Functional Assessment of Gastrointestinal Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Intestinal-Health Catalog
Dr Michael Hirt Page: 1 The Center for Integrative Medicine TABLE OF CONTENTS Intestinal Health ...................................................................................................... 2 CONFIDENTIAL Dr Michael Hirt Page: 2 The Center for Integrative Medicine INTESTINAL HEALTH GUTSY WHAT IT IS: A natural source of butyrate, a molecule that is necessary for intestinal health and healing. WHY YOU NEED IT: Important for patients with leaky gut and food intolerances Supports patients with Irritable Bowel Syndrome, gas, bloating, constipation Great for patients needing improved regularity Promotes a healthy inflammatory response in the intestines Supports healthy gut flora and biome Targets patients looking for overall health enhancements by improving crosstalk between the gut and your brain, skin, kidney and lungs. Important support for maintaining a healthy immune system and for patients with autoimmune diseases, like Lupus, Hashimoto’s, Rheumatoid Arthritis, colitis, Crohn’s disease Good for patients with neuro-degenerative disorders (like Parkinson’s, MS, dementia) and psychiatric disorders (anxiety, depression) Designed for patients needing to rebuild or improve their gut microbiome. HOW IT... Read More Price: CONFIDENTIAL Dr Michael Hirt Page: 3 The Center for Integrative Medicine BITTER TRUTH WHAT IT IS: A blend of organic herbs for patient with gas, bloating, and weak digestion WHY YOU NEED IT: Important for patients with IBS symptoms including gas, bloating and nausea. Great for patients with poor motility, like gastroparesis Targets patients with nausea, indigestion, heartburn, and acid reflux Fast acting, non-drug formula Safe and organic herbal blend HOW IT HELPS: Herbal bitters are a classic remedy for patients wanting healthy digestion. The Bitter Truth contains some twenty herbs known by traditional herbalists to support healthy gut functioning. -
Assignment Discovery Online Curriculum Digestion Curriculum
Assignment Discovery Online Curriculum Digestion Curriculum Focus Health Grade level 9-12 Duration One or two class periods Objectives Students will • research one common problem of the digestive system, such as constipation, gas, lactose intolerance, or ulcers • create a brochure, similar to one found at a doctor’s office, that describes the problem, its causes, symptoms, and possible treatments Materials • Paper (8½ x 11 inches) • Pens, pencils • Computer with Internet access Procedures 1. Begin the lesson by reviewing the major organs of the digestive system and the function of each. Make sure your discussion covers at least the following parts of the digestive tract: esophagus, stomach, small intestine, large intestine, and colon. You will find a good overview at: Discovery Health: Healthy Digestion http://health.discovery.com/centers/digestive/digestion.html 2. Ask students to name some of the problems of the digestive system covered in the video. Challenge students to link each condition with the appropriate part of the digestive tract. Below are some common digestive problems. (See “Vocabulary” for definitions.) • nausea • diarrhea • constipation • acid indigestion (heartburn) • gastroesophageal reflux disease (GERD) • ulcer • lactose intolerance • colorectal polyps or colorectal cancer 3. Have students work individually to create a patient brochure about one digestive problem. The brochure, similar to one they might see in a doctor’s office, should describe the problem, its causes, symptoms, and possible treatments. In addition, the brochure should be written and designed for a specific audience, such as kids, teens, young adults, middle-age adults, or older adults. When selecting an appropriate audience, ask students to consider what age a patient might be when he or she has questions about that problem. -

The Importance of Healthy Digestion an Ayurvedic Guide to Understanding Agni
The Importance of Healthy Digestion An Ayurvedic Guide to Understanding Agni The concept of agni, the Sanskrit word for “fire,” is rather essential to the Ayurvedic tradition. Ayurveda views agni as the very source of life. It is said that a man is as old as his agni and that when agni is extinguished, we die.1 Perhaps even more significantly, Ayurveda teaches us that impaired agni is at the root of every imbalance and disease. So the importance of agni in Ayurveda simply cannot be understated. This resource is intended to give you a deeper understanding and appreciation of agni, while offering you some practical tools with which to tend to your own agni. 800.953.6424 | BANYANBOTANICALS.COM 1 What is Agni? Fire has been worshiped throughout human history. In fact, Indo-European languages often had two distinct words for it: one for an inanimate form of fire, one for an animate form.2 Interestingly, the English word “fire” was born out of the inanimate form.2 On the other hand, the Sanskrit word agni (pronounced uhg-nih) is one of the oldest known words for the living, breathing variety of fire. Agni is also the root from which a number of words evoking the dynamic nature of fire emerged: “ignis” (Latin), “ugnis” (Old Prussian), as well as “ignite” and “igneous” (English).1, 2 As its etymological history suggests, the deeper significance of the Sanskrit word agni is profound—sacred, even. The Vedic culture revered fire for its light, its warmth, and its ability to cook food.3 But the Vedic understanding of agni extends well beyond “fire” in its physical form. -

Botanicals and Nutritional Compounds to Support Gastrointestinal Health
Botanicals and Nutritional Compounds to Support Gastrointestinal Health Co-authored by Donald R. Yance Jr., RH (AHG), CN and Suzanne E. Sky, L.Ac., MTOM Table of Contents Gastrointestinal Lining: Key to Gastrointestinal Health.....................................................................3 Gastrointestinal Disease and Health ................................................................................................ 3 Gastric Disease and GERD ..............................................................................................................4 Stomach Health and Gastric Acid ....................................................................................................... 5 The Stomach Lining and Gastritis ................................................................................................... 6 H. pylori Influences Gastric Health .................................................................................................. 6 Inflammation and Tissue Integrity...................................................................................................... 8 Mucosal Layer Transport and Role ...................................................................................................9 Intestinal Permeability and Tight Junctions ..................................................................................... 9 Stress and Intestinal Barrier Health .................................................................................................. 9 The Gut Microbiome and the Enteric Nervous -

Digestion and Elimination
Anne Fischer-Silva, CNT, LE DIGESTION AND ELIMINATION It has been said “You are what you eat.” We all understand the importance of eating nutrient-dense foods in order to achieve optimal health. A bigger issue, however, is how much of the nutrients in the foods you eat are actually absorbed and utilized? A more important and accurate statement might be “You are what you assimilate from what you eat”. The difference between the nutrients present in foods and how your body uses them represents the distinction between diet and nutrition. Diet is made up of what you eat. Nutrition is what your body does with the food. So then, you may ask, is it possible to eat a very healthy, nutrient-rich diet and still not obtain adequate nutrition from the food consumed? The answer is YES! Malabsorption is a term used to describe an overall reduction in digestive efficiency and performance. Many factors are involved with malabsorption – from stress to parasites. The human gastrointestinal tract is a complex system of mental, chemical, and mechanical functions. Digestive symptoms are some of the most common complaints today in the U.S. Many people have acclimated so completely to their poorly functioning digestive tract, they may come to think it is normal. Symptoms like bloating, excessive flatulence, constipation, and diarrhea are quite common, and yet they are signs of a dysfunctional GI tract. Here is a description of what optimal digestion looks like: • Digestion starts in the brain. It begins when we anticipate the act of eating. When we see and smell food, our brain signals the release of saliva. -

Digestive Formula
04070315_DigestiveFormPIP.qxd 2/15/05 10:55 AM Page 1 PHARMANEX® PRODUCT INFORMATION PAGE Digestive Formula PROMOTES HEALTHY DIGESTION* Positioning Statement • Provides a unique and comprehensive three-step approach to Digestive Formula contains a unique blend of natural extracts healthy digestion* to aid healthy digestion of food, prevent and alleviate the • Digestive Formula utilizes a proprietary blend of plant-based symptoms of occasional indigestion, and help the body recover enzymes, including three pH-specific proteases from over-consumption.* What Makes This Product Unique? Concept • Ginger root extract (Zingiber officinale) is standardized to Proper digestion is essential for good health. Anything that 5% gingerols 1 adversely affects digestive function may cause discomfort. • Digestive Formula addresses the number one cause of Millions of people worldwide—including up to one third of indigestion—normal bile production and normal function of the the U.S. population—suffer from occasional indigestion and liver-bile system* experience common digestive complaints. Symptoms include • Digestive Formula’s artichoke leaf extract is standardized to early feelings of satiation and temporary loss of appetite, 15% caffeoylquinic acids, three times the potency of most infrequent heartburn, nausea, flatulence, excessive belching, artichoke products currently available in the U.S. fat intolerance, and short-term constipation. Other factors that • Digestive Formula utilizes three pH-specific proteases that can also cause such digestive discomforts include stress, sick- become active in the digestive tract, compensating for a range ness, frequent traveling, and overeating. of pH in the stomach before and after a meal, and for varia- tions in each individual Digestive Formula offers a three-step approach to the prevention and treatment of occasional indigestion. -

Natural Treatments for Digestive Disorders
5/15/2017 Natural Treatments for Digestive Disorders Susan Buckley RDN, CDE, CLT South Denver Cardiology Assoc. Guard Your Gut! Americans spend more than $942 million dollars on over-the-counter antacids, and a whopping $13.6 billion dollars on prescription acid suppressants each year $725 million is spent on laxative products each year in America The cost of irritable bowel syndrome in the United States has been estimated at $1.7-$10 billion in direct medical costs, with an additional $20 billion in indirect costs, for a total of $21.7-$30 billion Constipation is the most common gastrointestinal complaint in the United States! 1 5/15/2017 Do You Think We Have Gut Issues? Defining Digestive Health Good digestive health indicates an ability to process nutrients through properly functioning gastrointestinal organs, including the stomach, intestines, liver, pancreas, esophagus and gallbladder. Most people who are in good digestive health are of appropriate weight and don’t regularly experience symptoms like heartburn, gas, constipation, diarrhea, nausea or stomach pain. American Gastroenterology Gastroenterology Association 2 5/15/2017 Definition – Digestive Health Ability to digest, absorb and utilize nutrients Eliminate waste products efficiently Optimizes vitality, and resilience Appropriate weight is central theme Don't regularly experience bothersome digestive symptoms This state of well-being is achieved by: consuming a nutritious diet minimizing emotional stressors embracing physical activity Oriented to the prevention of chronic disease. Gut Brain Connection Both our gut and our brain originate early in the embryo from the same clump of tissue which divides during fetal development. During early fetal development both your “gut” (esophagus, stomach, small intestine and colon) and your primary brain started to develop from the same clump of embryonic tissue. -
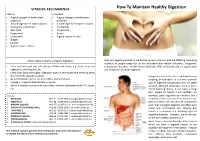
How to Maintain Healthy Digestion
VITAKIDS RECOMMENDS How To Maintain Healthy Digestion ADULTS CHILDREN • A good strength of multi-strain • A good strength of multi-strain probiotics probiotics • A multi-digestive enzyme complex • A multi-digestive enzyme complex • Zinc (with L-carnosine) • Chamomile • Aloe Vera • Peppermint • Peppermint • Ginger • Chamomile • A good source of Fiber • Ginger • Licorice • A good source of Fiber Other Lifestyle Tips for a Healthy Digestion: Oral and digestive problems are becoming very common and are affecting increasing numbers of people today due to our fast-paced and modern lifestyles. Indigestion, • Eat a well-balanced diet with plenty of fiber-rich foods, e.g. fresh fruits and constipation, diarrhea, Irritable Bowel Syndrome (IBS) and bad breath are typical signs vegetables, whole grains, etc. and symptoms of a poor digestion. • Chew your food thoroughly. Digestion starts in the mouth and chewing alerts the rest of the digestive system. Indigestion also refers to as abdominal pain, • Avoid stimulants such as alcohol, coffee, and spicy foods. bloating, or heartburn. It is a very common • Engage in a regular detoxification program. sign of digestive complication but it is often • Eat in a relaxed environment, one that is without distraction from TV, books, ignored. Although indigestion itself is not a etc. life-threatening illness, it can have a long- term impact on health if not rectified. For Find Us example, poor digestion can weaken one’s 1. PARAGON : #05-31 | 6733 3964 | [email protected] immunity as the nutrients from food are not 2. WESTGATE : #04-28 | 6465 9318 | [email protected] well absorbed. You may also be surprised to 3. -

Digestive Calm Patient Ed Sheet
Digestive Calm: Synergistic blend of herbal bitters to support healthy digestion* Digestive Calm is a powerful digestive support formula containing herbal bitters designed to optimize healthy digestion and help reduce occasional gastrointestinal discomfort after meals, such as gas, bloating, and excessive fullness.* This product is ideal for individuals who are sensitive to supplementation with hydrochloric acid (HCl, stomach acid) and for vegetarians and vegans who may benefit from digestive support but who prefer to avoid animal-sourced digestive enzymes. (Many digestive support products contain enzymes and bile of animal origin. Digestive Calm is completely free of these ingredients and contains solely plant-based compounds.) Proper digestive function lays the foundation for physical and mental health. The body is dependent on a steady supply of macro- and micronutrients (protein, fat, carbohydrate, vitamins and minerals) that must be liberated from the food you eat and then properly absorbed into the body. Proper timing, strength and secretion of stomach acid, gastric juices and pancreatic enzymes set the stage for effective nutrient absorption and also support immune function by neutralizing foodborne pathogens early in the digestive process. Hippocrates was close to the mark when he said that all disease begins in the gut, but actions in the intestines are influenced first by what occurs in the stomach. Digestive Calm features compounds with long histories of effective use in herbal and complementary medicine around the world: • -

Healthy Digestion & Weight Management
4 HEALTHY DIGESTION & WEIGHT MANAGEMENT When Lynette, 38, married her husband 12 years ago, she weighed 45 kg. Her weight went up to 50 kg after three years of careless eating habits and lack almost 60 kg. She felt tired all the time, and that extra weight on her slight build began to take a toll on her health and joints, especially her knees. Whenever was her weight gain. Over time, she grew very conscious about her weight. Initially, Lynette tried to lose weight through crash dieting and skipping meals, but these only made her hungrier, causing her to overeat. She also tried a drink marketed as “slimming tea”, but it gave her gastritis. Frustrated by one He advised her to make some lifestyle changes. Since then, she has been exercising regularly and eating healthily, even treating herself to her favourite local dish, laksa, occasionally. To avoid having to rely overmuch on oils, fats or to jazz up her cooking. With these sensible changes, Lynette’s weight went down to a healthy 52 kg over the course of one and a half years. She looks great, Maintaining a healthy weight and has never felt better in her life. is part and parcel of your health and wellness 42 BEAUTIFUL INSIDE OUT 43 UNDERSTANDING DIGESTION Just before the food passes into the stomach, it Digestion is the process of breaking down the food we Believe It Or Not! passes through a ring-shaped muscle called the eat into energy. These nutrients are absorbed into the lower oesophageal sphincter (LES). The LES relaxes bloodstream and carried all over the body to nourish Depending on the age and size to allow food to pass through to the stomach. -

Healthy Digestion
SELINSGROVE AREA HIGH SCHOOL SEALS Health News VOLUME III, ISSUE 7 M A R C H 2 0 1 9 Healthy Digestion Good (healthy) digestion is a 'silent' process - digestion in some form is taking place while we rest, eat, sleep or work. We generally only be- come aware of digestion when something goes wrong (eg, if you eat foods that don't agree with your body or drink too much alcohol or say, if you become constipated or have gas). Although the digestive system can withstand a lot of stress (from the foods you eat to emotional stresses), it can only do so for a limited pe- riod. Over time, the negative effects will accumulate and create health problems in the long-term. So irrespective of your lifestyle in the past, you can take some positive steps today to rejuvenate and maintain the health of your digestive system. Maintaining a healthy digestive system - key points Eat a healthy diet Eat moderately, slowly and regularly Exercise regularly Reduce/manage stress levels Quit smoking P A G E 2 Wash your Your Digestive System & How it Works hands well af- What is the digestive system? ter using the bathroom, AND The digestive system is made up of the gastrointestinal tract—also called the leave your GI tract or digestive tract—and the liver, pancreas, and gallbladder. The GI tract is a series of hollow organs joined in a long, twisting tube from the phone out of mouth to the anus. The hollow organs that make up the GI tract are the the bathroom! mouth, esophagus, stomach, small intestine, large intestine, and anus. -

Guard Your Gut!
4/16/2015 Guard Your Gut! Richard Collins, MD Susan Buckley RDN, CDE South Denver Cardiology Assoc. Guard Your Gut! Americans spend more than $942 million dollars on over-the-counter antacids, and a whopping 13.6 billion dollars on prescription acid suppressants each year $725 million is spent on laxative products each year in America The cost of irritable bowel syndrome in the United States has been estimated at $1.7-$10 billion in direct medical costs, with an additional $20 billion in indirect costs, for a total of $21.7-$30 billion Constipation is the most common gastrointestinal complaint in the United States! 1 4/16/2015 Do You Think We Have Gut Issues? Defining Digestive Health Good digestive health indicates an ability to process nutrients through properly functioning gastrointestinal organs, including the stomach, intestines, liver, pancreas, esophagus and gallbladder. Most people who are in good digestive health are of appropriate weight and don’t regularly experience symptoms like heartburn, gas, constipation, diarrhea, nausea or stomach pain. American Gastroenterology Association 2 4/16/2015 Definition – Digestive Health Ability to digest, absorb and utilize nutrients Eliminate waste products Optimizes vitality, and resilience Appropriate weight is central theme Don't regularly experience bothersome digestive symptoms This state of well-being is achieved by: consuming a nutritious diet minimizing emotional stressors embracing physical activity Oriented to the prevention of chronic disease. Gut Brain Connection Both our gut and our brain originate early in the embryo from the same clump of tissue which divides during fetal development. During early fetal development both your “gut” (esophagus, stomach, small intestine and colon) and your primary brain started to develop from the same clump of embryonic tissue.