Spectrum Analysis of Inborn Errors of Metabolism for Expanded Newborn
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cystinosis, Has Been Reported Previomly in 3 Patients Using (1
, PKU GENE - WSSIBLE CAUSE OF NON-SPECIFIC UENTAL RE- RARE PHENOTYPES OF PLACENTAL ALKALINE PHOSPHATASE: AN 523 TARDATION. Atsuko Fujimoto and Samuel P. Bes-n, ANALYSIS OF RELATIONSHIPS WITH SOME NEONATAL AND b USC Hed. Sch., Dept. Pediatrics, Los Angeles MATERNAL VARIABLES. F. Gloria-Bottini, A. Polzonetti, The Justification Hypothesis (J. Ped. 81:834, 1972) proposes . Bentivoglia, P. Lucarelli and E. Bottini (Spon. by C.D. Cook). that deficiencies in non-essential amino acids might cause mental Jniv. of Camerino, Dept. of Genetics and Computer Center and retardation. The mother heterozygous for synthesis of any one of Jniv. of Rome, Dept. of Pediatrics. the non-essential amino acids would deprive her fetus partially The large number (>15) and frequency (-2%) of rare placental and the heterozygous or homozygous fetus would be more or less alkaline phosphatase (PI) alleles represent a very special case unable to make up for the deficiency. Berman and Ford (Lancet i: among polymorphic enzymes. Since the PI gene is active only dur- 767, 1977) showed that such concatenation of heterozygous mother ing intrauterine life, the allelic diversity and its maintenance and heterozygous fetus is associated with significantly lower IQ. nay be connected with intrauterine environment and with fetal Our own wark has verified this finding. The possibility that development. 1700 newborn infants ( 1271 Caucasians, 337 Negroes heterozygosity for PKU in mother and fetus might be a cause of a and 92 Puerto Ricans), collected at Yale-New Haven Hospital from 1arq.e amount of "non-specific" mental retardation was tested by 1968-1971, were studied. An analysis of the relationship between looking for associated heterozygosity for PKU in mother and child rare PI phenotype and the following 14variableswas carried out: among.12 families in a genetic clinic. -

Effect of Propionic Acid on Fatty Acid Oxidation and U Reagenesis
Pediat. Res. 10: 683- 686 (1976) Fatty degeneration propionic acid hyperammonemia propionic acidemia liver ureagenesls Effect of Propionic Acid on Fatty Acid Oxidation and U reagenesis ALLEN M. GLASGOW(23) AND H. PET ER C HASE UniversilY of Colorado Medical Celller, B. F. SlOlillsky LaboralOries , Denver, Colorado, USA Extract phosphate-buffered salin e, harvested with a brief treatment wi th tryps in- EDTA, washed twice with ph os ph ate-buffered saline, and Propionic acid significantly inhibited "CO z production from then suspended in ph os ph ate-buffe red saline (145 m M N a, 4.15 [I-"ejpalmitate at a concentration of 10 11 M in control fibroblasts m M K, 140 m M c/, 9.36 m M PO" pH 7.4) . I n mos t cases the cells and 100 11M in methyl malonic fibroblasts. This inhibition was we re incubated in 3 ml phosph ate-bu ffered sa lin e cont aining 0.5 similar to that produced by 4-pentenoic acid. Methylmalonic acid I1Ci ll-I4Cj palm it ate (19), final concentration approximately 3 11M also inhibited ' 'C0 2 production from [V 'ejpalmitate, but only at a added in 10 II I hexane. Increasing the amount of hexane to 100 II I concentration of I mM in control cells and 5 mM in methyl malonic did not impair palmit ate ox id ation. In two experiments (Fig. 3) the cells. fibroblasts were in cub ated in 3 ml calcium-free Krebs-Ringer Propionic acid (5 mM) also inhibited ureagenesis in rat liver phosphate buffer (2) co nt ain in g 5 g/ 100 ml essent iall y fatty ac id slices when ammonia was the substrate but not with aspartate and free bovine se rum albumin (20), I mM pa lm itate, and the same citrulline as substrates. -

Propionic Acidemia Information for Health Professionals
Propionic Acidemia Information for Health Professionals Propionic acidemia is an organic acid disorder in which individuals are lacking or have reduced activity of the enzyme propionyl-CoA carboxylase, leading to propionic acidemia. Clinical Symptoms Symptoms generally begin in the first few days following birth. Metabolic crisis can occur, particularly after fasting, periods of illness/infection, high protein intake, or during periods of stress on the body. Symptoms of a metabolic crisis include lethargy, behavior changes, feeding problems, hypotonia, and vomiting. If untreated, metabolic crises can lead to tachypnea, brain swelling, cardiomyopathy, seizures, coma, basal ganglia stroke, and death. Many babies die within the first year of life. Lab findings during a metabolic crisis commonly include urine ketones, hyperammonemia, metabolic acidosis, low platelets, low white blood cells, and high blood ammonia and glycine levels. Long term effects may occur despite treatment and include developmental delay, brain damage, dystonia, failure to thrive, short stature, spasticity, pancreatitis, osteoporosis, and skin lesions. Incidence Propionic acidemia occurs in greater than 1 in 75,000 live births and is more common in Saudi Arabians and the Inuit population of Greenland. Genetics of propionic acidemia Mutations in the PCCA and PCCB genes cause propionic acidemia. Mutations prevent the production of or reduce the activity of propionyl-CoA carboxylase, which converts propionyl-CoA to methylmalonyl-CoA. This causes the body to be unable to correctly process isoleucine, valine, methionine, and threonine, resulting in an accumulation of glycine and propionic acid, which causes the symptoms seen in this condition. How do people inherit propionic acidemia? Propionic acidemia is inherited in an autosomal recessive manner. -
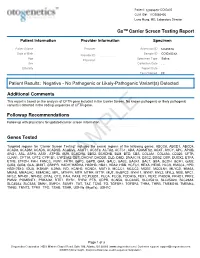
PDF Document Created by Pdffiller
Patient: 1234567843314948-COtGx0053 CLIA ID#: 11D2066426 Larry Hung, MD, Laboratory Director GxTM Carrier Screen Testing Report Patient Information Provider Information Specimen Patient Name Haley Papevies Provider Harbin Clinic Women's Accession ID 1234567843314948 Center Cartersville Date of Birth Apr 16, 1998 Sample ID COtGx0053XX Provider ID 1124488556 Age 19 Specimen Type Saliva Physician Vicki Yates Sex female Collection Date Jul 20, 2017 Ethnicity Report Date Aug 5, 2017 Test Ordered CF Patient Results: Negative - No Pathogenic or Likely-Pathogenic Variant(s) Detected Additional Comments This report is based on the analysis of CFTR gene included in the Carrier Screen. No known pathogenic or likely pathogenic variant(s) detected in the coding sequences of CFTR gene. Followup Recommendations Follow up with physicians for updated carrier screen information. The sequencing for CFTR gene was carried out with the other genes included in the Carrier Screen Testing (listed below). The analysis of the other genes in the Carrier Screen could be ordered through your physicians. Genes Tested Targeted regions for “Carrier Screen Testing” includes the exonic regions of the following genes: ABCC8, ABCD1, ABCD4, ACAD8, ACADM, ACADS, ACADSB, ACADVL, ACAT1, ACSF3, ACTA2, ACTC1, ADA, ADAMTS2, AGXT, AHCY, APC, APOB, ARG1, ASL, ASPA, ASS1, ATP7B, AUH, BCKDHA, BBS2, BCKDHB, BLM, BTD, CBS, COL3A1, COL4A3, CD320, CFTR, CLRN1, CPT1A, CPT2, CYP1B1, CYP21A2, DBT, DHCR7, DHDDS, DLD, DMD, DNAJC19, DSC2, DSG2, DSP, DUOX2, ETFA, ETFB, ETFDH, FAH, FANCC, FBN1, -

Supplement 1 Overview of Dystonia Genes
Supplement 1 Overview of genes that may cause dystonia in children and adolescents Gene (OMIM) Disease name/phenotype Mode of inheritance 1: (Formerly called) Primary dystonias (DYTs): TOR1A (605204) DYT1: Early-onset generalized AD primary torsion dystonia (PTD) TUBB4A (602662) DYT4: Whispering dystonia AD GCH1 (600225) DYT5: GTP-cyclohydrolase 1 AD deficiency THAP1 (609520) DYT6: Adolescent onset torsion AD dystonia, mixed type PNKD/MR1 (609023) DYT8: Paroxysmal non- AD kinesigenic dyskinesia SLC2A1 (138140) DYT9/18: Paroxysmal choreoathetosis with episodic AD ataxia and spasticity/GLUT1 deficiency syndrome-1 PRRT2 (614386) DYT10: Paroxysmal kinesigenic AD dyskinesia SGCE (604149) DYT11: Myoclonus-dystonia AD ATP1A3 (182350) DYT12: Rapid-onset dystonia AD parkinsonism PRKRA (603424) DYT16: Young-onset dystonia AR parkinsonism ANO3 (610110) DYT24: Primary focal dystonia AD GNAL (139312) DYT25: Primary torsion dystonia AD 2: Inborn errors of metabolism: GCDH (608801) Glutaric aciduria type 1 AR PCCA (232000) Propionic aciduria AR PCCB (232050) Propionic aciduria AR MUT (609058) Methylmalonic aciduria AR MMAA (607481) Cobalamin A deficiency AR MMAB (607568) Cobalamin B deficiency AR MMACHC (609831) Cobalamin C deficiency AR C2orf25 (611935) Cobalamin D deficiency AR MTRR (602568) Cobalamin E deficiency AR LMBRD1 (612625) Cobalamin F deficiency AR MTR (156570) Cobalamin G deficiency AR CBS (613381) Homocysteinuria AR PCBD (126090) Hyperphelaninemia variant D AR TH (191290) Tyrosine hydroxylase deficiency AR SPR (182125) Sepiaterine reductase -

Newborn Screening Laboratory Manual of Services
Newborn Screening Laboratory Manual of Services Test Panel: Please see the following links for a detailed description of testing in the Newborn Screening section. Information about the Newborn Screening program is available here. Endocrine Disorders Congenital adrenal hyperplasia (CAH) Congenital hypothyroidism (TSH) Hemoglobinopathies Sickle cell disease (FS) Alpha (Barts) Sickle βeta Thalassemia (FSA) Other sickling hemoglobinopathies such as: FAS FAC FAD FAE Homozygous conditions such as: FC FD FE Metabolic Disorders Biotinidase deficiency Galactosemia Cystic fibrosis (CF) first tier screening for elevated immunoreactive trypsinogen (IRT) Cystic fibrosis second tier genetic mutation analysis on the top 4% IRT concentrations. Current alleles detected : F508del, I507del, G542X, G85E, R117H, 621+1G->T, 711+1G->T, R334W, R347P, A455E, 1717-1G->A, R560T, R553X, G551D, 1898+1G->A, 2184delA, 2789+5G->A, 3120+1G->A, R1162X, 3659delC, 3849+10kbC->T, W1282X, N1303K, IVS polyT T5/T7/T9 *Currently validating a mutation panel that includes the above alleles in addition to the following: 1078delT, Y122X, 394delTT, R347H, M1101K, S1255X, 1898+5G->T, 2183AA->G, 2307insA, Y1092X, 3876delA, 3905insT, S549N, S549R_1645A->C, S549R-1647T->G, S549R-1647T->G, V520F, A559T, 1677delTA, 2055del9->A, 2143delT, 3199del6, 406-1G->A, 935delA, D1152H, CFTRdele2, E60X, G178R, G330X, K710X, L206W, Q493X, Q890X, R1066C, R1158X, R75X, S1196X, W1089X, G1244E, G1349D, G551S, R560KT, S1251N, S1255P Amino acid disorders Phenylketonuria (PKU) / Hyperphenylalaninemia Maple -

Incidence of Inborn Errors of Metabolism by Expanded Newborn
Original Article Journal of Inborn Errors of Metabolism & Screening 2016, Volume 4: 1–8 Incidence of Inborn Errors of Metabolism ª The Author(s) 2016 DOI: 10.1177/2326409816669027 by Expanded Newborn Screening iem.sagepub.com in a Mexican Hospital Consuelo Cantu´-Reyna, MD1,2, Luis Manuel Zepeda, MD1,2, Rene´ Montemayor, MD3, Santiago Benavides, MD3, Hector´ Javier Gonza´lez, MD3, Mercedes Va´zquez-Cantu´,BS1,4, and Hector´ Cruz-Camino, BS1,5 Abstract Newborn screening for the detection of inborn errors of metabolism (IEM), endocrinopathies, hemoglobinopathies, and other disorders is a public health initiative aimed at identifying specific diseases in a timely manner. Mexico initiated newborn screening in 1973, but the national incidence of this group of diseases is unknown or uncertain due to the lack of large sample sizes of expanded newborn screening (ENS) programs and lack of related publications. The incidence of a specific group of IEM, endocrinopathies, hemoglobinopathies, and other disorders in newborns was obtained from a Mexican hospital. These newborns were part of a comprehensive ENS program at Ginequito (a private hospital in Mexico), from January 2012 to August 2014. The retrospective study included the examination of 10 000 newborns’ results obtained from the ENS program (comprising the possible detection of more than 50 screened disorders). The findings were the following: 34 newborns were confirmed with an IEM, endocrinopathies, hemoglobinopathies, or other disorders and 68 were identified as carriers. Consequently, the estimated global incidence for those disorders was 3.4 in 1000 newborns; and the carrier prevalence was 6.8 in 1000. Moreover, a 0.04% false-positive rate was unveiled as soon as diagnostic testing revealed negative results. -

Downloaded from GEO
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.17.252007; this version posted November 3, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Oxylipin metabolism is controlled by mitochondrial b-oxidation during bacterial inflammation. Mariya Misheva1, Konstantinos Kotzamanis1*, Luke C Davies1*, Victoria J Tyrrell1, Patricia R S Rodrigues1, Gloria A Benavides2, Christine Hinz1, Robert C Murphy3, Paul Kennedy4, Philip R Taylor1,5, Marcela Rosas1, Simon A Jones1, Sumukh Deshpande1, Robert Andrews1, Magdalena A Czubala1, Mark Gurney1, Maceler Aldrovandi1, Sven W Meckelmann1, Peter Ghazal1, Victor Darley-Usmar2, Daniel White1, and Valerie B O’Donnell1 1Systems Immunity Research Institute and Division of Infection and Immunity, and School of Medicine, Cardiff University, UK, 2Department of Pathology, University of Alabama at Birmingham, Birmingham, AL 35294, USA, 3Department of Pharmacology, University of Colorado Denver, Aurora, CO 80045, USA, 4Cayman Chemical 1180 E Ellsworth Rd, Ann Arbor, MI 48108, United States, 5UK Dementia Research Institute at Cardiff, Cardiff University, UK Address correspondence: Valerie O’Donnell, [email protected] or Daniel White, [email protected], Systems Immunity Research Institute, Cardiff University *Both authors contributed equally to the study 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.17.252007; this version posted November 3, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. -

Neurodevelopmental Signatures of Narcotic and Neuropsychiatric Risk Factors in 3D Human-Derived Forebrain Organoids
Molecular Psychiatry www.nature.com/mp ARTICLE OPEN Neurodevelopmental signatures of narcotic and neuropsychiatric risk factors in 3D human-derived forebrain organoids 1 1 1 1 2 2 3 Michael Notaras , Aiman Lodhi , Estibaliz✉ Barrio-Alonso , Careen Foord , Tori Rodrick , Drew Jones , Haoyun Fang , David Greening 3,4 and Dilek Colak 1,5 © The Author(s) 2021 It is widely accepted that narcotic use during pregnancy and specific environmental factors (e.g., maternal immune activation and chronic stress) may increase risk of neuropsychiatric illness in offspring. However, little progress has been made in defining human- specific in utero neurodevelopmental pathology due to ethical and technical challenges associated with accessing human prenatal brain tissue. Here we utilized human induced pluripotent stem cells (hiPSCs) to generate reproducible organoids that recapitulate dorsal forebrain development including early corticogenesis. We systemically exposed organoid samples to chemically defined “enviromimetic” compounds to examine the developmental effects of various narcotic and neuropsychiatric-related risk factors within tissue of human origin. In tandem experiments conducted in parallel, we modeled exposure to opiates (μ-opioid agonist endomorphin), cannabinoids (WIN 55,212-2), alcohol (ethanol), smoking (nicotine), chronic stress (human cortisol), and maternal immune activation (human Interleukin-17a; IL17a). Human-derived dorsal forebrain organoids were consequently analyzed via an array of unbiased and high-throughput analytical approaches, including state-of-the-art TMT-16plex liquid chromatography/mass- spectrometry (LC/MS) proteomics, hybrid MS metabolomics, and flow cytometry panels to determine cell-cycle dynamics and rates of cell death. This pipeline subsequently revealed both common and unique proteome, reactome, and metabolome alterations as a consequence of enviromimetic modeling of narcotic use and neuropsychiatric-related risk factors in tissue of human origin. -

Abstracts from the 9Th Biennial Scientific Meeting of The
International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):15 DOI 10.1186/s13633-017-0054-x MEETING ABSTRACTS Open Access Abstracts from the 9th Biennial Scientific Meeting of the Asia Pacific Paediatric Endocrine Society (APPES) and the 50th Annual Meeting of the Japanese Society for Pediatric Endocrinology (JSPE) Tokyo, Japan. 17-20 November 2016 Published: 28 Dec 2017 PS1 Heritable forms of primary bone fragility in children typically lead to Fat fate and disease - from science to global policy a clinical diagnosis of either osteogenesis imperfecta (OI) or juvenile Peter Gluckman osteoporosis (JO). OI is usually caused by dominant mutations affect- Office of Chief Science Advsor to the Prime Minister ing one of the two genes that code for two collagen type I, but a re- International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):PS1 cessive form of OI is present in 5-10% of individuals with a clinical diagnosis of OI. Most of the involved genes code for proteins that Attempts to deal with the obesity epidemic based solely on adult be- play a role in the processing of collagen type I protein (BMP1, havioural change have been rather disappointing. Indeed the evidence CREB3L1, CRTAP, LEPRE1, P4HB, PPIB, FKBP10, PLOD2, SERPINF1, that biological, developmental and contextual factors are operating SERPINH1, SEC24D, SPARC, from the earliest stages in development and indeed across generations TMEM38B), or interfere with osteoblast function (SP7, WNT1). Specific is compelling. The marked individual differences in the sensitivity to the phenotypes are caused by mutations in SERPINF1 (recessive OI type obesogenic environment need to be understood at both the individual VI), P4HB (Cole-Carpenter syndrome) and SEC24D (‘Cole-Carpenter and population level. -

Mechanistic Studies on Medium Chain Acyl-Coa Dehydrogenase
Acyl-CoA Dehydrogenases: Mechanistic studies on Medium Chain Acyl-CoA Dehydrogenase Dissertation zur Erlangung des akademischen Grades des Doktors der Naturwissenschaften (Dr. rer. nat.) an der Universität Konstanz (Fachbereich Biologie) vorgelegt von Vasile Robert Gradinaru Konstanz, im Juni 2005 Tag der mündlichen Prüfung : 9. November 2005 Referent: Prof. Dr. Sandro Ghisla Referent: Prof. Dr. Peter Macheroux Acknowledgements I am greatly indebted to my supervisor, Prof. Dr. Sandro Ghisla, for his advice and support. He has been an excellent supervisor providing insightful comments and constructive criticism throughout this PhD project. I would also like to thank my colleagues in the Universities of Konstanz and Iasi for their advice, encouragement and friendship, without which I would certainly not have completed this thesis. In particular, I would like to thank Prof. Dr. Richard Schowen, Prof. Dr. Peter Macheroux, Prof. Dr. Colin Thorpe, Prof. Dr. Jung-Ja. Kim, Prof. Dr. Tatiana Nicolaescu, Prof. Dr. Constantin Ciugureanu, Prof. Dr. Robert Bach, Dr. Olga Dmitrenko, Susanne Feindler-Boeckh, Gudrun Vogt, Elmi Leisner, Karl Janko, Lili Smau, Nasser Ibrahim, Phaneeswara Rao Kommoju, Sudarshan Rao Ande, Lakshminarayana Kaza, Cosmin Pocanschi, Paula Bulieris for their active interest during the course of this project. My gratitude also goes to Prof. Alexandru Cecal for encouraging me to embark on this PhD. I express my loving thanks to my wife Luiza whose love, support, patience and understanding made this work easier. Above all, I wish to express my sincerest gratitude to my parents, who made my studies possible and who have always encouraged me. This study was financiarlly supported by the Deutsche Forschungsgemeinschaft (Gh 2/6-4). -
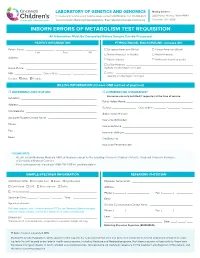
Inborn Errors of Metabolism Test Requisition
LABORATORY OF GENETICS AND GENOMICS Mailing Address: For local courier service and/or inquiries, please contact 513-636-4474 • Fax: 513-636-4373 3333 Burnet Avenue, Room R1042 www.cincinnatichildrens.org/moleculargenetics • Email: [email protected] Cincinnati, OH 45229 INBORN ERRORS OF METABOLISM TEST REQUISITION All Information Must Be Completed Before Sample Can Be Processed PATIENT INFORMATION ETHNIC/RACIAL BACKGROUND (Choose All) Patient Name: ___________________ , ___________________ , ________ European American (White) African-American (Black) Last First MI Native American or Alaskan Asian-American Address: ____________________________________________________ Pacific Islander Ashkenazi Jewish ancestry ____________________________________________________ Latino-Hispanic _____________________________________________ Home Phone: ________________________________________________ (specify country/region of origin) MR# __________________ Date of Birth ________ / ________ / _______ Other ____________________________________________________ (specify country/region of origin) Gender: Male Female BILLING INFORMATION (Choose ONE method of payment) o REFERRING INSTITUTION o COMMERCIAL INSURANCE* Insurance can only be billed if requested at the time of service. Institution: ____________________________________________________ Policy Holder Name: _____________________________________________ Address: _____________________________________________________ Gender: ________________ Date of Birth ________ / ________ / _______