Red‐Bellied Black Snake (Pseudechis Porphyriacus)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Phylogeny of the Black Snakes (Pseudechis: Elapidae: Serpentes
1 Multi-locus phylogeny and species delimitation of Australo-Papuan blacksnakes 2 (Pseudechis Wagler, 1830: Elapidae: Serpentes) 3 4 Simon T. Maddock 1,2,3,4,*, Aaron Childerstone 3, Bryan Grieg Fry 5, David J. Williams 5 6,7, Axel Barlow 3,8, Wolfgang Wüster 3 6 7 1 Department of Life Sciences, The Natural History Museum, London, SW7 5BD, UK. 8 2 Department of Genetics, Evolution and Environment, University College London, 9 London, WC1E 6BT, UK. 10 3 School of Biological Sciences, Environment Centre Wales, Bangor University, Bangor, 11 LL57 2UW, United Kingdom. 12 4 Department of Animal Management, Reaseheath, College, Nantwich, Cheshire, CW5 13 6DF, UK. 14 5 Venom Evolution Lab, School of Biological Sciences, University of Queensland, St 15 Lucia QLD, 4072 Australia. 16 6 Australian Venom Research Unit, Department of Pharmacology, University of 17 Melbourne, Parkville, Vic, 3010, Australia. 18 7 School of Medicine & Health Sciences, University of Papua New Guinea, Boroko, 19 NCD, 121, Papua New Guinea. 20 8 Institute for Biochemistry and Biology, University of Potsdam, 14476 Potsdam (Golm), 21 Germany. 22 23 * corresponding author: [email protected] 24 25 Abstract 26 Genetic analyses of Australasian organisms have resulted in the identification of 27 extensive cryptic diversity across the continent. The venomous elapid snakes are among 28 the best-studied organismal groups in this region, but many knowledge gaps persist: for 29 instance, despite their iconic status, the species-level diversity among Australo-Papuan 30 blacksnakes (Pseudechis) has remained poorly understood due to the existence of a group 31 of cryptic species within the P. -

Neurotoxic Effects of Venoms from Seven Species of Australasian Black Snakes (Pseudechis): Efficacy of Black and Tiger Snake Antivenoms
Clinical and Experimental Pharmacology and Physiology (2005) 32, 7–12 NEUROTOXIC EFFECTS OF VENOMS FROM SEVEN SPECIES OF AUSTRALASIAN BLACK SNAKES (PSEUDECHIS): EFFICACY OF BLACK AND TIGER SNAKE ANTIVENOMS Sharmaine Ramasamy,* Bryan G Fry† and Wayne C Hodgson* *Monash Venom Group, Department of Pharmacology, Monash University, Clayton and †Australian Venom Research Unit, Department of Pharmacology, University of Melbourne, Parkville, Victoria, Australia SUMMARY the sole clad of venomous snakes capable of inflicting bites of medical importance in the region.1–3 The Pseudechis genus (black 1. Pseudechis species (black snakes) are among the most snakes) is one of the most widespread, occupying temperate, widespread venomous snakes in Australia. Despite this, very desert and tropical habitats and ranging in size from 1 to 3 m. little is known about the potency of their venoms or the efficacy Pseudechis australis is one of the largest venomous snakes found of the antivenoms used to treat systemic envenomation by these in Australia and is responsible for the vast majority of black snake snakes. The present study investigated the in vitro neurotoxicity envenomations. As such, the venom of P. australis has been the of venoms from seven Australasian Pseudechis species and most extensively studied and is used in the production of black determined the efficacy of black and tiger snake antivenoms snake antivenom. It has been documented that a number of other against this activity. Pseudechis from the Australasian region can cause lethal 2. All venoms (10 g/mL) significantly inhibited indirect envenomation.4 twitches of the chick biventer cervicis nerve–muscle prepar- The envenomation syndrome produced by Pseudechis species ation and responses to exogenous acetylcholine (ACh; varies across the genus and is difficult to characterize because the 1 mmol/L), but not to KCl (40 mmol/L), indicating activity at offending snake is often not identified.3,5 However, symptoms of post-synaptic nicotinic receptors on the skeletal muscle. -
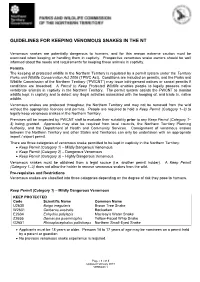
Guidelines for Keeping Venomous Snakes in the NT
GUIDELINES FOR KEEPING VENOMOUS SNAKES IN THE NT Venomous snakes are potentially dangerous to humans, and for this reason extreme caution must be exercised when keeping or handling them in captivity. Prospective venomous snake owners should be well informed about the needs and requirements for keeping these animals in captivity. Permits The keeping of protected wildlife in the Northern Territory is regulated by a permit system under the Territory Parks and Wildlife Conservation Act 2006 (TPWC Act). Conditions are included on permits, and the Parks and Wildlife Commission of the Northern Territory (“PWCNT”) may issue infringement notices or cancel permits if conditions are breached. A Permit to Keep Protected Wildlife enables people to legally possess native vertebrate animals in captivity in the Northern Territory. The permit system assists the PWCNT to monitor wildlife kept in captivity and to detect any illegal activities associated with the keeping of, and trade in, native wildlife. Venomous snakes are protected throughout the Northern Territory and may not be removed from the wild without the appropriate licences and permits. People are required to hold a Keep Permit (Category 1–3) to legally keep venomous snakes in the Northern Territory. Premises will be inspected by PWCNT staff to evaluate their suitability prior to any Keep Permit (Category 1– 3) being granted. Approvals may also be required from local councils, the Northern Territory Planning Authority, and the Department of Health and Community Services. Consignment of venomous snakes between the Northern Territory and other States and Territories can only be undertaken with an appropriate import / export permit. There are three categories of venomous snake permitted to be kept in captivity in the Northern Territory: Keep Permit (Category 1) – Mildly Dangerous Venomous Keep Permit (Category 2) – Dangerous Venomous Keep Permit (Category 3) – Highly Dangerous Venomous Venomous snakes must be obtained from a legal source (i.e. -
Draft Animal Keepers Species List
Revised NSW Native Animal Keepers’ Species List Draft © 2017 State of NSW and Office of Environment and Heritage With the exception of photographs, the State of NSW and Office of Environment and Heritage are pleased to allow this material to be reproduced in whole or in part for educational and non-commercial use, provided the meaning is unchanged and its source, publisher and authorship are acknowledged. Specific permission is required for the reproduction of photographs. The Office of Environment and Heritage (OEH) has compiled this report in good faith, exercising all due care and attention. No representation is made about the accuracy, completeness or suitability of the information in this publication for any particular purpose. OEH shall not be liable for any damage which may occur to any person or organisation taking action or not on the basis of this publication. Readers should seek appropriate advice when applying the information to their specific needs. All content in this publication is owned by OEH and is protected by Crown Copyright, unless credited otherwise. It is licensed under the Creative Commons Attribution 4.0 International (CC BY 4.0), subject to the exemptions contained in the licence. The legal code for the licence is available at Creative Commons. OEH asserts the right to be attributed as author of the original material in the following manner: © State of New South Wales and Office of Environment and Heritage 2017. Published by: Office of Environment and Heritage 59 Goulburn Street, Sydney NSW 2000 PO Box A290, -

Demansia Papuensis)
Clinical and Experimental Pharmacology and Physiology (2006) 33, 364–368 Blackwell Publishing Ltd NeuromuscularSOriginal Kuruppu ArticleIN et al. effects of D. papuensisVITRO venom NEUROTOXIC AND MYOTOXIC EFFECTS OF THE VENOM FROM THE BLACK WHIP SNAKE (DEMANSIA PAPUENSIS) S Kuruppu,* Bryan G Fry† and Wayne C Hodgson* *Monash Venom Group, Department of Pharmacology, Monash University and †Australian Venom Research Unit, Department of Pharmacology, University of Melbourne, Melbourne, Victoria, Australia SUMMARY of Australian snakes whose venoms have not been pharmacologically characterized. Whip snakes (D. papuensis and D. atra, also called 1. Black whip snakes belong to the family elapidae and are D. vestigata) belong to the family elapidae and are found throughout found throughout the northern coastal region of Australia. The the northern coastal region of Australia.3 The black whip snake black whip snake (Demansia papuensis) is considered to be poten- (D. papuensis) is considered to be potentially dangerous due to its tially dangerous due to its size and phylogenetic distinctiveness. size (up to 2 m) and phylogenetic distinctiveness which may suggest Previous liquid chromatography–mass spectrometry analysis of the presence of unique venom components.2 LC-MS analysis of D. papuensis venom indicated a number of components within D. papuensis venom indicated a number of components within the the molecular mass ranges compatible with neurotoxins. For the molecular mass ranges of 6–7 and 13–14 kDa.4 This may indicate the first time, this study examines the in vitro neurotoxic and myotoxic presence of short and long chain a-neurotoxins or PLA2 components, effects of the venom from D. -

Venemous Snakes
WASAH WESTERN AUSTRALIAN SOCIETY of AMATEUR HERPETOLOGISTS (Inc) K E E P I N G A D V I C E S H E E T Venomous Snakes Southern Death Adder (Acanthophis Southern Death antarcticus) – Maximum length 100 cm. Adder Category 5. Desert Death Adder (Acanthophis pyrrhus) – Acanthophis antarcticus Maximum length 75 cm. Category 5. Pilbara Death Adder (Acanthophis wellsi) – Maximum length 70 cm. Category 5. Western Tiger Snake (Notechis scutatus) - Maximum length 160 cm. Category 5. Mulga Snake (Pseudechis australis) – Maximum length 300 cm. Category 5. Spotted Mulga Snake (Pseudechis butleri) – Maximum length 180 cm. Category 5. Dugite (Pseudonaja affinis affinis) – Maximum Desert Death Adder length 180 cm. Category 5. Acanthophis pyrrhus Gwardar (Pseudonaja nuchalis) – Maximum length 100 cm. Category 5. NOTE: All species listed here are dangerously venomous and are listed as Category 5. Only the experienced herpetoculturalist should consider keeping any of them. One must be over 18 years of age to hold a category 5 license. Maintaining a large elapid carries with 1 it a considerable responsibility. Unless you are Pilbara Death Adder confident that you can comply with all your obligations and licence requirements when Acanthophis wellsi keeping dangerous animals, then look to obtaining a non-venomous species instead. NATURAL HABITS: Venomous snakes occur in a wide variety of habitats and, apart from death adders, are highly mobile. All species are active day and night. HOUSING: In all species listed except death adders, one adult (to 150 cm total length) can be kept indoors in a lockable, top-ventilated, all glass or glass-fronted wooden vivarium of Western Tiger Snake at least 90 x 45 cm floor area. -

Venom Week VI
Toxicon 150 (2018) 315e334 Contents lists availableHouston, at ScienceDirect TX, respectively. Toxicon journal homepage: www.elsevier.com/locate/toxicon Venom Week VI Texas A&M University, Kingsville, March 14-18, 2018 North American Society of Toxinology Venom Week VII will be held in 2020 at the University of Florida, Gain- Abstract Editors: Daniel E. Keyler, Pharm.D., FAACT and Elda E. Sanchez, esville, Florida, and organized by Drs. Alfred Alequas and Michael Schaer. Ph.D. Venom Week VI was held at Texas A&M University, Kingsville, Texas, and Appreciation is extended to Elsevier and Toxicon for their excellent sup- was sponsored by the North American Society of Toxinology. The meeting port, and to all Texas A&M University, Kingsville staff for their outstanding was attended by 160 individuals, including 14 invited speakers, and rep- contribution and efforts to make Venom Week VI a success. resenting eight different countries including the United States. Dr. Elda E. Sanchez was the meeting Chair along with meeting coordinators Drs. Daniel E. Keyler, University of Minnesota and Steven A. Seifert, University of New Mexico, USA. Abstracts Newly elected NAST officers were announced and welcomed: President, Basic and translational research IN Carl-Wilhelm Vogel MD, PhD; Secretary, Elda E. Sanchez, PhD; and Steven THIRD GENERATION ANTIVENOMICS: PUSHING THE LIMITS OF THE VITRO A. Seifert, Treasurer. PRECLINICAL ASSESSMENT OF ANTIVENOMS * Invited Speakers: D. Pla, Y. Rodríguez, J.J. Calvete . Evolutionary and Translational Venomics Glenn King, PhD, University of Queensland, Australia, Editor-in-Chief, Lab, Biomedicine Institute of Valencia, Spanish Research Council, 46010 Toxicon; Keynote speaker Valencia, Spain Bruno Lomonte, PhD, Instituto Clodomiro Picado, University of Costa Rica * Corresponding author. -

Berriquin LWMP Wildlife
Berriquin Wildlife Murray Land & Water Management Plan Wildlife Survey 2005-2006 Matthew Herring David Webb Michael Pisasale INTRODUCTION Why do a wildlife survey? 106 farms and were surveyed One of the great things about between June 2005 and March living in rural Australia is all the 2006. They incorporated a range wildlife that we share the land- of vegetation types (e.g. Black scape with. Historically, humans Box Woodland) as well as reveg- have impacted on the survival of etation on previously cleared many native plants and animals. land and constructed wetlands. Fortunately, there is a grow- Methods used to survey wildlife ing commitment in the country included: to wildlife conservation on the farm. As we improve our knowl- - Bird surveys edge and understanding of the - Log rolling for reptiles and local landscape and the animals frogs and plants that live in it we will - Spotlighting for mammals, rep be in a much better position to tiles and nocturnal birds conserve and enhance our natu- - Elliot traps for small mammals ral heritage for future genera- and reptiles tions. - Pitfall trapping for reptiles and frogs This wildlife survey was an ini- - Harp traps for bats tiative of the Berriquin Land & - Using the “Anabat” to record Water Management Plan (LWMP) bat calls M.Herring Working Group and is the largest - Call broadcasting to attract Wildlife expert Adam Bester and most extensive ever un- birds with 11 Little Forest Bats, one dertaken in the area. Berriquin of Berriquin’s most abundant was one of four LWMP areas that Other targeted methods were mammals. -

A Taxonomic Framework for Typhlopid Snakes from the Caribbean and Other Regions (Reptilia, Squamata)
caribbean herpetology article A taxonomic framework for typhlopid snakes from the Caribbean and other regions (Reptilia, Squamata) S. Blair Hedges1,*, Angela B. Marion1, Kelly M. Lipp1,2, Julie Marin3,4, and Nicolas Vidal3 1Department of Biology, Pennsylvania State University, University Park, PA 16802-5301, USA. 2Current address: School of Dentistry, University of North Carolina, Chapel Hill, NC 27599-7450, USA. 3Département Systématique et Evolution, UMR 7138, C.P. 26, Muséum National d’Histoire Naturelle, 57 rue Cuvier, F-75231 Paris cedex 05, France. 4Current address: Department of Biology, Pennsylvania State University, University Park, PA 16802-5301 USA. *Corresponding author ([email protected]) Article registration: http://zoobank.org/urn:lsid:zoobank.org:pub:47191405-862B-4FB6-8A28-29AB7E25FBDD Edited by: Robert W. Henderson. Date of publication: 17 January 2014. Citation: Hedges SB, Marion AB, Lipp KM, Marin J, Vidal N. 2014. A taxonomic framework for typhlopid snakes from the Caribbean and other regions (Reptilia, Squamata). Caribbean Herpetology 49:1–61. Abstract The evolutionary history and taxonomy of worm-like snakes (scolecophidians) continues to be refined as new molec- ular data are gathered and analyzed. Here we present additional evidence on the phylogeny of these snakes, from morphological data and 489 new DNA sequences, and propose a new taxonomic framework for the family Typhlopi- dae. Of 257 named species of typhlopid snakes, 92 are now placed in molecular phylogenies along with 60 addition- al species yet to be described. Afrotyphlopinae subfam. nov. is distributed almost exclusively in sub-Saharan Africa and contains three genera: Afrotyphlops, Letheobia, and Rhinotyphlops. Asiatyphlopinae subfam. nov. is distributed in Asia, Australasia, and islands of the western and southern Pacific, and includes ten genera:Acutotyphlops, Anilios, Asiatyphlops gen. -

Taxonomy of the Genus Pseudonaja (Reptilia: Elapidae) in Australia
AUSTRALIAN BIODIVERSITY RECORD ________________________________________________________ 2002 (No 7) ISSN 1325-2992 March, 2002 ________________________________________________________ Taxonomy of the Genus Pseudonaja (Reptilia: Elapidae) in Australia. by Richard W. Wells “Shiralee”, Major West Road, Cowra, New South Wales, Australia The clear morphological differences that exist within the genus as previously considered strongly indicate that it is a polyphyletic assemblage. Accordingly, I have taken the step of formally proposing the fragmentation of Pseudonaja. In this work I have decided to restrict the genus Pseudonaja to the Pseudonaja nuchalis complex. Additionally, I herein formally resurrect from synonymy the generic name Euprepiosoma Fitzinger, 1860 for the textilis group of species, erect a new generic name (Placidaserpens gen. nov.) for the snakes previously regarded as Pseudonaja guttata, erect a new generic name (Notopseudonaja gen. nov.) for the group of species previously regarded as the Pseudonaja modesta complex, and erect a new generic name (Dugitophis gen. nov.) for snakes previously regarded as the Pseudonaja affinis complex. Genus Pseudonaja Gunther, 1858 The Pseudonaja nuchalis Complex It is usually reported that Pseudonaja nuchalis occurs across most of northern, central and western Australia, ranging from Cape York Peninsula, in the north-east, through western, southern and south-eastern Queensland, far western New South Wales, north-western Victoria, and most of South Australia, Northern Territory and Western Australia. However, this distribution pattern is now known to actually represents several different species all regarded by most authorities for convenience as the single highly variable species, 'Pseudonaja nuchalis'. As usually defined, this actually is a highly variable and therefore confusing group of species to identify and it is not all surprising that there has been difficulty in breaking up the group. -

Proteomic and Genomic Characterisation of Venom Proteins from Oxyuranus Species
This file is part of the following reference: Welton, Ronelle Ellen (2005) Proteomic and genomic characterisation of venom proteins from Oxyuranus species. PhD thesis, James Cook University Access to this file is available from: http://eprints.jcu.edu.au/11938 Chapter 1 Introduction and literature review Chapter 1 Introduction and literature review 1.1 INTRODUCTION Animal venoms are an evolutionary adaptation to immobilise and digest prey and are used secondarily as a defence mechanism (Tu and Dekker, 1991). Intriguingly, evolutionary adaptations have produced a variety of venom proteins with specific actions and targets. A cocktail of protein and peptide toxins have varying molecular compositions, and these unique components have evolved for differing species to quickly and specifically target their prey. The compositions of venoms differ, with components varying within the toxins of spiders, stinging fish, jellyfish, octopi, cone shells, ticks, ants and snakes. Toxins have evolved for the varying mode of actions within different organisms, yet many enzymes are common to different venoms including L-amino oxidases, esterases, aminopeptidases, hyaluronidases, triphosphatases, alkaline phosphomonoesterases, 2 2 phospholipases, phosphodiesterases, serine-metalloproteases and Ca +IMg +-activated proteases. The enzymes found in venoms fall into one or more pharmacological groups including those which possess neurotoxic (causing paralysis or interfering with nervous system function), myotoxic (damaging muscle), haemotoxic (affecting the blood, -

Very Venomous, But...- Snakes of the Wet Tropics
No.80 January 2004 Notes from Very venomous but ... the Australia is home to some of the most venomous snakes in the world. Why? Editor It is possible that strong venom may little chance to fight back. There are six main snake families have evolved chiefly as a self-defence in Australia – elapids (venomous strategy. It is interesting to look at the While coastal and inland taipans eat snakes, the largest group), habits of different venomous snakes. only mammals, other venomous colubrids (‘harmless’ snakes) Some, such as the coastal taipan snakes feed largely on reptiles and pythons, blindsnakes, filesnakes (Oxyuranus scutellatus), bite their frogs. Venom acts slowly on these and seasnakes. prey quickly, delivering a large amount ‘cold-blooded’ creatures with slow of venom, and then let go. The strong metabolic rates, so perhaps it needs to Australia is the only continent venom means that the prey doesn’t be especially strong. In addition, as where venomous snakes (70 get far before succumbing so the many prey species develop a degree of percent) outnumber non- snake is able to follow at a safe immunity to snake venom, a form of venomous ones. Despite this, as distance. Taipans eat only mammals – evolutionary arms race may have been the graph on page one illustrates, which are able to bite back, viciously. taking place. very few deaths result from snake This strategy therefore allows the bites. It is estimated that between snake to avoid injury. … not necessarily deadly 50 000 and 60 000 people die of On the other hand, the most Some Australian snakes may be snake bite each year around the particularly venomous, but they are world.