 Agent(s) Indication(s) Dosage Breyanzi® • Treatment of adult BLBCL: (lisocabtagene maraleucel) patients with relapsed or A single dose of Breyanzi refractory large B-cell contains 50 to 110 X 106 Suspension for intravenous lymphoma after two or CAR-positive viable T cells infusion more lines of systemic (consisting of 1:1 CAR- therapy, including positive viable T cells of the diffuse large B-cell CD8 and CD4 components) lymphoma (DLBCL) not with each component otherwise specified supplied separately in one (including DLBCL arising to four single-dose vials. from indolent See the respective lymphoma), high-grade Certificate of Release for B-cell lymphoma, Infusion (RFI Certificate) for primary mediastinal each component for the large B-cell lymphoma, actual cell counts and and follicular lymphoma volumes to be infused grade 3B Limitations of Use: Breyanzi is not indicated for treatment of patients with primary central nervous system lymphoma CLINICAL RATIONALE Diffuse Large B-cell Lymphoma Diffuse large B-cell lymphoma (DLBCL) is a subtype of non-Hodgkin lymphomas (NHL). DLBCL are the most common lymphoid neoplasms in adults, accounting for approximately 30% of NHLs diagnosed annually. Immunophenotypic analysis is essential for the differentiation of the various subtypes of NHL to establish the proper diagnosis. This can be performed by flow cytometry and/or immunohistochemistry (IHC). -

Toxicity of CAR-T Cells and the Role of Immunity
International Journal of Molecular Sciences Review A New Era in Endothelial Injury Syndromes: Toxicity of CAR-T Cells and the Role of Immunity Eleni Gavriilaki 1,* , Ioanna Sakellari 1, Maria Gavriilaki 2 and Achilles Anagnostopoulos 1 1 Hematology Department—BMT Unit, G Papanicolaou Hospital, 57010 Thessaloniki, Greece; [email protected] (I.S.); [email protected] (A.A.) 2 Laboratory of Clinical Neurophysiology, AHEPA Hospital, Aristotle University of Thessaloniki, 54636 Thessaloniki, Greece; [email protected] * Correspondence: [email protected]; Tel.: +30-2313-307-550 Received: 28 April 2020; Accepted: 28 May 2020; Published: 29 May 2020 Abstract: Immunotherapy with chimeric antigen receptor T (CAR-T cells) has been recently approved for patients with relapsed/refractory B-lymphoproliferative neoplasms. Along with great efficacy in patients with poor prognosis, CAR-T cells have been also linked with novel toxicities in a significant portion of patients. Cytokine release syndrome (CRS) and neurotoxicity present with unique clinical phenotypes that have not been previously observed. Nevertheless, they share similar characteristics with endothelial injury syndromes developing post hematopoietic cell transplantation (HCT). Evolution in complement therapeutics has attracted renewed interest in these life-threatening syndromes, primarily concerning transplant-associated thrombotic microangiopathy (TA-TMA). The immune system emerges as a key player not only mediating cytokine responses but potentially contributing to endothelial injury in CAR-T cell toxicity. The interplay between complement, endothelial dysfunction, hypercoagulability, and inflammation seems to be a common denominator in these syndromes. As the indications for CAR-T cells and patient populations expand, there in an unmet clinical need of better understanding of the pathophysiology of CAR-T cell toxicity. -

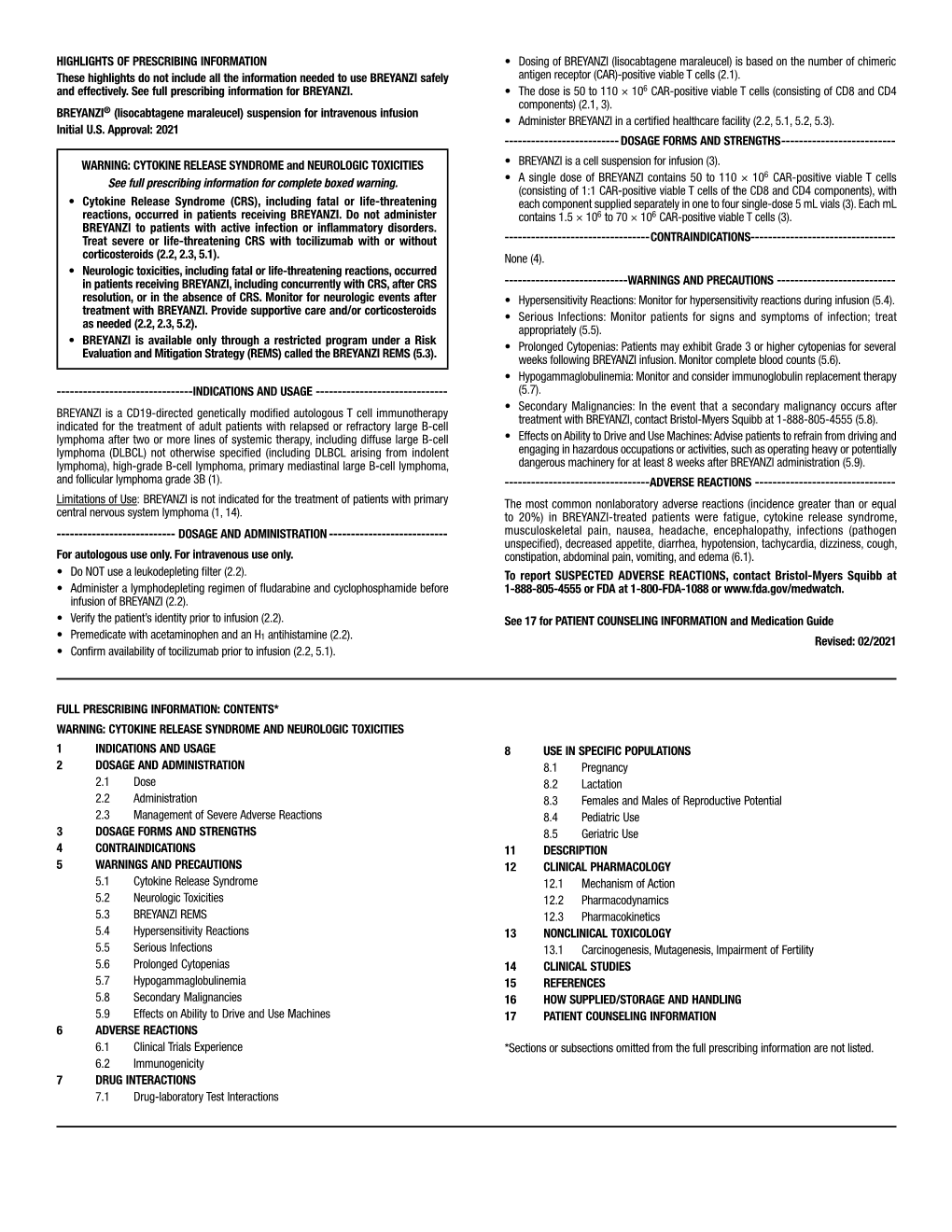
These Highlights Do Not Include All the Information Needed to Use BREYANZI Safely and Effectively. See Full Prescribing Information for BREYANZI
BREYANZI- lisocabtagene maraleucel Juno Therapeutics, Inc. ---------- HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use BREYANZI safely and effectively. See full prescribing information for BREYANZI. BREYANZI® (lisocabtagene maraleucel) suspension for intravenous infusion Initial U.S. Approval: 2021 WARNING: CYTOKINE RELEASE SYNDROME and NEUROLOGIC TOXICITIES See full prescribing information for complete boxed warning. Cytokine Release Syndrome (CRS), including fatal or life-threatening reactions, occurred in patients receiving BREYANZI. Do not administer BREYANZI to patients with active infection or inflammatory disorders. Treat severe or life-threatening CRS with tocilizumab with or without corticosteroids (2.2, 2.3, 5.1). Neurologic toxicities, including fatal or life-threatening reactions, occurred in patients receiving BREYANZI, including concurrently with CRS, after CRS resolution, or in the absence of CRS. Monitor for neurologic events after treatment with BREYANZI. Provide supportive care and/or corticosteroids as needed (2.2, 2.3, 5.2). BREYANZI is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the BREYANZI REMS (5.3). INDICATIONS AND USAGE BREYANZI is a CD19-directed genetically modified autologous T cell immunotherapy indicated for the treatment of adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified (including DLBCL arising from indolent lymphoma), high-grade B-cell lymphoma, primary mediastinal large B-cell lymphoma, and follicular lymphoma grade 3B (1). Limitations of Use: BREYANZI is not indicated for the treatment of patients with primary central nervous system lymphoma (1, 14). -

Package Insert
6 HIGHLIGHTS OF PRESCRIBING INFORMATION • The dose is 50 to 110 × 10 CAR-positive viable T cells These highlights do not include all the information needed to use (consisting of CD8 and CD4 components) (2.1, 3). BREYANZI safely and effectively. See full prescribing information for • Administer BREYANZI in a certified healthcare facility (2.2, 5.1, BREYANZI. 5.2, 5.3). ® ______________ ______________ BREYANZI (lisocabtagene maraleucel) suspension for intravenous DOSAGE FORMS AND STRENGTHS infusion • BREYANZI is a cell suspension for infusion (3). Initial U.S. Approval: 2021 • A single dose of BREYANZI contains 50 to 110 × 106 CAR- positive viable T cells (consisting of 1:1 CAR-positive viable T WARNING: CYTOKINE RELEASE SYNDROME and cells of the CD8 and CD4 components), with each component NEUROLOGIC TOXICITIES supplied separately in one to four single-dose 5 mL vials (3). Each See full prescribing information for complete boxed warning. mL contains 1.5 × 106 to 70 × 106 CAR-positive viable T cells (3). • Cytokine Release Syndrome (CRS), including fatal or life- ___________________ ____________________ threatening reactions, occurred in patients receiving CONTRAINDICATIONS BREYANZI. Do not administer BREYANZI to patients None (4). with active infection or inflammatory disorders. Treat _____ __________ _______________ severe or life-threatening CRS with tocilizumab with or WARNINGS AND PRECAUTIONS without corticosteroids (2.2, 2.3, 5.1). • Hypersensitivity Reactions: Monitor for hypersensitivity reactions • Neurologic toxicities, including fatal or life-threatening during infusion (5.4). reactions, occurred in patients receiving BREYANZI, • Serious Infections: Monitor patients for signs and symptoms of including concurrently with CRS, after CRS resolution, or infection; treat appropriately (5.5). -

Breyanzi® (Lisocabtagene Maraleucel) (Intravenous) Document Number: IC-0590 Last Review Date: 03/01/2021 Date of Origin: 03/01/2021 Dates Reviewed: 03/2021
Breyanzi® (lisocabtagene maraleucel) (Intravenous) Document Number: IC-0590 Last Review Date: 03/01/2021 Date of Origin: 03/01/2021 Dates Reviewed: 03/2021 I. Length of Authorization Coverage will be provided for one treatment course (1 dose of Breyanzi) and may not be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Unit]: • 1 carton (1 to 4 vials) B. Max Units (per dose and over time) [HCPCS Unit]: • 1 infusion of up to 110 million autologous anti-cd19 car -positive viable t-cells III. Initial Approval Criteria 1-7 Submission of medical records related to the medical necessity criteria is REQUIRED on all requests for authorizations. Records will be reviewed at the time of submission. Please provide documentation via direct upload through the PA web portal or by fax. Coverage is provided in the following conditions: • Patient does not have a clinically significant active systemic infection or inflammatory disorder; AND • Patient has not received live vaccines within 6 weeks prior to the start of lymphodepleting chemotherapy, during lisocabtagene maraleucel treatment, and will not receive live vaccines until immune recovery following treatment; AND • Patient has been screened for hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) in accordance with clinical guidelines prior to collection of cells (leukapheresis); AND • Prophylaxis for infection has been followed according to local guidelines; AND Proprietary & Confidential © 2021 Magellan Health, Inc. • Healthcare facility has enrolled -

Lisocabtagene Maraleucel (Breyanzi)
Clinical Policy: Lisocabtagene Maraleucel (Breyanzi) Reference Number: ERX.SPA.392 Effective Date: 02.05.21 Last Review Date: 08.21 Line of Business: Commercial, Medicaid Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Lisocabtagene maraleucel (Breyanzi®) is a CD19-directed genetically modified autologous T-cell immunotherapy. FDA Approved Indication(s) Breyanzi is indicated for the treatment of adult patients with relapsed or refractory large B-cell lymphoma (LBCL) after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified (including DLBCL arising from indolent lymphoma), high-grade B-cell lymphoma, primary mediastinal large B-cell lymphoma, and follicular lymphoma grade 3B. Limitation of use: Breyanzi is not indicated for the treatment of patients with active primary central nervous system (CNS) lymphoma. Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. Health plan approved formularies should be reviewed for all coverage determinations. Requirements to use preferred alternative agents apply only when such requirements align with the health plan approved formulary. It is the policy of health plans affiliated with Envolve Pharmacy Solutions™ that Breyanzi is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Large B-Cell Lymphoma* (must meet all): *Only for initial treatment dose; subsequent doses will not be covered. 1. Diagnosis of one of the following LBCL (a–f ); a. DLBCL; b. DLBCL transformed from one of the following (i – v): i. -

066 Chimeric Antigen Receptor Therapy for Hematologic Malignancies
Medical Policy Chimeric Antigen Receptor Therapy for Leukemia and Lymphoma Table of Contents • Policy: Commercial • Coding Information • Information Pertaining to All Policies • Policy: Medicare • Description • References • Authorization Information • Policy History Policy Number: 066 BCBSA Reference Number: 8.01.63 Related Policies • Adoptive Immunotherapy #455 • CAR T-Cell Therapy Services for B-cell Acute Lymphoblastic Leukemia (tisagenlecleucel) Prior Authorization Request Form #925 • CAR T-Cell Therapy Services for Diffuse Large B-cell Lymphoma (axicabtagene cilleucel or tisagenlecleucel) Prior Authorization Request Form #924 • CAR T-Cell Therapy Services for Follicular Lymphoma (Axicabtagene Ciloleucel) Prior Authorization Request Form #944 • CAR T-Cell Therapy Services for Mantle Cell Lymphoma (Brexucabtagene Autoleucel) Prior Authorization Request Form #940 • CAR T-Cell Therapy Services for Non-Hodgkin Lymphoma (Lisocabtagene Maraleucel) Prior Authorization Request Form #941 • Cellular Immunotherapy for Prostate Cancer #268 Policy Commercial Members: Managed Care (HMO and POS), PPO, and Indemnity *Prior Authorization Request Form: Chimeric Antigen Receptor Therapy for Hematologic Malignancies This form must be completed and faxed to: Medical and Surgical: 888-973-0726; Medicare Advantage: 1-800-447-2994. • Click here for CAR T-Cell Therapy Services for Diffuse Large B-cell Lymphoma (axicabtagene cilleucel or tisagenlecleucel) Prior Authorization Request Form #924 • Click here for CAR T-Cell Therapy Services for B-cell Acute Lymphoblastic -

Breyanzi (Lisocabtagene Maraleucel)
Breyanzi (lisocabtagene maraleucel) Policy Origination Date: April 5, 2021 Number: MG.MM.PH.324 Medical Guideline Disclaimer Property of EmblemHealth. All rights reserved. The treating physician or primary care provider must submit to EmblemHealth the clinical evidence that the patient meets the criteria for the treatment or surgical procedure. Without this documentation and information, EmblemHealth will not be able to properly review the request for prior authorization. The clinical review criteria expressed below reflects how EmblemHealth determines whether certain services or supplies are medically necessary. EmblemHealth established the clinical review criteria based upon a review of currently available clinical information (including clinical outcome studies in the peer-reviewed published medical literature, regulatory status of the technology, evidence-based guidelines of public health and health research agencies, evidence-based guidelines and positions of leading national health professional organizations, views of physicians practicing in relevant clinical areas, and other relevant factors). EmblemHealth expressly reserves the right to revise these conclusions as clinical information changes and welcomes further relevant information. Each benefit program defines which services are covered. The conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered and/or paid for by EmblemHealth, as some programs exclude coverage for services or supplies that EmblemHealth considers medically necessary. If there is a discrepancy between this guideline and a member's benefits program, the benefits program will govern. In addition, coverage may be mandated by applicable legal requirements of a state, the Federal Government or the Centers for Medicare & Medicaid Services (CMS) for Medicare and Medicaid members.