Mean Arterial Pressure 2
Total Page:16
File Type:pdf, Size:1020Kb
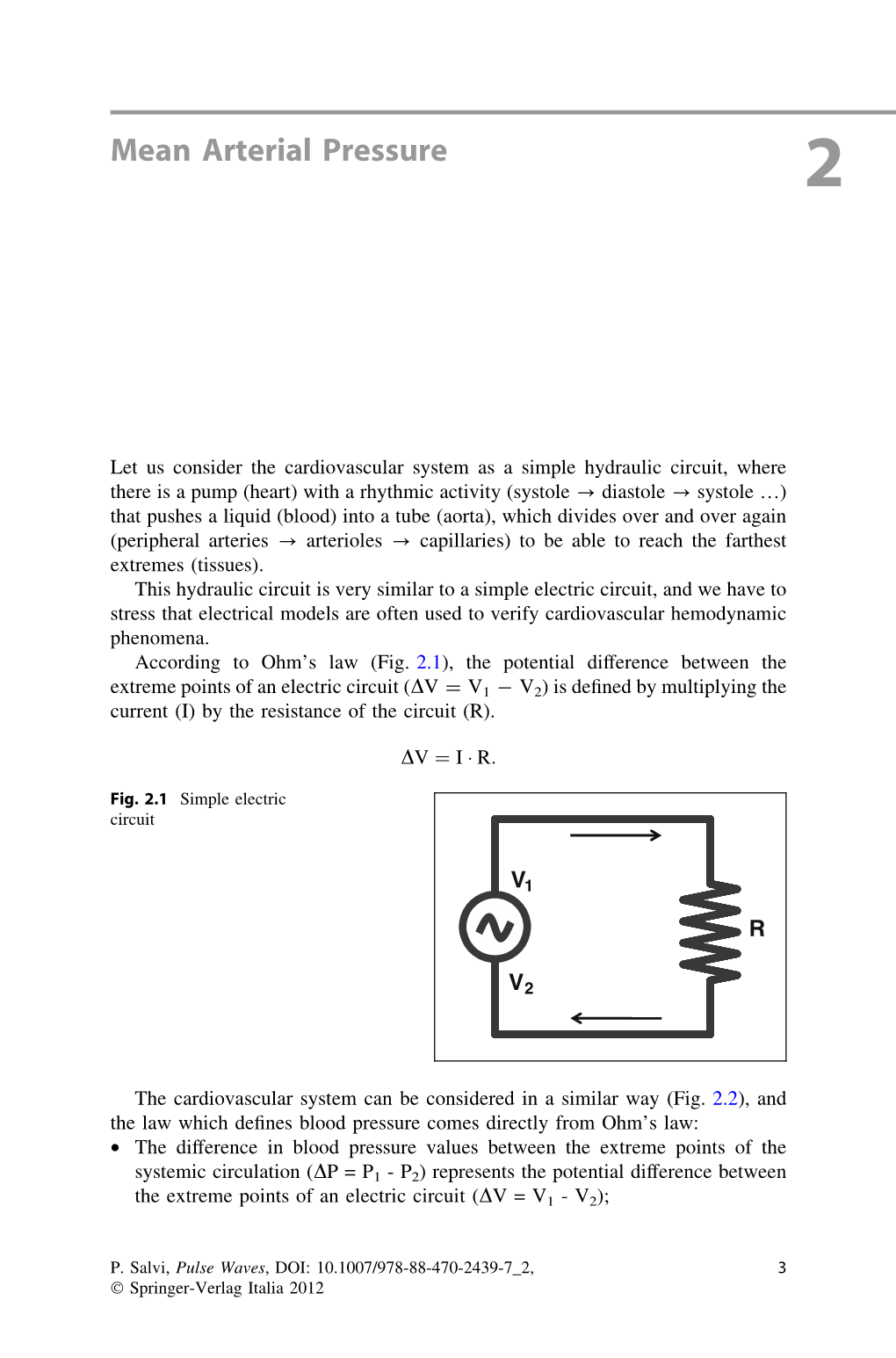
Load more
Recommended publications
-

Pressure on Perfusion - Mean Arterial Pressure in Relation to Cerebral Ischemia and Kidney Injury
Pressure on Perfusion - Mean Arterial Pressure in Relation to Cerebral Ischemia and Kidney Injury Line Larsen and Carina Dyhr Jørgensen Affiliation: Department of Cardiac Thoracic Surgery University Hospital Odense Sdr. Boulevard 29 5000 Odense C, Denmark Supervisor: Claus Andersen, MD, Consultant Anaesthesiologist, Department of Anaesthesiology, V, OUH. Poul Erik Mortensen, MD, Consultant Surgeon, Department of Cardiac Thoracic Surgery, T, OUH. Pressure on Perfusion Line Larsen and Carina Dyhr Jørgensen Index Abstract ........................................................................................................................................................... 2 Introduction ..................................................................................................................................................... 3 Aim ................................................................................................................................................................ 8 Hypothesis ..................................................................................................................................................... 8 Methodological considerations ....................................................................................................................... 9 Materials and methods .................................................................................................................................. 10 Study design ............................................................................................................................................... -

High Blood Pressure
KNOW THE FACTS ABOUT High Blood Pressure What is high blood pressure? What are the signs and symptoms? Blood pressure is the force of blood High blood pressure usually has no against your artery walls as it circulates warning signs or symptoms, so many through your body. Blood pressure people don’t realize they have it. That’s normally rises and falls throughout the why it’s important to visit your doctor day, but it can cause health problems if regularly. Be sure to talk with your it stays high for a long time. High blood doctor about having your blood pressure pressure can lead to heart disease and checked. stroke—leading causes of death in the United States.1 How is high blood pressure diagnosed? Your doctor measures your blood Are you at risk? pressure by wrapping an inflatable cuff One in three American adults has high with a pressure gauge around your blood pressure—that’s an estimated arm to squeeze the blood vessels. Then 67 million people.2 Anyone, including he or she listens to your pulse with a children, can develop it. stethoscope while releasing air from the cuff. The gauge measures the pressure in Several factors that are beyond your the blood vessels when the heart beats control can increase your risk for high (systolic) and when it rests (diastolic). blood pressure. These include your age, sex, and race or ethnicity. But you can work to reduce your risk by How is it treated? eating a healthy diet, maintaining a If you have high blood pressure, your healthy weight, not smoking, and being doctor may prescribe medication to treat physically active. -

Blood Vessels: Part A
Chapter 19 The Cardiovascular System: Blood Vessels: Part A Blood Vessels • Delivery system of dynamic structures that begins and ends at heart – Arteries: carry blood away from heart; oxygenated except for pulmonary circulation and umbilical vessels of fetus – Capillaries: contact tissue cells; directly serve cellular needs – Veins: carry blood toward heart Structure of Blood Vessel Walls • Lumen – Central blood-containing space • Three wall layers in arteries and veins – Tunica intima, tunica media, and tunica externa • Capillaries – Endothelium with sparse basal lamina Tunics • Tunica intima – Endothelium lines lumen of all vessels • Continuous with endocardium • Slick surface reduces friction – Subendothelial layer in vessels larger than 1 mm; connective tissue basement membrane Tunics • Tunica media – Smooth muscle and sheets of elastin – Sympathetic vasomotor nerve fibers control vasoconstriction and vasodilation of vessels • Influence blood flow and blood pressure Tunics • Tunica externa (tunica adventitia) – Collagen fibers protect and reinforce; anchor to surrounding structures – Contains nerve fibers, lymphatic vessels – Vasa vasorum of larger vessels nourishes external layer Blood Vessels • Vessels vary in length, diameter, wall thickness, tissue makeup • See figure 19.2 for interaction with lymphatic vessels Arterial System: Elastic Arteries • Large thick-walled arteries with elastin in all three tunics • Aorta and its major branches • Large lumen offers low resistance • Inactive in vasoconstriction • Act as pressure reservoirs—expand -

Pathophysiology of the Cardiovascular System and Neonatal Hypotension
Pathophysiology of the Cardiovascular System and Neonatal Hypotension Sandra L. Shead, RNC-NIC, MSN, CNS, NNP-BC Continuing Nursing Education BSTRACT (CNE) Credit A A total of 2.5 contact Hypotension is common in low birth weight neonates and less common in term newborns and is hours may be earned as CNE credit associated with significant morbidity and mortality. Determining an adequate blood pressure in for reading the articles in this issue neonates remains challenging for the neonatal nurse because of the lack of agreed-upon norms. Values identified as CNE and for completing an online posttest and evaluation. for determining norms for blood pressure at varying gestational and postnatal ages are based on To be successful the learner must empirical data. Understanding cardiovascular pathophysiology, potential causes of hypotension, and obtain a grade of at least 80% on assessment of adequate perfusion in the neonatal population is important and can assist the neonatal the test. Test expires three (3) years from publication date. Disclosure: nurse in the evaluation of effective blood pressure. This article reviews cardiovascular pathophysiology The author/planning committee as it relates to blood pressure and discusses potential causes of hypotension in the term and preterm has no relevant financial interest or affiliations with any commercial neonate. Variation in management of hypotension across centers is discussed. Underlying causes and interests related to the subjects pathophysiology of hypotension in the neonate are described. discussed within this article. No commercial support or sponsorship was provided for this educational Keywords: neonatal hypotension; definition; physiology; cardiovascular system; preterm; management; activity. ANN/ANCC does not assessment; cerebral; autoregulation; blood pressure endorse any commercial products discussed/displayed in conjunction with this educational activity. -

The Icefish (Chionodraco Hamatus)
The Journal of Experimental Biology 207, 3855-3864 3855 Published by The Company of Biologists 2004 doi:10.1242/jeb.01180 No hemoglobin but NO: the icefish (Chionodraco hamatus) heart as a paradigm D. Pellegrino1,2, C. A. Palmerini3 and B. Tota2,4,* Departments of 1Pharmaco-Biology and 2Cellular Biology, University of Calabria, 87030, Arcavacata di Rende, CS, Italy, 3Department of Cellular and Molecular Biology, University of Perugia, 06126, Perugia, Italy and 4Zoological Station ‘A. Dohrn’, Villa Comunale, 80121, Napoli, Italy *Author for correspondence (e-mail: [email protected]) Accepted 13 July 2004 Summary The role of nitric oxide (NO) in cardio-vascular therefore demonstrate that under basal working homeostasis is now known to include allosteric redox conditions the icefish heart is under the tonic influence modulation of cell respiration. An interesting animal for of a NO-cGMP-mediated positive inotropism. We also the study of this wide-ranging influence of NO is the cold- show that the working heart, which has intracardiac adapted Antarctic icefish Chionodraco hamatus, which is NOS (shown by NADPH-diaphorase activity and characterised by evolutionary loss of hemoglobin and immunolocalization), can produce and release NO, as multiple cardio-circulatory and subcellular compensations measured by nitrite appearance in the cardiac effluent. for efficient oxygen delivery. Using an isolated, perfused These results indicate the presence of a functional NOS working heart preparation of C. hamatus, we show that system in the icefish heart, possibly serving a both endogenous (L-arginine) and exogenous (SIN-1 in paracrine/autocrine regulatory role. presence of SOD) NO-donors as well as the guanylate cyclase (GC) donor 8Br-cGMP elicit positive inotropism, while both nitric oxide synthase (NOS) and sGC Key words: nitric oxide, heart, Antarctic teleost, icefish, Chionodraco inhibitors, i.e. -

Arterial System Lecture Block 10 Vascular Structure/Function
Arterial System Lecture Block 10 Arterial System Bioengineering 6000 CV Physiology Vascular Structure/Function Arterial System Bioengineering 6000 CV Physiology Functional Overview Arterial System Bioengineering 6000 CV Physiology Vessel Structure Aorta Artery Vein Vena Cava Arteriole Capillary Venule Diameter 25 mm 4 mm 5 mm 30 mm 30 µm 8 µm 20 µm Wall 2 mm 1 mm 0.5 mm 1.5 mm 6 µm 0.5 µm 1 µm thickness Endothelium Elastic tissue Smooth Muscle Fibrous Tissue Arterial System Bioengineering 6000 CV Physiology Aortic Compliance • Factors: – age 20--24 yrs – athersclerosis 300 • Effects – more pulsatile flow 200 dV 30--40 yrs C = – more cardiac work dP 50-60 yrs – not hypertension Laplace’s Law 100 70--75 yrs (thin-walled cylinder): [%] Volume Blood T = wall tension P = pressure T = Pr r = radius For thick wall cylinder 100 150 200 P = pressure Pr Pressure [mm Hg] σ = wall stress r = radius σ = Tension Wall Stress w = wall thickness w [dyne/cm] [dyne/cm2] Aorta 2 x 105 10 x 105 Capillary 15-70 1.5 x 105 Arterial System Bioengineering 6000 CV Physiology Arterial Hydraulic Filter Arterial System Bioengineering 6000 CV Physiology Arterial System as Hydraulic Filter Arterial Cardiac Pressure • Pulsatile --> Output t Physiological smooth flow t Ideal • Cardiac energy conversion Cardiac • Reduces total Output Arterial cardiac work Pressure t Pulsatile t Challenge Cardiac Output Arterial Pressure t Filtered t Reality Arterial System Bioengineering 6000 CV Physiology Elastic Recoil in Arteries Arterial System Bioengineering 6000 CV Physiology Effects of Vascular Resistance and Compliance Arterial System Bioengineering 6000 CV Physiology Cardiac Output vs. -

Vascular Peripheral Resistance and Compliance in the Lobster Homarus Americanus
The Journal of Experimental Biology 200, 477–485 (1997) 477 Printed in Great Britain © The Company of Biologists Limited 1997 JEB0437 VASCULAR PERIPHERAL RESISTANCE AND COMPLIANCE IN THE LOBSTER HOMARUS AMERICANUS JERREL L. WILKENS*,1, GLEN W. DAVIDSON†,1 AND MICHAEL J. CAVEY1,2 1Department of Biological Sciences, The University of Calgary, 2500 University Drive NW, Calgary, Alberta, Canada T2N 1N4 and 2Department of Anatomy, The University of Calgary, 3330 Hospital Drive NW, Calgary, Alberta, Canada T2N 4N1 Accepted 24 October 1996 Summary The peripheral resistance to flow through each arterial become stiffer at pressures greater than peak systolic bed (in actuality, the entire pathway from the heart back pressure and at radii greater than twice the unpressurized to the pericardial sinus) and the mechanical properties of radius. The dorsal abdominal artery possesses striated the seven arteries leaving the lobster heart are measured muscle in the lateral walls. This artery remains compliant and compared. Resistance is inversely proportional to over the entire range of hemolymph pressures expected in artery radius and, for each pathway, the resistance falls lobsters. These trends are illustrated when the non-linearly as flow rate increases. The resistance of the incremental modulus of elasticity is compared among hepatic arterial system is lower than that predicted on the arteries. All arteries should function as Windkessels to basis of its radius. Body-part posture and movement may damp the pulsatile pressures and flows generated by the affect the resistance to perfusion of that region. The total heart. The dorsal abdominal artery may also actively vascular resistance placed on the heart when each artery regulate its flow. -

Pathophysiology of the Right Ventricle And€Of the Pulmonary Circulation In
SERIES | WORLD SYMPOSIUM ON PULMONARY HYPERTENSION Pathophysiology of the right ventricle and of the pulmonary circulation in pulmonary hypertension: an update Anton Vonk Noordegraaf1, Kelly Marie Chin2, François Haddad3, Paul M. Hassoun4, Anna R. Hemnes5, Susan Roberta Hopkins6, Steven Mark Kawut7, David Langleben8, Joost Lumens9,10 and Robert Naeije11,12 Number 3 in the series “Proceedings of the 6th World Symposium on Pulmonary Hypertension” Edited by N. Galiè, V.V. McLaughlin, L.J. Rubin and G. Simonneau Affiliations: 1Amsterdam UMC, Vrije Universiteit Amsterdam, Pulmonary Medicine, Amsterdam Cardiovascular Sciences, Amsterdam, The Netherlands. 2Division of Pulmonary and Critical Care Medicine, University of Texas Southwestern, Dallas, TX, USA. 3Division of Cardiovascular Medicine, Stanford University and Stanford Cardiovascular Institute, Palo Alto, CA, USA. 4Division of Pulmonary and Critical Care Medicine, Johns Hopkins University, Baltimore, MD, USA. 5Division of Allergy, Pulmonary and Critical Care Medicine, Vanderbilt University Medical Center, Nashville, TN, USA. 6Dept of Medicine, University of California, San Diego, La Jolla, CA, USA. 7Penn Cardiovascular Institute, Dept of Medicine, and Center for Clinical Epidemiology and Biostatistics, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA. 8Center for Pulmonary Vascular Disease, Cardiology Division, Jewish General Hospital and McGill University, Montreal, QC, Canada. 9Maastricht University Medical Center, CARIM School for Cardiovascular Diseases, Maastricht, The Netherlands. 10Université de Bordeaux, LIRYC (L’Institut de Rythmologie et Modélisation Cardiaque), Bordeaux, France. 11Dept of Cardiology, Erasme University Hospital, Brussels, Belgium. 12Laboratory of Cardiorespiratory Exercise Physiology, Faculty of Motor Sciences, Université Libre de Bruxelles, Brussels, Belgium. Correspondence: Anton Vonk Noordegraaf, Amsterdam UMC, Vrije Universiteit Amsterdam, Pulmonary Medicine, Amsterdam Cardiovascular Sciences, De Boelelaan 1117, 1081 HV Amsterdam, The Netherlands. -

What Is High Blood Pressure?
ANSWERS Lifestyle + Risk Reduction by heart High Blood Pressure BLOOD PRESSURE SYSTOLIC mm Hg DIASTOLIC mm Hg What is CATEGORY (upper number) (lower number) High Blood NORMAL LESS THAN 120 and LESS THAN 80 ELEVATED 120-129 and LESS THAN 80 Pressure? HIGH BLOOD PRESSURE 130-139 or 80-89 (HYPERTENSION) Blood pressure is the force of blood STAGE 1 pushing against blood vessel walls. It’s measured in millimeters of HIGH BLOOD PRESSURE 140 OR HIGHER or 90 OR HIGHER mercury (mm Hg). (HYPERTENSION) STAGE 2 High blood pressure (HBP) means HYPERTENSIVE the pressure in your arteries is higher CRISIS HIGHER THAN 180 and/ HIGHER THAN 120 than it should be. Another name for (consult your doctor or immediately) high blood pressure is hypertension. Blood pressure is written as two numbers, such as 112/78 mm Hg. The top, or larger, number (called Am I at higher risk of developing HBP? systolic pressure) is the pressure when the heart There are risk factors that increase your chances of developing HBP. Some you can control, and some you can’t. beats. The bottom, or smaller, number (called diastolic pressure) is the pressure when the heart Those that can be controlled are: rests between beats. • Cigarette smoking and exposure to secondhand smoke • Diabetes Normal blood pressure is below 120/80 mm Hg. • Being obese or overweight If you’re an adult and your systolic pressure is 120 to • High cholesterol 129, and your diastolic pressure is less than 80, you have elevated blood pressure. High blood pressure • Unhealthy diet (high in sodium, low in potassium, and drinking too much alcohol) is a systolic pressure of 130 or higher,or a diastolic pressure of 80 or higher, that stays high over time. -

A Review of the Stroke Volume Response to Upright Exercise in Healthy Subjects
190 Br J Sports Med: first published as 10.1136/bjsm.2004.013037 on 25 March 2005. Downloaded from REVIEW A review of the stroke volume response to upright exercise in healthy subjects C A Vella, R A Robergs ............................................................................................................................... Br J Sports Med 2005;39:190–195. doi: 10.1136/bjsm.2004.013037 Traditionally, it has been accepted that, during incremental well trained athletes (subject sex was not stated). Unfortunately, these findings were exercise, stroke volume plateaus at 40% of VO2MAX. largely ignored and it became accepted that However, recent research has documented that stroke stroke volume plateaus during exercise of increasing intensity. volume progressively increases to VO2MAX in both trained More recent investigations have reported that and untrained subjects. The stroke volume response to stroke volume progressively increases in certain 7–12 incremental exercise to VO2MAX may be influenced by people. The mechanisms for the continual training status, age, and sex. For endurance trained increase in stroke volume are not completely understood. Gledhill et al7 proposed that subjects, the proposed mechanisms for the progressive enhanced diastolic filling and subsequent increase in stroke volume to VO2MAX are enhanced diastolic enhanced contractility are responsible for the filling, enhanced contractility, larger blood volume, and increased stroke volume in trained subjects. However, an increase in stroke volume with an decreased cardiac afterload. For untrained subjects, it has increase in exercise intensity has also been been proposed that continued increases in stroke volume reported in untrained subjects.89Table 1 presents may result from a naturally occurring high blood volume. a summary of the past research that has quantified stroke volume during exercise. -

Arteries to Arterioles
• arteries to arterioles Important: The highest pressure of circulating blood is found in arteries, and gradu- ally drops as the blood flows through the arterioles, capillaries, venules, and veins (where it is the lowest). The greatest drop in blood pressure occurs at the transition from arteries to arterioles. Arterioles are one of the blood vessels of the smallest branch of the arterial circula- tion. Blood flowing from the heart is pumped by the left ventricle to the aorta (largest artery), which in turn branches into smaller arteries and finally into arterioles. The blood continues to flow through these arterioles into capillaries, venules, and finally veins, which return the blood to the heart. Arterioles have a very small diameter (<0.5 mm), a small lumen, and a relatively thick tunica media that is composed almost entirely of smooth muscle, with little elastic tissue. This smooth muscle constricts and dilates in response to neurochemical stimuli, which in turn changes the diameter of the arterioles. This causes profound and rapid changes in peripheral resistance. This change in diameter of the arteri- oles regulates the flow of blood into the capillaries. Note: By affecting peripheral resistance, arterioles directly affect arterial blood pressure. Primary function of each type of blood vessel: - Arteries - transport blood away from the heart, generally have blood that is rich in oxygen - Arterioles - control blood pressure - Capillaries - diffusion of nutrients/oxygen - Veins - carry blood back to the heart, generally have blood that is low in oxygen. -

Effects of Vasodilation and Arterial Resistance on Cardiac Output Aliya Siddiqui Department of Biotechnology, Chaitanya P.G
& Experim l e ca n i t in a l l C Aliya, J Clinic Experiment Cardiol 2011, 2:11 C f a Journal of Clinical & Experimental o r d l DOI: 10.4172/2155-9880.1000170 i a o n l o r g u y o J Cardiology ISSN: 2155-9880 Review Article Open Access Effects of Vasodilation and Arterial Resistance on Cardiac Output Aliya Siddiqui Department of Biotechnology, Chaitanya P.G. College, Kakatiya University, Warangal, India Abstract Heart is one of the most important organs present in human body which pumps blood throughout the body using blood vessels. With each heartbeat, blood is sent throughout the body, carrying oxygen and nutrients to all the cells in body. The cardiac cycle is the sequence of events that occurs when the heart beats. Blood pressure is maximum during systole, when the heart is pushing and minimum during diastole, when the heart is relaxed. Vasodilation caused by relaxation of smooth muscle cells in arteries causes an increase in blood flow. When blood vessels dilate, the blood flow is increased due to a decrease in vascular resistance. Therefore, dilation of arteries and arterioles leads to an immediate decrease in arterial blood pressure and heart rate. Cardiac output is the amount of blood ejected by the left ventricle in one minute. Cardiac output (CO) is the volume of blood being pumped by the heart, by left ventricle in the time interval of one minute. The effects of vasodilation, how the blood quantity increases and decreases along with the blood flow and the arterial blood flow and resistance on cardiac output is discussed in this reviewArticle.