Institutional Review Board Policies and Procedures Effective January 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Occupational Therapy Code of Ethics and Ethics Standards (2010)
Occupational Therapy Code of Ethics and Ethics Standards (2010) PREAMBLE The American Occupational Therapy Association (AOTA) Occupational Therapy Code of Ethics and Ethics Standards (2010) ("Code and Ethics Standards") is a public statement of principles used to promote and maintain high standards of conduct within the profession. Members of AOTA are committed to promoting inclusion, diversity, independence, and safety for all recipients in various stages of life, health, and illness and to empower all beneficiaries of occupational therapy. This commitment extends beyond service recipients to include professional colleagues, students, educators, businesses, and the community. Fundamental to the mission of the occupational therapy profession is the therapeutic use of everyday life activities (occupations) with individuals or groups for the purpose of participation in roles and situations in home, school, workplace, community, and other settings. "Occupational therapy addresses the physical, cognitive, psychosocial, sensory, and other aspects of performance in a variety of contexts to support engagement in everyday life activities that affect health, well being, and quality of life" AOTA, 2004). Occupational therapy personnel have an ethical responsibility primarily to recipients of service and secondarily to society. The Occupational Therapy Code of Ethics and Ethics Standards (2010) was tailored to address the most prevalent ethical concerns of the profession in education, research, and practice. The concerns of stakeholders including the public, consumers, students, colleagues, employers, research participants, researchers, educators, and practitioners were addressed in the creation of this document. A review of issues raised in ethics cases, member questions related to ethics, and content of other professional codes of ethics were utilized to ensure that the revised document is applicable to occupational therapists, occupational therapy assistants, and students in all roles. -

Human Challenge Trials for Vaccine Development: Regulatory Considerations
POST ECBS Version ENGLISH ONLY EXPERT COMMITTEE ON BIOLOGICAL STANDARDIZATION Geneva, 17 to 21 October 2016 Human Challenge Trials for Vaccine Development: regulatory considerations © World Health Organization 2016 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; email: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. -

Informed Consent and Refusal
CHAPTER 3 Informed Consent and Refusal Evolution of the doctrine of informed consent Elements of informed consent and refusal The nature of informed consent Exceptions to the consent requirement Mrs. Stack is a 67- year- old woman admitted with rectal bleeding, chronic renal in- sufficiency, diabetes, and blindness. On admission, she was alert and capacitated. Two weeks later, she suffered a cardiopulmonary arrest, was resuscitated and intu- bated, and was transferred to the medical intensive care unit (MICU) in an unrespon- sive and unstable state. Consent for emergency dialysis was obtained from her son, who is also her health care agent. Dialysis was repeated two days later. During the past several years, Mrs. Stack has consistently stated to her family and her primary care doctor that she would never want to be on chronic dialysis and she has refused it numerous times when it was recommended. The physician, who has known and treated Mrs. Stack for many years, also treated her daughter who had been on chronic dialysis for some time and had died after suffering a heart attack. According to the physician and the patient’s family, Mrs. Stack’s refusal of dialysis has been based on her conviction that her daughter died as a result of the dialysis treatments. Mrs. Stack’s mental status has cleared considerably and, despite the ventilator, she is able to communicate nonverbally. Although she appears to understand the benefits of dialysis and the consequences of refusing it, including deterioration and eventual death, she has consistently and vehemently refused further treatments. Her capacity to make this decision is not now in question. -

The Implications of Religious Beliefs on Medical and Patient Care
University of Pennsylvania ScholarlyCommons Master of Science in Organizational Dynamics Theses Organizational Dynamics Programs 11-14-2011 The Implications of Religious Beliefs on Medical and Patient Care Dana I. Al Husseini University of Pennsylvania, [email protected] Follow this and additional works at: https://repository.upenn.edu/od_theses_msod Al Husseini, Dana I., "The Implications of Religious Beliefs on Medical and Patient Care" (2011). Master of Science in Organizational Dynamics Theses. 46. https://repository.upenn.edu/od_theses_msod/46 Submitted to the Program of Organizational Dynamics in the Graduate Division of the School of Arts and Sciences in Partial Fulfillment of the Requirements for the Degree of Master of Science in Organizational Dynamics at the University of Pennsylvania Advisor: Adrian Tschoegl This paper is posted at ScholarlyCommons. https://repository.upenn.edu/od_theses_msod/46 For more information, please contact [email protected]. The Implications of Religious Beliefs on Medical and Patient Care Abstract Throughout history and to this date in a continuously globalized world, monotheistic religions and medicine have caused numerous acrimonious debates especially in crucial moments of life and death. Medical and nursing staff working with patients from different religions in any country in the world must adhere to and respect those patients’ faiths and be aware of them to provide better patient care and in worst case scenarios, avoid litigation. Furthermore, this paper should not to be treated as an encyclopedic reference; it is merely a general overview into the three monotheistic faiths to alert professional healthcare staff of the possibility of a religious implication even if it contradicts their own concerns and points of views. -
Informed Consent
Christine Grady Department of Bioethics NIH Clinical Center The views expressed here are mine and do not necessarily represent those of the CC, NIH, or Department of Health and Human Services Informed consent is the bedrock principle on which most of modern research ethics rest…This was at the heart of the crucial ethical provision stated in the first words of the Nuremberg Code, and it remains equally compelling a half century later. Menikoff J, Camb Quarterly 2004 p 342 Authorization of an activity based on understanding what the activity entails. A legal, regulatory, and ethical requirement in health care and in most research with human subjects A process of reasoned decision making (not a form or an episode) One aspect of conducting ethical clinical research “Every human being of adult years and sound mind has a right to determine what will be done with his body… Justice Cardozo, 1914 Respect for autonomy or for an individual’s capacity and right to define own goals and make choices consistent with those goals. Well entrenched in American values, jurisprudence, medical practice, and clinical research. “Informed consent is rooted in the fundamental recognition…that adults are entitled to accept or reject health care interventions on the basis of their own personal values and in furtherance of their own personal goals” Presidents Commission for the study of ethical problems…1982 Informed consent in medical practice …informed consent in clinical practice is frequently inadequate… Physicians receive little training… Misunderstand requirements and legal standards… Time pressures and competing demands… Patient comprehension is often poor… Recent studies have demonstrated improvement in patient understanding of risks after communication interventions Schenker et al 2010; Matiasek et al. -

Informed Consent for Participation in Personal Training
PRINCETON UNIVERSITY Personal Training INFORMED CONSENT FOR PARTICIPATION IN PERSONAL TRAINING Name: ________________________ 1. Purpose and Explanation of Procedure I desire to participate voluntarily in an acceptable plan of exercise conditioning. I also desire to be placed in program activities which are recommended to me for improvement of my general health and well-being in which I will be given exact instructions regarding the amount and kind of exercise I should do. Professionally trained personnel will provide leadership to direct my activities, monitor my performance and otherwise evaluate my effort. Depending upon my health status, I may or may not be required to have my heart rate evaluated during these sessions and/or regulate my exercise within desired limits. I understand that I am expected to follow staff instructions with regard to the proper performance of each exercise. I have been advised and understand it is recommended that I obtain a medical examination by a physician before I participate in this program. The medical examination is highly suggested in order to identify conditions which may preclude participation. If I am taking prescribed medications, I have already so informed the program staff and further agree to inform them promptly of any changes which my doctor or I may make with regard to such use. I have been informed that during my participation in exercise, I will be asked to complete the physical activities unless such symptoms as fatigue, shortness of breath, chest discomfort or similar occurrences appear. At that point, I have been advised it is my complete right and responsibility to decrease or stop exercising and that it is my obligation to inform the program personnel of my symptoms. -

Biobanks for Europe
KI-NA-25-302-EN-C This expert group report on the ethical and regulatory challenges of international biobank research has been authored by an interdisciplinary group with experts from science, law, governance and ethics. Biobanks for Biobank research is rapidly evolving, and in close interaction with developments in informatics and genomics. The size and breath of the collections of biological samples and associated data that can be Europe assembled has increased exponentially. This opens up a vast range of new options for research and diagnosis, but at the same time also holds an important challenge for the governance of these activities. In this report, the expert group makes speci c recommendations for good A Challenge for Governance governance of Biobanks Research and Innovation policy Research and Innovation ed205134cover_BAT.indd 1-3 11/06/12 09:14 How to obtain EU publications Free publications: • via EU Bookshop (http://bookshop.europa.eu); • at the European Union’s representations or delegations. You can obtain their contact details on the Internet (http://ec.europa.eu) or by sending a fax to +352 2929-42758. Priced publications: • via EU Bookshop (http://bookshop.europa.eu). Priced subscriptions (e.g. annual series of the O cial Journal of the European Union and reports of cases before the Court of Justice of the European Union): • via one of the sales agents of the Publications O ce of the European Union (http://publications.europa.eu/others/agents/index_en.htm). EUROPEAN COMMISSION Directorate-General for Research and Innovation Directorate B — European Research Area Unit B6 — Ethics and gender Contact: Lino PAULA European Commission B-1049 Brussels E-mail: [email protected] ed205134cover_BAT.indd 4-6 11/06/12 09:14 EUROPEAN COMMISSION Biobanks for Europe A challenge for governance Report of the Expert Group on Dealing with Ethical and Regulatory Challenges of International Biobank Research Chair: Herbert Gottweis Rapporteur: Jane Kaye Members: Fabrizia Bignami, Emmanuelle Rial-Sebbag, Roberto Lattanzi, Milan Macek Jr. -
TWU IRB Reference Sheet for Recruitment and Informed Consent
TWU IRB Reference Sheet for Recruitment and Informed Consent RECRUITMENT Recruitment Materials (flyers, email scripts, social media posts, etc.) • Items that are required: • State that research will be conducted • State that participation is voluntary • If the internet/email is used for participation, include the following statement: “There is a potential risk of loss of confidentiality in all email, downloading, electronic meetings, and internet transactions.” • Items that are NOT required, but recommended: • PI’s contact information (email is recommended over cell phone #, but both are okay) • Location/site of the study • Study title • Brief description of the study • If using a TWU logo, TWU marketing is asking that you use the new logo • Main eligibility requirements • Benefits for participation • Total time commitment • If your scripts will vary across different platforms (email script, social media post, phone script, etc.), make sure you attach all appropriate scripts. If you are using the same script across all platforms, state so. • Make sure the information you include is consistent with the information you provide in the application and consent form. • Remember, it is okay to leave out details that are subject to change (e.g., study or session dates, gift card vendors). It is very possible that your study will not start when you want it to. If you leave out actual dates, you will not need to submit a modification request to change it later. The same thing goes with gift cards. If your study is funded, you may work with ORSP to get gift cards. You may need 40 $5 gift cards, but they do not have 40 from the same vendor. -
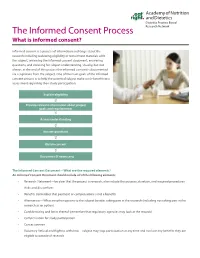
The Informed Consent Process Research Network What Is Informed Consent?
Dietetics Practice Based The Informed Consent Process Research Network What is informed consent? Informed consent is a process of information exchange about the research including reviewing eligibility or recruitment materials with the subject, reviewing the informed consent document, answering questions, and checking for subject understanding. Usually, but not always, at the end of this process the informed consent is documented via a signature from the subject. One of the main goals of the informed consent process is to help the potential subject make a risk-benefit ratio assessment regarding their study participation. Explain eligibility Provide relevant information about project goals and requirements Assess understanding Answer questions Obtain consent Document (if necessary) The Informed Consent Document—What are the required elements? An Informed Consent Document should include all of the following elements: • Research Statement—be clear that the project is research, also include the purpose, duration, and required procedures • Risks and discomforts • Benefits (remember that payment or compensation is not a benefit) • Alternatives—What are other options to the subject besides taking part in the research (including not taking part in the research as an option) • Confidentiality and limits thereof (remember that regulatory agencies may look at the records) • Compensation for study participation • Contact person • Voluntary Refusal and Right to withdraw—subject may stop participation at any time and not lose any benefits they are -

A Comparison of Two Bioethical Theories
A Comparison of Two Bioethical Theories A thesis presented to the faculty of the College of Arts and Sciences of Ohio University In partial fulfillment of the requirements for the degree Master of Arts Gavin G. Enck June 2009 © 2009 Gavin G. Enck. All Rights Reserved. 2 This thesis titled A Comparison of Two Bioethical Theories by GAVIN G. ENCK has been approved for the Department of Philosophy and the College of Arts and Sciences by Arthur Zucker Associate Professor of Philosophy Benjamin M. Ogles Dean, College of Arts and Sciences 3 ABSTRACT ENCK, GAVIN G., M.A., June 2009, Philosophy A Comparison of Two Bioethical Theories (81 pp.) Director of Thesis: Arthur Zucker This thesis compares two bioethical theories in order to determine which theory is better for use by medical professionals. The two theories are Tom L. Beauchamp and James Childress’s “Principlism” and Bernard Gert, K. Danner Clouser, and Charles M. Culver’s “Moral Rules.” The structure of the paper is as follows: an explication of both theories, an examination of the similarities and differences between the theories, an evaluation of criticisms of both theories, and identification of the three advantages the Moral Rules theory has over Principlism. In the conclusion, I claim the Moral Rules is the better bioethical theory for the medical profession. Approved: _____________________________________________________________ Arthur Zucker Associate Professor of Philosophy 4 TABLE OF CONTENTS Page Abstract .............................................................................................................................. -

Bioethics and Informed Consent
Bioethics and Informed Consent Professor Lucy Allais Informed consent is a central notion in bioethics. The emphasis on informed consent in medical practice is relatively recent (20th century). Bioethics is a relatively young field, beginning, in the USA, in the 50s and 60s, maturing in the 80s and 90s. This is different to both medical ethics, and ethics generally. Medical ethics Reflections by doctors and societies on the ethics of medical practice is probably as old as doctoring (Hippocratic oath; the Code of Hammurabi, written in Babylon in 1750 BC). Traditionally focused on the doctor-patient relationship and the virtues possessed by the good doctor. (Kuhse and Singer A Companion to Bioethics 2001:4). Ethics in philosophy: Morality: how should we live? what is right? what is wrong? Ethics: the academic study of morality. Are there objective values? Are there truths about right and wrong? What makes actions wrong? How do we resolve moral disputes? What is the basis of human rights? When (if ever) is euthanasia permissible? Is it morally justifiable to incarcerate MDR TB patients? “in 1972, no American medical school thought medical ethics important enough to be taught to all future physicians.... A decade later, in 1984—after the advent of bioethics—84 percent of medical schools required students to take a course in medical ethics or bioethics during their first two years of instruction.” (Baker 2013) The four core values of autonomy, justice, beneficence and non-maleficence. Autonomy often dominates discussions of bioethics. 6 Informed consent is linked to autonomy. Autonomy means being self-governing. Autonomy is often thought to be at the basis of human rights: human rights protect the capacities of each individual to live their life for themself. -

Protecting Human Research Participants NIH Office of Extramural Research Introduction
Protecting Human Research Participants NIH Office of Extramural Research Introduction Research with human subjects can occasionally result in a dilemma for investigators. When the goals of the research are designed to make major contributions to a field, such as improving the understanding of a disease process or determining the efficacy of an intervention, investigators may perceive the outcomes of their studies to be more important than providing protections for individual participants in the research. Although it is understandable to focus on goals, our society values the rights and welfare of individuals. It is not considered ethical behavior to use individuals solely as means to an end. The importance of demonstrating respect for research participants is reflected in the principles used to define ethical research and the regulations, policies, and guidance that describe the implementation of those principles. Who? This course is intended for use by individuals involved in the design and/or conduct of National Institutes of Health (NIH) funded human subjects research. What? This course is designed to prepare investigators involved in the design and/or conduct of research involving human subjects to understand their obligations to protect the rights and welfare of subjects in research. The course material presents basic concepts, principles, and issues related to the protection of research participants. Why? As a part of NIH's commitment to the protection of human subjects and its response to Federal mandates for increased emphasis on protection for human subjects in research, the NIH Office of Extramural Research released a policy on Required Education in the Protection of Human Research Participants in June 2000.