COMPLETE CHEMISTRY PANEL Scroll Down Or Click on the Following Parameters to Quickly Access Content CHEM15/17: GLU BUN CREA
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Myoglobin Expression Under Hypoxic Condtions In
THESIS IN THE FACE OF HYPOXIA: MYOGLOBIN EXPRESSION UNDER HYPOXIC CONDTIONS IN CULTURED WEDDELL SEAL SKELETAL MUSCLE CELLS Submitted by Michael Anthony De Miranda Jr. Department of Biology In partial fulfillment of the requirements For the degree of Master of Science Colorado State University Fort Collins, Colorado Spring 2012 Master’s Committee: Advisor: Shane Kanatous Gregory Florant Scott Earley Copyright by Michael A. De Miranda Jr. 2012 All Rights Reserved ABSTRACT IN THE FACE OF HYPOXIA: MYOGLOBIN EXPRESSION UNDER HYPOXIC CONDITIONS IN CULTURED WEDDELL SEAL SKELETAL MUSCLE CELLS The hallmark adaptation to breath-hold diving in Weddell seals (Leptonychotes weddellii) is enhanced concentrations of myoglobin in their skeletal muscles. Myoglobin is a cytoplasmic hemoprotein that stores oxygen for use in aerobic metabolism throughout the dive duration. In addition, throughout the duration of the dive, Weddell seals rely on oxygen stored in myoglobin to sustain aerobic metabolism in which lipid is the primary contributor of acetyl CoA for the citric acid cycle. Together, enhanced myoglobin concentrations and a lipid-based aerobic metabolism represent some of the unique adaptations to diving found in skeletal muscle of Weddell seals. This thesis presents data that suggests cultured Weddell seal skeletal muscle cells inherently possess adaptations to diving such as increased myoglobin concentrations, and rely on lipids to fuel aerobic metabolism. I developed the optimum culture media for this unique primary cell line based on myoblast confluence, myoblast growth rates, myotube counts, and myotube widths. Once the culture media was established, I then determined the de novo expression of myoglobin under normoxic and hypoxic oxygen conditions and the metabolic profile of the myotubes under each oxygen condition. -

Hba1c %, Total Serum Protein and Albumin Levels in Type 2 Diabetes Mellitus Patients: a Case-Control Study Dr
European Journal of Molecular & Clinical Medicine (EJMCM) ISSN: 2515-8260 Volume 07, Issue 11, 2020 Original research article HbA1c %, total serum protein and albumin levels in type 2 diabetes mellitus patients: a case-control study Dr. Shweta Kumari1*, Dr. Supriya2 1Junior Resident (Academic), Department of Pathology Darbhanga Medical College and Hospital, Laheriasarai, Darbhanga, Bihar, India 2Junior Resident (Academic), Department of Pathology Darbhanga Medical College and Hospital, Laheriasarai, Darbhanga, Bihar, India Corresponding Author: Dr. Shweta Kumari Abstract Aim: the aim of the study to assessment of glycated haemoglobin, total protein and albumin levels in patients with type 2 diabetes mellitus. Methods: This case control study was done the Department of Pathology Darbhanga Medical College and Hospital, Laheriasarai, Darbhanga, Bihar, India, for 1 year. The research enlisted 100 participants, 50 of whom were diabetic and 50 of whom were not, all of whom were between the ages of 40 and 70. Every patient's blood sample was obtained in 5mls, with 1ml dispensed into EDTA for glycated haemoglobin estimation and 4ml dispensed into clear containers for serum albumin and total protein estimation. Normal procedures were used to determine the amount of glycated haemoglobin, estimate serum albumin, and estimate total protein. Results: The mean level of HbA1c was significantly higher in the diabetic subjects when compared with control group (10.11±1.41Vs 6.18±0.71; p=0.000). There was no significant differences observed between the age, the serum levels of Albumin and Total protein in the test and control subjects (p>0.05). Conclusion: The present study showed significantly higher mean levels of HbA1c in the diabetic patients compared with the control subjects. -

International Journal of Medical and Biomedical Studies (IJMBS)
|| ISSN(online): 2589-8698 || ISSN(print): 2589-868X || International Journal of Medical and Biomedical Studies Available Online at www.ijmbs.info PubMed (National Library of Medicine ID: 101738825) Index Copernicus Value 2018: 75.71 Original Research Article Volume 4, Issue 3; March: 2020; Page No. 209-213 EVALUATION OF CHANGES IN LEVELS OF GLYCATED HEMOGLOBIN, TOTAL PROTEIN AND ALBUMIN IN PATIENTS DIAGNOSED WITH TYPE 2 DIABETES MELLITUS Dr. Vivek Kumar1, Dr. Neeraj Kumar2, Dr. Jaideo Prasad3 1Tutor, Dept. of Pathology, Anugrah Narayan Magadh Medical College and Hospital, Gaya, Bihar, India. 2Senior Resident, Dept. of Medicine, Anugrah Narayan Magadh Medical College and Hospital, Gaya, Bihar, India. 3Prof & HOD, Dept. of Pathology, Anugrah Narayan Magadh Medical College and Hospital, Gaya, Bihar, India. Article Info: Received 07 February 2020; Accepted 26 March 2020 DOI: https://doi.org/10.32553/ijmbs.v4i3.1099 Corresponding author: Dr. Neeraj Kumar Conflict of interest: No conflict of interest. Abstract Insulin resistance in Type 2 diabetes mellitus metabolism of carbohydrates, lipids and proteins gives an estimate of the average blood glucose the previous three months in diabetes. Protein and HbA1c have been shown to be involved complications of diabetes mellitus. Hence based on above findings the present study was planned for Evaluation of Changes in Levels of Glycated Hemoglobin, Total Protein and Albumin in Patients Diagnosed with Type 2 Diabetes Mellitus. The present study was planned in Anugrah Narayan Magadh Medical College and Hospital, Gaya, Bihar, India. In the present study 50 cases were evaluated. The 25 cases were enrolled on the Group A as normal cases in Control group. -
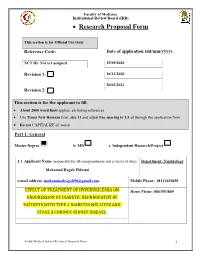
Of Treatment of Hyperuricemia on Effect
Faculty of Medicine Institutional Review Board (IRB) • Research Proposal Form This section is for Official Use Only Reference Code: Date of application (dd/mm/yyyy): NCT ID: Not yet assigned 15/09/2020 Revision 1: 10/12/2020 20/02/2021 Revision 2: This section is for the applicant to fill. • About 2000 word limit applies, excluding references. • Use Times New Romans Font, size 11 and adjust line spacing to 1.5 all through the application form • Do not CAPITALIZE all words Part 1: General Master Degree b. MD c. Independent Research/Project 1.1 Applicant Name (responsible for all correspondences and accuracy of data): Department: Nephrology Mohamed Ragab Eldremi email address: [email protected] Mobile Phone: 01114430050 EFFECT OF TREATMENT OF HYPERURICEMIA ON Home Phone: 0863553849 PROGRESSION OF DIABETIC NEPHROPATHY IN PATIENTS WITH TYPE 2 DIABETES MELLITUS AND STAGE 3 CHRONIC KIDNEY DISEASE. Assiut Medical School Research Proposal Form 1 Faculty of Medicine Institutional Review Board (IRB) 1.2 English Title of research project: EFFECT OF TREATMENT OF HYPERURICEMIA ON PROGRESSION OF DIABETIC NEPHROPATHY IN PATIENTS WITH TYPE 2 DIABETES MELLITUS AND STAGE 3 CHRONIC KIDNEY DISEASE. 1.3 Do you need funding from Assiut Medical School Grants Office? Yes No (If no, skip and delete Part 4) Mention other sponsoring agent(s) if any: ………………no…………………………... Part 2: Research Details Assiut Medical School Research Proposal Form 2 Faculty of Medicine Institutional Review Board (IRB) 2.1 Background (Research Question, Available Data from the literature, Current strategy for dealing with the problem, Rationale of the research that paves the way to the aim(s) of the work). -

Serum Uric Acid Concentrations and Risk of Adverse Outcomes in Patients with COVID-19
ORIGINAL RESEARCH published: 06 May 2021 doi: 10.3389/fendo.2021.633767 Serum Uric Acid Concentrations and Risk of Adverse Outcomes in Patients With COVID-19 † † † † † Bo Chen 1 , Chenyang Lu 1 , Hong-Qiu Gu 2,3 , Yang Li 4 , Guqin Zhang 5 , Jonathan Lio 6, Xiongyan Luo 1, Lingshu Zhang 1, Yidan Hu 1, Xiaomeng Lan 7, Zerong Chen 7, Qibing Xie 1* and Huaqin Pan 8,9,10* 1 Department of Rheumatology and Immunology, West China Hospital, Sichuan University, Chengdu, China, 2 China National Clinical Research Center for Neurological Diseases, Beijing Tiantan Hospital, Capital Medical University, Beijing, China, 3 National Center for Healthcare Quality Management in Neurological Diseases, Beijing Tiantan Hospital, Capital Medical University, Beijing, China, 4 Department of Endocrinology, West China Hospital, Sichuan University, Chengdu, China, 5 Department of Respiratory and Critical Care Medicine, Zhongnan Hospital of Wuhan University, Wuhan, China, 6 Internal Medicine, University of Chicago, Chicago, IL, United States, 7 West China School of Public Health and West China Fourth Hospital, Sichuan University, Chengdu, China, 8 Department of Critical Care Medicine, Zhongnan Hospital of Wuhan University, Wuhan, China, 9 Department of Critical Care Medicine, Leishenshan Hospital, Wuhan, China, 10 Clinical Research Edited by: Center of Hubei Critical Care Medicine, Wuhan, China Jeff M. P. Holly, University of Bristol, United Kingdom Background: Although hyperuricemia frequently associates with respiratory diseases, Reviewed by: Yu Sun, patients with severe coronavirus disease 2019 (COVID-19) and severe acute respiratory Shandong University, China syndrome (SARS) can show marked hypouricemia. Previous studies on the association of Ma. Cecilia Opazo, Andres Bello University, Chile serum uric acid with risk of adverse outcomes related to COVID-19 have produced *Correspondence: contradictory results. -

Serum Total Protein, Albumin, Globulin Population of Various Ages and Sex in Karachi and Their Ratio in Apparently Healthy
SERUM TOTAL PROTEIN, ALBUMIN, GLOBULIN POPULATION OF VARIOUS AGES AND SEX IN KARACHI AND THEIR RATIO IN APPARENTLY HEALTHY Pages with reference to book, From 12 To 16 Khushnaseeb Ibrahim, Sarwar Jehan Zuberi ( PMRC Research Centre, Jinnah Postgraduate Medical Centre, Karachi. ) Syed Naznil Husnain ( Department of Biochemistry, University of Karachi, Karachi. ) Abstract Serum proteins, albumin and globulin in 456 (274 males and 182 females) subjects were within the normal range and showed unifornt distribution. Mean protein levels were low in infants under 0—1 year of age. No significant change was noted with age and sex in other groups. These values were considered to be normal for our population as all protein values fell within 2.5 and 97.5 percentile (95% of the total population) irrespective of age and sex except babies under 0—1 year. The average intake of protein/kg body weight was almost upto the recommended allowances(JPMA 39: 12, 1989). INTRODUCTION Serum protein levels in normals vary from 63—8 g% and albumin 4—6 g% 1-4 . This study repbrts levels of serum proteins, albumin, globulins and albumin/globulin ratios in healthy subjects and their relationship with age, sex and protein intake. SUBJECTS AND METHOD One thousand and thirty-six (526 males and 510 females) healthy subjects were selected from the hospital staff, well baby clinics, MCH Centres, primary and secondary schools, colleges and various organizations according to percentage distribution of age and sex in the Karachi population (Census, 1972). Information regarding age, sex, general physical health, dietary history, height and weight were recorded on a preceded proforma. -

Calcium and Phosphorus Metabolism of Bone Tissue
ÚSTAV LÉKAŘSKÉ BIOCH EMIE A LABORATORNÍ DIAGNO STIKY 1. LF UK Calcium and phosphorus Metabolism of bone tissue General Medicine Lenka Fialová & Martin Vejražka translated and edited by Jan Pláteník 2018/2019 1 Bone Tissue Bone provides mechanical support and protection to soft organs, enables movement, hosts hematopoietic tissue, and serves as storage of calcium, phosphate, and magnesium ions. From one third it consists of protein matrix , and from two thirds of the bone mineral . • The bone protein matrix contains mostly type I collagen (90 %); together with other proteins such as osteocalcin, osteonectin, osteopontin, etc. (10 %). • The bone mineral is composed from small crystals of hydroxyapatite Ca 10 (PO 4)6(OH) 2. Other compounds, such as calcium carbonate, calcium fluoride and magnesium phosphate, are present as well. The metabolic activity of bone tissue is provided by bone cells. Osteoblasts form osteoid (the bone protein matrix), into which mineral salts are deposited. Other cell types include osteoclasts , whose main function is bone resorption, and osteocytes , which complement activity of osteoclasts by providing fine tuning of bone resorption. During lifetime of an individual, the bone tissue is subject of perpetual remodelation , encompassing osteoclastic bone resorption followed by osteoblastic bone formation . Osteoclasts dissolve mineral components and degrade the bone matrix. On the other hand, osteoblasts intracellularly synthesize precursors of the bone matrix proteins. Functional coupling of bone resorption and formation ensures that the living bone tissue is constantly renewed. Metabolism of bones is tightly coupled to metabolism of calcium and phosphorus. 2 Calcium 2.1 Homeostasis of calcium Human body contains about 1,000 g of calcium. -

Glasgow Prognostic Score Predicts Prognosis of Intrahepatic Cholangiocarcinoma
566 MOLECULAR AND CLINICAL ONCOLOGY 6: 566-574, 2017 Glasgow Prognostic Score predicts prognosis of intrahepatic cholangiocarcinoma QUN-XIONG PAN, ZI-JIAN SU, JIAN-HUA ZHANG, CHONG-REN WANG and SHAO-YING KE Department of Oncological Surgery, Quanzhou First Affiliated Hospital of Fujian Medical University, Quanzhou, Fujian 362000, P.R. China Received May 6, 2016; Accepted September 26, 2016 DOI: 10.3892/mco.2017.1166 Abstract. High Glasgow Prognostic Score (GPS) has been Introduction associated with poor prognosis in patients with lung, ovarian, colorectal and renal cancer, as well as hepatocellular carcinoma. Intrahepatic cholangiocarcinoma (ICC) is an intrahepatic The aim of this study was to investigate the prognostic value of malignancy arising from the biliary epithelium in the intra- GPS in patients with intrahepatic cholangiocarcinoma (ICC) hepatic bile duct from the segmental and area ducts and their undergoing partial hepatectomy. A total of 72 patients with finer branches to the small bile ducts and ductules (1,2). ICC pathologically confirmed ICC were classified according to is the second most frequent intrahepatic primary liver tumour their GPS scores assigned based on the preoperative levels of after hepatocellular carcinoma (3), accounting for 5-10% of C-reactive protein (CRP) and albumin. Their clinicopatho- primary liver cancer cases (4). Of note, the global incidence logical data were retrospectively assessed using univariate and of ICC has been steadily increasing over the last 30 years (4). multivariate analysis to determine their association with overall From the early 1970s to 1999, the ICC incidence in United survival and recurrence. High GPS scores in ICC patients States and China increased by >150% (4,5). -

Association of Glycated Albumin/Glycosylated Hemoglobin
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy Dovepress open access to scientific and medical research Open Access Full Text Article ORIGINAL RESEARCH Association of Glycated Albumin/Glycosylated Hemoglobin Ratio with Blood Glucose Fluctuation and Long-Term Blood Glucose Control in Patients with Type 2 Diabetes Mellitus Bai-Rong Wang1,2 Objective: This study aimed to investigate the association of the glycated albumin (GA)/ Jun-Teng Yao2 glycosylated hemoglobin (HbA1c) ratio with the mean amplitude of glycemic excursion Hui Zheng1 (MAGE) in type 2 diabetes mellitus (T2DM). Quan-Min Li1 Methods: A total of 102 patients with T2DM who were first treated in Jinjiang Hospital of Fujian Province were enrolled in this study. The patients’ general clinical data, including 1 Department of Endocrinology, Medical HbA1c, GA, fasting blood glucose, and fasting and peak C-peptide values upon diagnosis College of Soochow University, Suzhou 215123, Jiangsu, People's Republic of and after one year of follow-up, were collected, and their MAGE was calculated. China; PLA Rocket Force Characteristic Results: With the increase of the GA/HbA1c ratio at baseline, the patients’ fasting and peak Medical Center, Beijing, 100088, People’s Republic of China; 2Department of C-peptide values decreased gradually from baseline to follow-up, while their MAGE, Endocrinology, Jinjiang Municipal HbA1c, and fasting blood glucose increased gradually. A regression analysis demonstrated Hospital, Jinjiang, 362200, People’s that the baseline MAGE was independently positively correlated with the GA/HbA1c ratio. Republic of China A Cox regression analysis demonstrated that a baseline GA/HbA1c ratio of >2.78 was an independent risk factor for poor fasting blood glucose and HbA1c. -

Download PDF Mckittrick-Wheelock Syndrome: a Rare Etiology of Acute
Rom J Morphol Embryol 2011, 52(3 Suppl):1153–1156 R J M E ASE EPORT Romanian Journal of C R Morphology & Embryology http://www.rjme.ro/ McKittrick–Wheelock syndrome: a rare etiology of acute renal failure associated to well-differentiated adenocarcinoma (G1) arising within a villous adenoma LILIANA ANA TUŢĂ1), MĂDĂLINA BOŞOTEANU2), MARIANA DEACU2), E. DUMITRU3) 1)Department of Nephrology 2)Department of Pathology 3)Department of Gastroenterology Faculty of Medicine, “Ovidius” University, Constanta Emergency County Hospital, Constanta Abstract Introduction: Large villous adenomas or adenocarcinomas of the rectum can determine secretory diarrhea, associated with a depleting syndrome of prerenal acute renal failure, hyponatremia, hypokalemia, and hypoproteinemia, with favorable prognosis if early detected and properly treated. The syndrome is rare, with approximately 50 cases reported in the literature. Aim: Acute renal failure, caused by fluids and electrolytes hypersecretion, secondary to a malignant rectal villous adenoma is revealed in a 55-year-old patient, admitted with major hydro-electrolytic and acid-base disturbances to our Nephrology Department. Case Presentation: The 55-year-old male patient had a nine months history of mucous diarrhea, for which he was treated unsuccessfully by GP’s and infectionists. The symptomatology aggravated progressively and the patient was admitted through ICU with oligoanuria, severe dehydration and hydro-electrolytic and acid-base disturbances. Rectosigmoidoscopy revealed a giant villous adenoma at the rectum. Conservative therapy initially improved, and finally normalized renal function and made possible surgical resection of the tumor, with an excellent evolution afterwards. Conclusions: The McKittrick–Wheelock syndrome is a rare, life-threatening condition that requires interdisciplinary medical diagnosis and treatment, but has a good prognosis if renal function is recovered in time and makes possible curative tumoral resection. -

Myoglobin from Equine Skeletal Muscle
Myoglobin from equine skeletal muscle Catalog Number M0630 Storage Temperature –20 C CAS RN 100684-32-0 Precautions and Disclaimer This product is for R&D use only, not for drug, Product Description household, or other uses. Please consult the Safety Molecular mass:1 17.6 kDa Data Sheet for information regarding hazards and safe Extinction coefficient:2 EmM = 12.92 (555 nm) handling practices. pI:3 7.3 (major component) and 6.8 (minor component) Preparation Instructions Myoglobin from horse skeletal muscle is a single chain This protein is soluble in water (10 mg/ml), yielding a heme protein containing 153 amino acid residues. It clear, red brown solution. posesses no disulfide bridges or free -SH groups. Myoglobin contains 8 variously sized right-handed References helical regions, joined by non-ordered or random coil 1. Darbre, P.D. et al., Comparison of the myoglobin of regions. These 8 helices (A, B, C, D, E, F, G, and H) the zebra (Equus burchelli) with that of the horse are folded back on top of one another, and the heme is (Equus cabalus). Biochim. Biophys. Acta, 393(1), situated between helices E and F. The heme is almost 201-204 (1975). totally buried. Only the edge carrying the two 2. Bowen, W.J., The absorption spectra and extinction hydrophylic propionic acid groups is exposed. The coefficients of myoglobin. J. Biol. Chem., 179, 235- heme is held in position by a coordinating complex 245 (1949). between the central Fe(II) atom and 2 histidine residues 3. Radola, B.J., Isoelectric focusing in layers of (on helices E and F, respectively). -

Association Between Serum Liver Enzymes and Hypertension
Rahman et al. BMC Cardiovascular Disorders (2020) 20:128 https://doi.org/10.1186/s12872-020-01411-6 RESEARCH ARTICLE Open Access Association between serum liver enzymes and hypertension: a cross-sectional study in Bangladeshi adults Sadaqur Rahman, Shiful Islam, Tangigul Haque, Rahanuma Raihanu Kathak and Nurshad Ali* Abstract Background: Hypertension is a major contributing factor to cardiovascular disease and is a leading cause of death in the world. The association between hepatic enzymes and hypertension has been reported in limited studies and the findings are inconsistent; data from Bangladeshi adults are not available yet. This study was conducted to estimate the prevalence of elevated liver enzymes and evaluate the association of elevated liver enzymes with hypertension in Bangladeshi adults. Methods: In this cross-sectional study, 302 blood samples were collected from adult participants and analyzed the serum concentrations of alanine and aspartate aminotransferase (ALT, AST), alkaline phosphatase (ALP), and γ-glutamyltransferase (GGT) and other markers related to hypertension. Hypertension was defined as resting SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg. Associations between elevated liver enzymes and hypertension were evaluatedbymultinomiallogistic regression. Results: The mean concentrations of serum ALT, AST and GGT were significantly higher in the hypertensive group compared to the normotensive group (p < 0.01, p <0.01andp < 0.001, respectively). Overall, 49.2% of subjects in the hypertensive group and 38.1% of individuals in the normotensive group had at least one or more elevated liver enzymes. The prevalence of elevated ALT, AST, and GGT was significantly higher among participants in the hypertensive group compared to the normotensive group (p < 0.01, p <0.01andp < 0.001, respectively).