The Evolving Landscape of Therapeutic and Diagnostic Radiopharmaceuticals
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Landscape Analysis of Phase 2/3 Clinical Trials of Targeted
Journal of Nuclear Medicine, published on February 12, 2021 as doi:10.2967/jnumed.120.258103 Landscape analysis of Phase 2/3 clinical trials for Targeted Radionuclide Therapy Erik Mittra1, Amanda Abbott2, and Lisa Bodei3 Affiliations 1. Division of Nuclear Medicine & Molecular Imaging, Oregon Health & Science University, Portland, OR 2. Clinical Trials Network, Society of Nuclear Medicine & Molecular Imaging, Reston, VA 3. Molecular Imaging and Therapy Service, Memorial Sloan Kettering Cancer Center, New York, NY Word count without figure: 880 Word count with figure: 971 Key Words: radioisotope therapy, radiopharmaceutical therapy and radioligand therapy Text Within Nuclear Medicine, theranostics has revitalized the field of Targeted Radionuclide Therapy (TRT) and there is a growing number of investigator-initiated and industry-sponsored clinical trials of TRT. This article summarizes the current trials available in the NIH database, the largest trial repository, to provide both an overview of the current landscape and a glimpse towards an undeniably exciting future of theranostics. This landscape analysis was completed by searching the terms “radionuclide therapy”, “radioisotope therapy”, “radiopharmaceutical therapy” and “radioligand therapy” on ClinicalTrials.gov in November 2020. Other terms may provide different results. Phase 1/2, 2, and 3 trials that are currently recruiting and those not yet recruiting were included. Studies. Overall, the results showed 42 clinical trials including 13 Phase 1/2, 26 Phase 2, and three Phase 3. Given this range of phases, the planned enrollment varies widely from 10-813, with an average of 147 participants. Five different radioisotopes, 12 ligands or targets, and 11 different cancer types are represented (Figure 1). -

OPERATIONAL GUIDANCE on HOSPITAL RADIOPHARMACY: a SAFE and EFFECTIVE APPROACH the Following States Are Members of the International Atomic Energy Agency
OPERATIONAL GUIDANCE ON HOSPITAL RADIOPHARMACY: A SAFE AND EFFECTIVE APPROACH The following States are Members of the International Atomic Energy Agency: AFGHANISTAN GUATEMALA PAKISTAN ALBANIA HAITI PALAU ALGERIA HOLY SEE PANAMA ANGOLA HONDURAS PARAGUAY ARGENTINA HUNGARY PERU ARMENIA ICELAND PHILIPPINES AUSTRALIA INDIA POLAND AUSTRIA INDONESIA PORTUGAL AZERBAIJAN IRAN, ISLAMIC REPUBLIC OF QATAR BANGLADESH IRAQ REPUBLIC OF MOLDOVA BELARUS IRELAND ROMANIA BELGIUM ISRAEL RUSSIAN FEDERATION BELIZE ITALY SAUDI ARABIA BENIN JAMAICA SENEGAL BOLIVIA JAPAN SERBIA BOSNIA AND HERZEGOVINA JORDAN SEYCHELLES BOTSWANA KAZAKHSTAN BRAZIL KENYA SIERRA LEONE BULGARIA KOREA, REPUBLIC OF SINGAPORE BURKINA FASO KUWAIT SLOVAKIA CAMEROON KYRGYZSTAN SLOVENIA CANADA LATVIA SOUTH AFRICA CENTRAL AFRICAN LEBANON SPAIN REPUBLIC LIBERIA SRI LANKA CHAD LIBYAN ARAB JAMAHIRIYA SUDAN CHILE LIECHTENSTEIN SWEDEN CHINA LITHUANIA SWITZERLAND COLOMBIA LUXEMBOURG SYRIAN ARAB REPUBLIC COSTA RICA MADAGASCAR TAJIKISTAN CÔTE D’IVOIRE MALAWI THAILAND CROATIA MALAYSIA THE FORMER YUGOSLAV CUBA MALI REPUBLIC OF MACEDONIA CYPRUS MALTA TUNISIA CZECH REPUBLIC MARSHALL ISLANDS TURKEY DEMOCRATIC REPUBLIC MAURITANIA UGANDA OF THE CONGO MAURITIUS UKRAINE DENMARK MEXICO UNITED ARAB EMIRATES DOMINICAN REPUBLIC MONACO UNITED KINGDOM OF ECUADOR MONGOLIA GREAT BRITAIN AND EGYPT MONTENEGRO NORTHERN IRELAND EL SALVADOR MOROCCO ERITREA MOZAMBIQUE UNITED REPUBLIC ESTONIA MYANMAR OF TANZANIA ETHIOPIA NAMIBIA UNITED STATES OF AMERICA FINLAND NEPAL URUGUAY FRANCE NETHERLANDS UZBEKISTAN GABON NEW ZEALAND VENEZUELA GEORGIA NICARAGUA VIETNAM GERMANY NIGER YEMEN GHANA NIGERIA ZAMBIA GREECE NORWAY ZIMBABWE The Agency’s Statute was approved on 23 October 1956 by the Conference on the Statute of the IAEA held at United Nations Headquarters, New York; it entered into force on 29 July 1957. The Headquarters of the Agency are situated in Vienna. -
Azedra) Reference Number: ERX.SPA.420 Effective Date: 03.01.21 Last Review Date: 02.21 Line of Business: Commercial, Medicaid Revision Log
Clinical Policy: Iobenguane I-131 (Azedra) Reference Number: ERX.SPA.420 Effective Date: 03.01.21 Last Review Date: 02.21 Line of Business: Commercial, Medicaid Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Iobenguane I-131 (Azedra®) injection is a radioactive agent. FDA Approved Indication(s) Azedra is indicated for the treatment of adult and pediatric patients 12 years and older with iobenguane scan positive, unresectable, locally advanced or metastatic pheochromocytoma or paraganglioma who require systemic anticancer therapy. Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. Health plan approved formularies should be reviewed for all coverage determinations. Requirements to use preferred alternative agents apply only when such requirements align with the health plan approved formulary. It is the policy of health plans affiliated with Envolve Pharmacy Solutions™ that Azedra is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Pheochromocytoma and Paraganglioma (must meet all): 1. Diagnosis of pheochromocytoma or paraganlioma; 2. Prescribed by or in consultation with an oncologist; 3. Age ≥ 12 years; 4. Tumor is unresectable, locally advanced, or metastatic; 5. Member currently receives medication to control tumor secretion of catecholamines (e.g., epinephrine, norepinephrine, dopamine) and related symptoms (e.g., hypertension, arrhythmia, hyperglycemia); 6. Metaiodobenzylguanidine (MIBG) scan is positive; 7. Concurrent radiopharmaceuticals have not been prescribed (e.g., Lutathera® [lutetium lu-177 dotatate]); 8. Request meets one of the following (a or b):* a. Dose does not exceed (i or ii): i. -
COMMENT (11) Status: Pending Post PUBLIC SUBMISSION PUBLICATION Tracking No
Page 1 of 2 SUNSI Review Complete Template = ADM-013 E-RIDS=ADM-03 ADD: Jazel Parks, As of: 10/1/19 1:22 PM Harriet Karagiannis Received: September 25, 2019 COMMENT (11) Status: Pending_Post PUBLIC SUBMISSION PUBLICATION Tracking No. 1k3-9ce3-dnzr DATE: 7/26/2019 Comments Due: September 26, 2019 CITATION 84 FR Submission Type: Web 36127 Docket: NRC-2019-0154 Release of Patients Administered Radioactive Material Comment On: NRC-2019-0154-0003 Release of Patients Administered Radioactive Material; Extension of comment period Document: NRC-2019-0154-DRAFT-0012 Comment on FR Doc # 2019-17060 Submitter Information Name: Daniel Miron Address: W176S8019 Joel Drive Muskego, WI, 53150 Email: [email protected] General Comment I am pleased to comment on the draft regulatory guide (DG), DG-8057, Release of Patients Administered Radioactive Material that was published in the Federal Register on July 26, 2019. (Docket ID NRC-2019- 0154). I am a health physicist who is certified by the American Board of Health Physics and have over 25 years of health physics experience in medical health physics. This includes being the Radiation Safety Officer (RSO) on multiple limited scope and broad scope medical licenses. I recommend that the data for I-123 NaI in table 3 Activities of Radiopharmaceuticals That Require Instructions and Records When Administered to Patients Who Are Breastfeeding an Infant or Child be reviewed and updated to reflect the current clinical use of I-123 NaI. Specifically the recommended duration of interruption of breastfeeding should be changed to Complete cessation due to the reasons listed below. -

RADIO PHARMACEUTICALS Production Control Safety Precautions Applications Storage
RADIO PHARMACEUTICALS Production control Safety precautions Applications Storage. Presented by: K. ARSHAD AHMED KHAN M.Pharm, (Ph.D) Department of Pharmaceutics, Raghavendra Institute of Pharmaceutical Education and Research [RIPER] Anantapur. 1 DEFINITION: Radiopharmaceuticals are the radioactive substances or radioactive drugs for diagnostic or therapeutic interventions. or Radiopharmaceuticals are medicinal formulations containing radioisotopes which are safe for administration in humans for diagnosis or for therapy. 2 COMPOSITION: • A radioactive isotope that can be injected safely into the body, and • A carrier molecule which delivers the isotope to the area to be treated or examined. 3 USAGE/WORKING: 4 BASICS Nuclide: This is a particular nuclear species characterized by its atomic number (No. of protons) and mass 12 23 number (No. of protons + neutrons). 6C , 11Na Isotopes: These are nuclides with same atomic number and different mass number. 1 2 3 Hydrogen has 3 isotopes --- 1H , 1H , 1H . 10 11 12 13 14 Carbon has 5 isotopes ------6C , 6C , 6C , 6C , 6C . 5 • ISOTOPES MAY BE STABLE OR UNSTABLE. • The nucleus is unstable if the number of neutrons is less or greater than the number of protons. • If they are unstable, they under go radioactive decay or disintegration and are known as radioactive isotopes/ radioactive nuclides. Radioactivity: The property of unstable nuclides of emitting radiation by spontaneous transformation of nuclei into other nuclides is called radioactivity. •Radioactive isotopes emit radiations or rays like α, β, γ rays. 6 PRODUCTION CONTROL 7 8 9 10 11 12 13 14 15 Radiopharmaceuticals production occurs in machines like 1. Cyclotron (low energy, high energy) 2. -

Radiopharmaceuticals and Contrast Media – Oxford Clinical Policy
UnitedHealthcare® Oxford Clinical Policy Radiopharmaceuticals and Contrast Media Policy Number: RADIOLOGY 034.19 T0 Effective Date: January 1, 2021 Instructions for Use Table of Contents Page Related Policies Coverage Rationale ....................................................................... 1 • Cardiology Procedures Requiring Prior Definitions .................................................................................... 10 Authorization for eviCore Healthcare Arrangement Prior Authorization Requirements .............................................. 10 • Radiation Therapy Procedures Requiring Prior Applicable Codes ........................................................................ 10 Authorization for eviCore Healthcare Arrangement Description of Services ............................................................... 13 • Radiology Procedures Requiring Prior Authorization References ................................................................................... 13 for eviCore Healthcare Arrangement Policy History/Revision Information ........................................... 14 Instructions for Use ..................................................................... 14 Coverage Rationale eviCore healthcare administers claims on behalf of Oxford Health Plans for the following services that may be billed in conjunction with radiopharmaceuticals and/or contrast media: • Radiology Services: Refer to Radiology Procedures Requiring Prior Authorization for eviCore Healthcare Arrangement for additional information. -

Nuclear Pharmacy Quick Sample
12614-01_CH01-rev3.qxd 10/25/11 10:56 AM Page 1 CHAPTER 1 Radioisotopes Distribution for Not 1 12614-01_CH01-rev3.qxd 10/25/1110:56AMPage2 2 N TABLE 1-1 Radiopharmaceuticals Used in Nuclear Medicine UCLEAR Chemical Form and Typical Dosage P Distribution a b HARMACY Radionuclide Dosage Form Use (Adult ) Route Carbon C 11 Carbon monoxide Cardiac: Blood volume measurement 60–100 mCi Inhalation Carbon C 11 Flumazenil injection Brain: Benzodiazepine receptor imaging 20–30 mCi IV Q UICK Carbon C 11 Methionine injection Neoplastic disease evaluation in brain 10–20 mCi IV R Carbon C 11 forRaclopride injection Brain: Dopamine D2 receptor imaging 10–15 mCi IV EFERENCE Carbon C 11 Sodium acetate injection Cardiac: Marker of oxidative metabolism 12–40 mCi IV Carbon C 14 Urea Diagnosis of Helicobacter pylori infection 1 µCi PO Chromium Cr 51 Sodium chromate injection Labeling red blood cells (RBCs) for mea- 10–80 µCi IV suring RBC volume, survival, and splenic sequestration Cobalt Co 57 Cyanocobalamin capsules Diagnosis of pernicious anemia and 0.5 µCi PO Not defects of intestinal absorption Fluorine F 18 Fludeoxyglucose injection Glucose utilization in brain, cardiac, and 10–15 mCi IV neoplastic disease Fluorine F 18 Fluorodopa injection Dopamine neuronal decarboxylase activity 4–6 mCi IV in brain Fluorine F 18 Sodium fluoride injection Bone imaging 10 mCi IV Gallium Ga 67 Gallium citrate injection Hodgkin’s disease, lymphoma 8–10 mCi IV Acute inflammatory lesions 5 mCi IV Indium In 111 Capromab pendetide Metastatic imaging in patients with biopsy- -

Targeted Radiotherapeutics from 'Bench-To-Bedside'
RadiochemistRy in switzeRland CHIMIA 2020, 74, No. 12 939 doi:10.2533/chimia.2020.939 Chimia 74 (2020) 939–945 © C. Müller, M. Béhé, S. Geistlich, N. P. van der Meulen, R. Schibli Targeted Radiotherapeutics from ‘Bench-to-Bedside’ Cristina Müllera, Martin Béhéa, Susanne Geistlicha, Nicholas P. van der Meulenab, and Roger Schibli*ac Abstract: The concept of targeted radionuclide therapy (TRT) is the accurate and efficient delivery of radiation to disseminated cancer lesions while minimizing damage to healthy tissue and organs. Critical aspects for success- ful development of novel radiopharmaceuticals for TRT are: i) the identification and characterization of suitable targets expressed on cancer cells; ii) the selection of chemical or biological molecules which exhibit high affin- ity and selectivity for the cancer cell-associated target; iii) the selection of a radionuclide with decay properties that suit the properties of the targeting molecule and the clinical purpose. The Center for Radiopharmaceutical Sciences (CRS) at the Paul Scherrer Institute in Switzerland is privileged to be situated close to unique infrastruc- ture for radionuclide production (high energy accelerators and a neutron source) and access to C/B-type labora- tories including preclinical, nuclear imaging equipment and Swissmedic-certified laboratories for the preparation of drug samples for human use. These favorable circumstances allow production of non-standard radionuclides, exploring their biochemical and pharmacological features and effects for tumor therapy and diagnosis, while investigating and characterizing new targeting structures and optimizing these aspects for translational research on radiopharmaceuticals. In close collaboration with various clinical partners in Switzerland, the most promising candidates are translated to clinics for ‘first-in-human’ studies. -
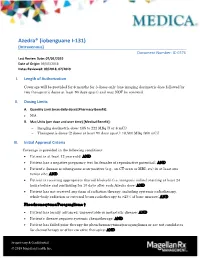
Azedra® (Iobenguane I‐131) (Intravenous) Document Number: IC‐0376 Last Review Date: 07/01/2019 Date of Origin: 09/05/2018 Dates Reviewed: 09/2018, 07/2019
Azedra® (iobenguane I‐131) (Intravenous) Document Number: IC‐0376 Last Review Date: 07/01/2019 Date of Origin: 09/05/2018 Dates Reviewed: 09/2018, 07/2019 I. Length of Authorization Coverage will be provided for 6 months for 3 doses only (one imaging dosimetric dose followed by two therapeutic doses at least 90 days apart) and may NOT be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [Pharmacy Benefit]: N/A B. Max Units (per dose and over time) [Medical Benefit]: Imaging dosimetric dose: 185 to 222 MBq (5 or 6 mCi) Therapeutic doses (2 doses at least 90 days apart): 18,500 MBq (500 mCi) III. Initial Approval Criteria Coverage is provided in the following conditions: Patient is at least 12 years old; AND Patient has a negative pregnancy test (in females of reproductive potential); AND Patient’s disease is iobenguane scan-positive (e.g., on CT-scan or MRI, etc) in at least one tumor site; AND Patient is receiving appropriate thyroid blockade (i.e. inorganic iodine) starting at least 24 hours before and continuing for 10 days after each Azedra dose; AND Patient has not received any form of radiation therapy, including systemic radiotherapy, whole-body radiation or external beam radiotherapy to >25% of bone marrow; AND Pheochromocytoma/Paraganglioma † Patient has locally advanced, unresectable or metastatic disease; AND Patient’s disease requires systemic chemotherapy; AND Patient has failed prior therapy for pheochromocytoma/paraganglioma or are not candidates for chemotherapy or other curative therapies; AND Proprietary & Confidential © 2019 Magellan Health, Inc. Patient has a life expectancy of at least 6 months; AND Patient has a Karnofsky Performance Status score ≥ 60; AND Patient does not have uncontrolled/unstable hypertension † FDA Approved Indication(s); ‡ Compendia recommended indication(s) IV. -

Bispecific Antibody Pretargeting of Radionuclides for Immuno^ Single
Bispecific Antibody Pretargeting of Radionuclides for Immuno ^ Single-Photon Emission Computed Tomography and Immuno ^ Positron Emission Tomography Molecular Imaging:An Update Robert M. Sharkey,1Habibe Karacay,1William J. McBride,2 Edmund A. Rossi,3 Chien-Hsing Chang,3 and David M. Goldenberg1 Abstract Molecular imaging is intended to localize disease based on distinct molecular/functional characteristics. Much of today’s interest in molecular imaging is attributed to the increased acceptance and role of 18F-flurodeoxyglucose (18F-FDG) imaging in a variety of tumors. The clinical acceptance of 18F-FDG has stimulated research for other positron emission tomography (PET) agents with improved specificity to aid in tumor detection and assessment. In this regard, a number of highly specific antibodies have been described for different cancers. Although scintigraphic imaging with antibodies in the past was helpful in patient management, most antibody-based imaging products have not been able to compete successfully with the sensitivity afforded by 18F-FDG-PET, especially when used in combination with computed tomography. Recently, however, significant advances have been made in reengineering antibodies to improve their targeting properties. Herein, we describe progress being made in using a bispecific antibody pretargeting method for immuno ^ single-photon emission computed tomography and immunoPETapplications, as contrasted to directly radiolabeled antibodies.This approach not only significantly enhances tumor/nontumor ratios but also provides high signal intensity in the tumor, making it possible to visualize micrometastases of colonic cancer as small as 0.1to 0.2 mm in diameter using an anti ^ carcinoembryonic antigen bispecific antibody, whereas FDG failed to localize these lesions in a nude mouse model. -

Radiotoxicity After Iodine-131 Therapy for Thyroid Cancer Using the Micronucleus Assay
Radiotoxicity After Iodine-131 Therapy for Thyroid Cancer Using the Micronucleus Assay Naoto Watanabe, Kunihiko Yokoyama, Seigo Kinuya, Noriyuki Shuke, Masashi Shimizu, Ryusuke Futatsuya, Takatoshi Michigishi, Norihisa Tonami, Hikaru Seto and David A. Goodwin Departments of Radiology and Radiological Science, Toyama Medical and Pharmaceutical University, Toyama; Department of Nuclear Medicine, Kanazawa University, Kanazawa; Department of Radiology, Asahikawa Medical University, Asahikawa, Japan; Nuclear Medicine Service, Veterans Affairs Health Sciences, Palo Alto, California; and Department of Radiology, Stanford University School of Medicine, Stanford, California thrombocytopenia have been reported (6,7). Therefore, in most The purpose of the present study was to evaluate the degree of patients who are treated with a large amount of I3il, the limiting cytological radiation damage to lymphocytes after1311therapy using the cytokinesis-blocked micronucleus assay. The chromosomal factor is the radiation dose to the blood and the bone marrow damage to lymphocytes induced by 131I ¡nvivo should result in (8). Dosimetrie studies have estimated the radiation dose to the augmentation of the cells with micronuclei. Methods: We studied 25 blood and bone marrow with a large amount of radioiodine (3 ). patients with differentiated thyroid carcinoma who were treated with Previous work has been done on cytogenetic changes (9). 3.7 GBq of 131I.Isolated lymphocytes collected from patients 1 wk However, the cytological effects of radiation exposure on the after therapy were harvested and treated according to the cytoki lymphocytes in vivo with large therapeutic doses of radioiodine nesis-blocked method of Fenech and Morley. The micronucleus have not been extensively examined. number of micronuclei per 500 binucleated cells were scored by The purpose of our study was to evaluate the degree of visual inspection. -

EANM Procedure Guidelines for 131I-Meta-Iodobenzylguanidine (131I-Mibg) Therapy
Eur J Nucl Med Mol Imaging (2008) 35:1039–1047 DOI 10.1007/s00259-008-0715-3 GUIDELINES EANM procedure guidelines for 131I-meta-iodobenzylguanidine (131I-mIBG) therapy Francesco Giammarile & Arturo Chiti & Michael Lassmann & Boudewijn Brans & Glenn Flux Published online: 15 February 2008 # EANM 2008 Abstract Meta-iodobenzylguanidine, or Iobenguane, is an nervous system. The neuroendocrine system is derived from a aralkylguanidine resulting from the combination of the family of cells originating in the neural crest, characterized by benzyl group of bretylium and the guanidine group of an ability to incorporate amine precursors with subsequent guanethidine (an adrenergic neurone blocker). It is a decarboxylation. The purpose of this guideline is to assist noradrenaline (norepinephrine) analogue and so-called nuclear medicine practitioners to evaluate patients who might “false” neurotransmitter. This radiopharmaceutical, labeled be candidates for 131I-meta-iodobenzylguanidine to treat with 131I, could be used as a radiotherapeutic metabolic agent neuro-ectodermal tumours, to provide information for in neuroectodermal tumours, that are derived from the performing this treatment and to understand and evaluate primitive neural crest which develops to form the sympathetic the consequences of therapy. F. Giammarile (*) Keywords Guidelines . Therapy . mIBG CH Lyon Sud, EA 3738, HCL, UCBL, 165 Chemin du Grand Revoyet, Purpose 69495 Pierre Benite Cedex, France e-mail: [email protected] The purpose of this guideline is to assist nuclear medicine A. Chiti practitioners to U.O. di Medicina Nucleare, Istituto Clinico Humanitas, via Manzoni, 56, 1. Evaluate patients who might be candidates for 131I-meta- 20089 Rozzano (MI), Italy iodobenzylguanidine (mIBG) to treat neuro-ectodermal e-mail: [email protected] tumours M.