Immune-Modulators to Combat Hepatitis B Virus Infection: From
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Porvac® Subunit Vaccine E2-CD154 Induces Remarkable Rapid Protection Against Classical Swine Fever Virus
Article Porvac® Subunit Vaccine E2-CD154 Induces Remarkable Rapid Protection against Classical Swine Fever Virus Yusmel Sordo-Puga 1, Marisela Suárez-Pedroso 1 , Paula Naranjo-Valdéz 2, Danny Pérez-Pérez 1, Elaine Santana-Rodríguez 1, Talia Sardinas-Gonzalez 1, Mary Karla Mendez-Orta 1, Carlos A. Duarte-Cano 1, Mario Pablo Estrada-Garcia 1 and María Pilar Rodríguez-Moltó 1,* 1 Animal Biotechnology Department, Center for Genetic Engineering and Biotechnology, P.O. Box 6162, Havana 10600, Cuba; [email protected] (Y.S.-P.); [email protected] (M.S.-P.); [email protected] (D.P.-P.); [email protected] (E.S.-R.); [email protected] (T.S.-G.); [email protected] (M.K.M.O.); [email protected] (C.A.D.); [email protected] (M.P.E.) 2 Central Laboratory Unit for Animal Health (ULCSA), Havana 11400, Cuba; [email protected] * Correspondence: [email protected]; Tel.: +53-7-2504419 Abstract: Live attenuated C-strain classical swine fever vaccines provide early onset protection. These vaccines confer effective protection against the disease at 5–7 days post-vaccination. It was previously reported that intramuscular administration of the Porvac® vaccine protects against highly virulent Citation: Sordo-Puga, Y.; classical swine fever virus (CSFV) “Margarita” strain as early as seven days post-vaccination. In Suárez-Pedroso, M.; Naranjo-Valdéz, order to identify how rapidly protection against CSFV is conferred after a single dose of the Porvac® P.; Pérez-Pérez, D.; subunit vaccine E2-CD154, 15 swine, vaccinated with a single dose of Porvac®, were challenged Santana-Rodríguez, E.; 3 intranasally at five, three, and one day post-vaccination with 2 × 10 LD50 of the highly pathogenic Sardinas-Gonzalez, T.; Mendez-Orta, Cuban “Margarita” strain of the classical swine fever virus. -

Current Therapies for Chronic Hepatitis C
Southern Illinois University Edwardsville SPARK Pharmacy Faculty Research, Scholarship, and Creative Activity School of Pharmacy 1-2011 Current Therapies for Chronic Hepatitis C McKenzie C. Ferguson Southern Illinois University Edwardsville, [email protected] Follow this and additional works at: https://spark.siue.edu/pharmacy_fac Part of the Pharmacy and Pharmaceutical Sciences Commons Recommended Citation Ferguson, McKenzie C., "Current Therapies for Chronic Hepatitis C" (2011). Pharmacy Faculty Research, Scholarship, and Creative Activity. 4. https://spark.siue.edu/pharmacy_fac/4 This Article is brought to you for free and open access by the School of Pharmacy at SPARK. It has been accepted for inclusion in Pharmacy Faculty Research, Scholarship, and Creative Activity by an authorized administrator of SPARK. For more information, please contact [email protected],[email protected]. Chronic Hepatitis C & Current Therapies 1 Review of Chronic Hepatitis C & Current Therapies Reviews of Therapeutics Pharmacotherapy McKenzie C. Ferguson, Pharm.D., BCPS From the School of Pharmacy, Southern Illinois University Edwardsville, Department of Pharmacy Practice, Edwardsville, Illinois. Address for reprint requests : Southern Illinois University Edwardsville School of Pharmacy 220 University Park Drive, Ste 1037 Edwardsville, IL 62026-2000 Email: [email protected] Keywords : hepatitis C, HCV, ribavirin, interferon, peginterferon alfa-2a, peginterferon alfa-2b, albinterferon, taribavirin, telaprevir, therapeutic efficacy, safety The author received no sources of support in the form of grants, equipment, or drugs. Chronic Hepatitis C & Current Therapies 2 ABSTRACT Hepatitis C virus affects more than 180 million people worldwide and as many as 4 million people in the United States. Given that most patients are asymptomatic until late in disease progression, diagnostic screening and evaluation of patients that display high-risk behaviors associated with acquisition of hepatitis C should be performed. -

THE CONCISE GUIDE to PHARMACOLOGY 2017/18 Alexander, Stephen P
University of Dundee THE CONCISE GUIDE TO PHARMACOLOGY 2017/18 Alexander, Stephen P. H.; Fabbro, Doriano; Kelly, Eamonn; Marrion, Neil V.; Peters, John A.; Faccenda, Elena Published in: British Journal of Pharmacology DOI: 10.1111/bph.13876 Publication date: 2017 Licence: CC BY Document Version Publisher's PDF, also known as Version of record Link to publication in Discovery Research Portal Citation for published version (APA): Alexander, S. P. H., Fabbro, D., Kelly, E., Marrion, N. V., Peters, J. A., Faccenda, E., Harding, S. D., Pawson, A. J., Sharman, J. L., Southan, C., Davies, J. A., & CGTP Collaborators (2017). THE CONCISE GUIDE TO PHARMACOLOGY 2017/18: Catalytic receptors. British Journal of Pharmacology, 174 (Suppl. 1), S225-S271. https://doi.org/10.1111/bph.13876 General rights Copyright and moral rights for the publications made accessible in Discovery Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from Discovery Research Portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain. • You may freely distribute the URL identifying the publication in the public portal. Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Download date: 23. Sep. 2021 S.P.H. -

Antigen-Specific Induced Foxp3 Regulatory T Cells Are Generated
Antigen-specific induced Foxp3+ regulatory T cells are generated following CD40/CD154 blockade Ivana R. Ferrer, Maylene E. Wagener, Minqing Song, Allan D. Kirk, Christian P. Larsen, and Mandy L. Ford1 Emory Transplant Center and Department of Surgery, Emory University, Atlanta, GA 30322 Edited by James P. Allison, Memorial Sloan-Kettering Cancer Center, New York, NY, and approved November 4, 2011 (received for review April 7, 2011) Blockade of the CD40/CD154 pathway potently attenuates T-cell in vivo accumulation of Treg and deletion of graft-specific ef- responses in models of autoimmunity, inflammation, and trans- fectors after CD40/CD154 blockade has not been investigated. plantation. Indeed, CD40 pathway blockade remains one of the To address these questions, we used an ovalbumin (OVA)- most powerful methods of prolonging graft survival in models of expressing transgenic mouse model (20), which allowed us to di- + + transplantation. But despite this effectiveness, the cellular and rectly track both donor-reactive CD4 and CD8 T-cell responses molecular mechanisms underlying the protective effects of CD40 simultaneously over time. Although previous studies have used pathway blockade are incompletely understood. Furthermore, the transgenic models to assess the degree of T-cell deletion after CD154/CD40 blockade (16, 21), none has systematically inter- relative contributions of deletion, anergy, and regulation have not + been measured in a model in which donor-reactive CD4+ and CD8+ rogated the impact of anti-CD154 on the kinetics of both CD4 and CD8+ T-cell deletion and acquisition of effector function. T-cell responses can be assessed simultaneously. To investigate the fi Our results indicated that although CD40/CD154 blockade alone impact of CD40/CD154 pathway blockade on graft-speci c T-cell delayed donor-reactive CD4+ and CD8+ T-cell expansion and responses, a transgenic mouse model was used in which recipients differentiation, the addition of DST was required for antigen- fi + + containing ovalbumin-speci cCD4 and CD8 TCR transgenic T specific T-cell deletion. -

Interferon Gamma Release Assay (IGRA) Interferon Gamma Release Assay (IGRA) Is a Blood Test That Has Recently Been Introduced As Another Method to Diagnose LTBI
Section 4: TB Screening These cases also included patients that did not have previous exposure to tuberculin. It is imperative that health care providers should have Epinephrine Hypochloride solution (1:1000) and other appropriate agents available for immediate use in the case of a hypersensitivity reaction. As per NACI, recommendations all patients must be monitored for 15 minutes after inoculation. Interferon Gamma Release Assay (IGRA) Interferon gamma release assay (IGRA) is a blood test that has recently been introduced as another method to diagnose LTBI. Therefore, it can complement the TST in certain situations. In general, IGRAs are more specific than the TST in populations vaccinated with BCG, especially if BCG is given after infancy or multiple times. When a person is exposed to MTB it produces many immune cells, which produce various proteins. Among these proteins are interferon gamma or IFN-y. The interferon gamma release assay (IGRA) is a blood test that measures IFN-y. Therefore, if a person has been exposed and infected with TB, IFN-y can be detected with this test. There are two IGRA tests used in Canada, the T-SPOT.TB test and the QuantiFERON®-TB Gold test. Provincial Laboratory (ProvLab) Alberta uses QuantiFERON®-TB Gold (QFT) test in the NWT. Specimens must be received by the regional laboratory and incubated for 16–24 hours. This limits availability of this test in the NWT. IGRA can only be ordered through the Office of the Chief Public Health Officer and Stanton Regional Hospital Specialists who are involved in TB management and treatment. IGRAs require laboratories with adequate equipment and trained personnel to perform the assays. -

Interferon-Based Biopharmaceuticals: Overview on the Production, Purification, and Formulation
Review Interferon-Based Biopharmaceuticals: Overview on the Production, Purification, and Formulation Leonor S. Castro 1,†, Guilherme S. Lobo 1,†, Patrícia Pereira 2 , Mara G. Freire 1 ,Márcia C. Neves 1,* and Augusto Q. Pedro 1,* 1 CICECO–Aveiro Institute of Materials, Chemistry Department, University of Aveiro, Campus Universitário de Santiago, 3810-193 Aveiro, Portugal; [email protected] (L.S.C.); [email protected] (G.S.L.); [email protected] (M.G.F.) 2 Centre for Mechanical Engineering, Materials and Processes, Department of Chemical Engineering, University of Coimbra, Rua Sílvio Lima-Polo II, 3030-790 Coimbra, Portugal; [email protected] * Correspondence: [email protected] (M.C.N.); [email protected] (A.Q.P.) † These authors contributed equally to this work. Abstract: The advent of biopharmaceuticals in modern medicine brought enormous benefits to the treatment of numerous human diseases and improved the well-being of many people worldwide. First introduced in the market in the early 1980s, the number of approved biopharmaceutical products has been steadily increasing, with therapeutic proteins, antibodies, and their derivatives accounting for most of the generated revenues. The success of pharmaceutical biotechnology is closely linked with remarkable developments in DNA recombinant technology, which has enabled the production of proteins with high specificity. Among promising biopharmaceuticals are interferons, first described by Isaacs and Lindenmann in 1957 and approved for clinical use in humans nearly thirty years later. Interferons are secreted autocrine and paracrine proteins, which by regulating several biochemical Citation: Castro, L.S.; Lobo, G.S.; pathways have a spectrum of clinical effectiveness against viral infections, malignant diseases, Pereira, P.; Freire, M.G.; Neves, M.C.; and multiple sclerosis. -

2010 Hepatitis C Treatment Updates
2010 Hepatitis C Treatment Updates Summer 2010 Treatment Options Conventional Interferon Alone (Monotherapy) Studies in adults have demonstrated that monotherapy with conventional interferon is effective for adults 10-15% of the time. Although children typically respond better than adults to this treatment (27% for genotype 1 and 71% for genotype 2 and 3), subsequent study has confirmed that using conventional interferon in combination with ribavirin produces better treatment outcomes for both adults and children. Thus, conventional interferon alone is no longer recommended for the majority of children requiring HCV therapy. Conventional Interferon Alpha-2b in Combination with Ribavirin (Rebetron for Children) Rebetron was the first drug to be FDA-approved to treat children with hepatitis C. It’s approved for use in children between the ages of 5 and 16 years. Rebetron is a combination drug that contains both Intron A (an interferon alfa-2b) and Rebetol (which is ribavirin). Rebetron is administered as a weight-based dose of oral Rebetol that is taken twice a day. (Rebetol should never be used alone to treat hepatitis C.) The Intron A portion of the treatment is a subcutaneous injection that is given three times weekly for 24 to 48 weeks. Sometimes, problems with anemia or depression can develop with this treatment. When this occurs, doses should be reduced temporarily or permanently until the problem is reversed. Additionally, if uncontrollable thyroid abnormalities (such has hypothyroidism) occur, treatment should be discontinued. Use of conventional interferon alpha-2b in combination with ribavirin has been shown to improve treatment outcomes in adults when compared to using conventional interferon alone. -
High Sensitivity Immunoassays for Detecting Ifn-Gamma in Cytokine Release Syndrome
APPLICATION NOTE HIGH SENSITIVITY IMMUNOASSAYS FOR DETECTING IFN-GAMMA IN CYTOKINE RELEASE SYNDROME INTRODUCTION T cell expansion with increased Interferon Gamma (IFN-γ) release. Note that increased IFN-γ is also an early and prominent element of CRS. IFN , along with IL-6, IL-10 and TNF-alpha are the Cytokine Release Syndrome (CRS), also known as the “Cytokine -γ core cytokines involved in CRS (2). IFN activates macrophages Storm”, is a systemic inflammatory response characterized at the -γ which secrete excessive amounts of other cytokines such as cellular level by the rapid release of excessive concentrations IL-6, TNF and IL-10. Lastly, it is important to keep in mind that of cytokines (1,2). Patient symptoms range from mild fever to α IFN is pleiotropic and has both harmful and beneficial effects. hypotension, multiorgan system failure, neurotoxicity and death. -γ Although IFN has a harmful role in CRS, it also been correlated CRS is caused by a variety of events, including viral infection, -γ with antiproliferative, proapoptotic and antitumor activities in the antibody-based immunotherapy and cellular immunotherapy. context of cancer (4). In antibody-based immunotherapies, the incidence of CRS is relatively low, however, onset can occur within days and up to We previously described the new 3rd generation R&D Systems® weeks of infusion in cellular immunotherapy. Evidence suggests IFN-γ Quantikine® ELISA kit. Learn more about that assay here. that the risk and severity of CRS is influenced by the type of Here, we describe the R&D Systems® Human IFN-γ Quantikine® therapy, disease burden and patient characteristics, such as age. -

Quantum of Effectiveness Evidence in FDA's Approval of Orphan Drugs
Quantum of Effectiveness Evidence in FDA’s Approval of Orphan Drugs Cataloguing FDA’s Flexibility in Regulating Therapies for Persons with Rare Disorders by Frank J. Sasinowski, M.S., M.P.H., J.D.1 Chairman of the Board National Organization for Rare Disorders One of the key underlying issues facing the development of effective for their intended uses. all drugs, and particularly orphan drugs, is what kind of evi- dence the Food and Drug Administration (FDA) requires for FDA has for many decades acknowledged that there is a need approval. The Federal Food, Drug, and Cosmetic [FD&C] Act IRUÁH[LELOLW\LQDSSO\LQJLWVVWDQGDUGIRUDSSURYDO)RUH[- provides that for FDA to grant approval for a new drug, there ample, one of FDA’s regulations states that: “FDA will ap- must be “substantial evidence” of effectiveness derived from prove an application after it determines that the drug meets the “adequate and well-controlled investigations.” This language, statutory standards for safety and effectiveness… While the which dates from 1962, provides leeway for FDA medical re- statutory standards apply to all drugs, the many kinds of drugs viewers to make judgments as to what constitutes “substantial that are subject to the statutory standards and the wide range HYLGHQFHµRIDGUXJ·VHIIHFWLYHQHVVWKDWLVRILWVEHQHÀWWR RIXVHVIRUWKRVHGUXJVGHPDQGÁH[LELOLW\LQDSSO\LQJWKHVWDQ- patients. GDUGV7KXV)'$LVUHTXLUHGWRH[HUFLVHLWVVFLHQWLÀFMXGJPHQW to determine the kind and quantity of data and information an 7KHVROHODZWKDWDSSOLHVVSHFLÀFDOO\WRRUSKDQGUXJVWKH2U- applicant is required to provide for a particular drug to meet SKDQ'UXJ$FWRISURYLGHGÀQDQFLDOLQFHQWLYHVIRUGUXJ the statutory standards.” 21 C.F.R. § 314.105(c). FRPSDQLHVWRGHYHORSRUSKDQGUXJVZKLFKLVOHJDOO\GHÀQHG as products that treat diseases that affect 200,000 or fewer )'$SXEOLFO\KDVH[SUHVVHGVHQVLWLYLW\WRDSSO\LQJWKLVÁH[- patients in the U.S. -
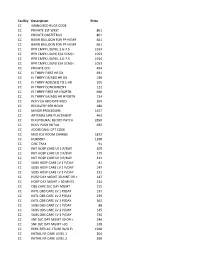
NMMC West Point CDM.Xlsx
Facility Description Price CC SWING BED RUGS CODE CC PRIVATE 1ST WEST 861 CC PRIVATE OBSTETRICS 861 CC BAKRI BALLOON FOR PP HEMR 661 CC BAKRI BALLOON FOR PP HEMR 661 CC RPR CMPX LID/N/L 2.6‐7.5 1914 CC RPR CMPX LID/N/ E/A 5CM/< 1053 CC RPR CMPX LID/N/L 2.6‐7.5 1914 CC RPR CMPX LID/N/ E/A 5CM/< 1053 CC PRIVATE ECU 494 CC IV THRPY FIRST HR DX 691 CC IV THRPY EA/ADD HR DX 190 CC IV THRPY ADD/SEQ TO 1 HR 205 CC IV THRPY CONCURRENT 122 CC IV THRPY FIRST HR HYDRTN 690 CC IV THRPY EA/ADD HR HYDRTN 134 CC INJ IV EA ADD DIFF MED 269 CC RECOVERY PER HOUR 280 CC MINOR PROCEDURE 1627 CC ARTERIAL LINE PLACEMENT 463 CC INJ EPIDURAL BLOOD PATCH 2850 CC INJ IV PUSH INITIAL 692 CC ADDITIONAL CPT CODE CC MED ICU ROOM CHARGE 1872 CC NURSERY 1200 CC CIRC TRAY 91 CC INIT HOSP CARE LV 1 P/DAY 205 CC INIT HOSP CARE LV 2 P/DAY 279 CC INIT HOSP CARE LV 3 P/DAY 412 CC SUBS HOSP CARE LV 1 P/DAY 81 CC SUBS HOSP CARE LV 2 P/DAY 147 CC SUBS HOSP CARE LV 3 P/DAY 212 CC HOSP DAY MGMT 30 MNT OR < 147 CC HOSP DAY MGMT > 30 MNTS 214 CC OBS CARE D/C DAY MGMT 155 CC INITL OBS CARE LV 1 P/DAY 197 CC INITL OBS CARE LV 2 P/DAY 239 CC INITL OBS CARE LV 3 P/DAY 362 CC SUBS OBS CARE LV 1 P/DAY 88 CC SUBS OBS CARE LV 2 P/DAY 145 CC SUBS OBS CARE LV 3 P/DAY 236 CC SNF D/C DAY MGMT 30 OR < 240 CC SNF D/C DAY MGMT >30 318 CC PERC REPLAC J TUBE W/O FL 1948 CC INITIAL NF CARE LEVEL 1 204 CC INITIAL NF CARE LEVEL 2 290 CC INITIAL NF CARE LEVEL 3 368 CC SUBSQENT NF CARE LEVEL 197 CC SUBSQENT NF CARE LEVEL 2 151 CC SUBSQENT NF CARE LEVEL 3 198 CC SUBSQENT NF CARE LEVEL 4 295 CC OBS OR I/P -

Monitoring and Mathematical Modeling of in Vitro Human Megakaryocyte Expansion and Maturation Dynamics
YOUNES LEYSI-DERILOU MONITORING AND MATHEMATICAL MODELING OF IN VITRO HUMAN MEGAKARYOCYTE EXPANSION AND MATURATION DYNAMICS Thèse présentée à la Faculté des études supérieures de l’Université Laval dans le cadre du programme de doctorat en génie chimique pour l’obtention du grade de Philosophiae doctor (Ph.D.) DEPARTMENT DE GÉNIE CHIMIQUE FACULTÉ DE SCIENCES ET GÉNIE UNIVERSITÉ LAVAL QUÉBEC 2011 © Younes Leysi-Derilou, 2011 ii Résumé La mégakaryopoïèse est un processus complexe, qui prend naissance à partir des cellules souches hématopoïétiques (HSC). Ces dernières se différencient par étapes successives en mégakaryocytes (MKs) qui, suite à leur maturation, libèrent les plaquettes. Afin de modéliser le sort des HSCs lors de la mégakaryopoïèse en culture, un nouveau modèle mathématique a été développé, basé sur un programme de différenciation tridimensionnelle (3-D) où chaque sous-population est représentée par un compartiment. Dans le but d’évaluer la prolifération, la différenciation des MKs immatures puis matures, la cinétique de mort cellulaire ainsi que le nombre de plaquettes produites, à partir des cellules de sang de cordon (CB) ombilical enrichies en CD34+, un ensemble d'équations différentielles a été déployé. Les cellules CD34+ ont été placées en culture dans un milieu optimisé pour la différenciation mégakaryocytaire. Les paramètres cinétiques ont été estimés pour deux températures d'incubation (37°C versus 39°C). Les résultats des régressions ont été validés par l'évaluation de l'estimabilité des paramètres, en utilisant des analyses de sensibilité locale et globale, puis la détermination d'un intervalle de confiance. Ceux-ci ont été comparés par le biais de tests statistiques et d’analyses en composante principale (ACP). -

7 Engineering of Therapeutic Proteins
Engineering of 7 Therapeutic Proteins Fei Wen, Sheryl B. Rubin-Pitel, and Huimin Zhao CONTENTS Protein Therapeutics versus Small Molecule Drugs .............................................. 154 Sources of Protein Therapeutics ................................................................... 155 Targets of Protein Therapeutics and Modes of Action .................................. 155 Engineering Effective Protein Therapeutics .......................................................... 156 Challenges in Pharmaceutical Translation of New Therapeutic Proteins ..... 156 Strategies for Designing Effective Protein Therapeutics .............................. 156 Strategies for Improving Pharmacokinetics ...................................... 157 Strategies for Reducing Immunogenicity ......................................... 158 Genetic Engineering ......................................................................... 159 Examples of Protein Therapeutics ......................................................................... 160 Monoclonal Antibody Therapeutics.............................................................. 161 Enzyme Therapeutics Acting on Extracellular Targets ................................. 161 Protein Therapeutics as Replacements for Defective or Deficient Proteins .....162 Protein Hormones ............................................................................. 162 Coagulation Factors .......................................................................... 163 Enzyme Replacement Therapy ........................................................