Acid-Base Disorders and Renal Tubular Acidosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diabetic Ketoacidosis and Hyperosmolar BMJ: First Published As 10.1136/Bmj.L1114 on 29 May 2019
STATE OF THE ART REVIEW Diabetic ketoacidosis and hyperosmolar BMJ: first published as 10.1136/bmj.l1114 on 29 May 2019. Downloaded from hyperglycemic syndrome: review of acute decompensated diabetes in adult patients Esra Karslioglu French,1 Amy C Donihi,2 Mary T Korytkowski1 1Division of Endocrinology and Metabolism, Department of ABSTRACT Medicine, University of Pittsburgh, Pittsburgh, PA, USA Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome (HHS) are life threatening 2University of Pittsburgh School of complications that occur in patients with diabetes. In addition to timely identification of the Pharmacy, Pittsburgh, PA, USA Correspondence to: M Korytkowski precipitating cause, the first step in acute management of these disorders includes aggressive [email protected] administration of intravenous fluids with appropriate replacement of electrolytes (primarily Cite this as: BMJ 2019;365:l1114 doi: 10.1136/bmj.l1114 potassium). In patients with diabetic ketoacidosis, this is always followed by administration Series explanation: State of the of insulin, usually via an intravenous insulin infusion that is continued until resolution of Art Reviews are commissioned on the basis of their relevance to ketonemia, but potentially via the subcutaneous route in mild cases. Careful monitoring academics and specialists in the US and internationally. For this reason by experienced physicians is needed during treatment for diabetic ketoacidosis and HHS. they are written predominantly by Common pitfalls in management include premature termination of intravenous insulin US authors therapy and insufficient timing or dosing of subcutaneous insulin before discontinuation of intravenous insulin. This review covers recommendations for acute management of diabetic ketoacidosis and HHS, the complications associated with these disorders, and methods for http://www.bmj.com/ preventing recurrence. -

Acid-Base Abnormalities in Dogs with Diabetic Ketoacidosis: a Prospective Study of 60 Cases
325 Acid-base abnormalities in dogs with diabetic ketoacidosis: a prospective study of 60 cases Distúrbios ácido-base em cães com cetoacidose diabética: estudo prospectivo de 60 casos Ricardo DUARTE1; Denise Maria Nunes SIMÕES1; Khadine Kazue KANAYAMA1; Márcia Mery KOGIKA1 1School of Veterinary Medicine and Animal Science, University of São Paulo, São Paulo-SP, Brazil Abstract Diabetic ketoacidosis (DKA) is considered a typical high anion gap metabolic acidosis due to the retention of ketoanions. The objective of this study was to describe the acid-base disturbances of dogs with DKA and further characterize them, according to their frequency, adequacy of the secondary physiologic response, and occurrence of mixed disturbances. Sixty dogs with DKA were enrolled in the study. Arterial blood pH and gas tensions, plasma electrolytes, serum b-hydroxybutyrate (b-OHB), glucose, albumin and urea concentrations were determined for all dogs included in the study. All dogs were evaluated individually and systematically by the traditional approach to the diagnosis of acid- base disorders. Most of the dogs had a high anion gap acidosis, with appropriated respiratory response (n = 18; 30%) or concurrent respiratory alkalosis (n = 14; 23%). Hyperchloremic acidosis with moderated to marked increases in b-OHB was observed in 18 dogs (30%) and 7 of these patients had concurrent respiratory alkalosis. Hyperchloremic acidosis with mild increase in b-OHB was observed in 6 dogs (10%). Four dogs (7%) had a high anion gap acidosis with mild increase in b-OHB and respiratory alkalosis. Most of dogs with DKA had a high anion gap acidosis, but mixed acid-base disorders were common, chiefly high anion gap acidosis and concurrent respiratory alkalosis, and hyperchloremic acidosis with moderated to marked increases in serum b-OHB. -

Pathophysiology of Acid Base Balance: the Theory Practice Relationship
Intensive and Critical Care Nursing (2008) 24, 28—40 ORIGINAL ARTICLE Pathophysiology of acid base balance: The theory practice relationship Sharon L. Edwards ∗ Buckinghamshire Chilterns University College, Chalfont Campus, Newland Park, Gorelands Lane, Chalfont St. Giles, Buckinghamshire HP8 4AD, United Kingdom Accepted 13 May 2007 KEYWORDS Summary There are many disorders/diseases that lead to changes in acid base Acid base balance; balance. These conditions are not rare or uncommon in clinical practice, but every- Arterial blood gases; day occurrences on the ward or in critical care. Conditions such as asthma, chronic Acidosis; obstructive pulmonary disease (bronchitis or emphasaemia), diabetic ketoacidosis, Alkalosis renal disease or failure, any type of shock (sepsis, anaphylaxsis, neurogenic, cardio- genic, hypovolaemia), stress or anxiety which can lead to hyperventilation, and some drugs (sedatives, opoids) leading to reduced ventilation. In addition, some symptoms of disease can cause vomiting and diarrhoea, which effects acid base balance. It is imperative that critical care nurses are aware of changes that occur in relation to altered physiology, leading to an understanding of the changes in patients’ condition that are observed, and why the administration of some immediate therapies such as oxygen is imperative. © 2007 Elsevier Ltd. All rights reserved. Introduction the essential concepts of acid base physiology is necessary so that quick and correct diagnosis can The implications for practice with regards to be determined and appropriate treatment imple- acid base physiology are separated into respi- mented. ratory acidosis and alkalosis, metabolic acidosis The homeostatic imbalances of acid base are and alkalosis, observed in patients with differing examined as the body attempts to maintain pH bal- aetiologies. -

Surgeons, Columbia University, New York City) (Received for Publication August 9, 1932)
THE ADDIS SEDIMENT COUNT IN NORMAL CHILDREN By JOHN D. LYTTLE (From the Babies Hospit and the Department of Pediatrics, Colege of Physicians and Surgeons, Columbia University, New York City) (Received for publication August 9, 1932) THE METHOD In 1925 Addis (1) described a method by which, in a concentrated acid urine, the rate of excretion of protein, casts and red and white cells could be determined. His method, with certain modifications, has been followed here. All of the counts were made on the 12 hour night specimen from 7 or 8 P.M. to 7 or 8 A.M. Addis recommended that fluids be restricted during, and for 12 hours preceding the collection, since in dilute and alkaline urine hyaline casts dissolve and red cells may be completely lysed. With children this rigid restriction of fluid proved impossible. Withholding fluid during the afternoon and night except for 200 cc. at the evening meal, gave urines of such concentration and acidity that they were suitable for a count. Most children had an early supper and col- lections were started at 7 or 8 P.M. Under these conditions, the urinary pH was between 5.0 and 6.0 and the specific gravity usually well above 1.020. The specimens were treated as described by Addis: "the con- centrated night urine is thoroughly mixed by repeated inversion of the rubber-stoppered bottle and a 10 cc. sample is transferred to a special graduated tube, and centrifugalized for five minutes at 1,800 revolutions per minute. The supernatant urine is decanted and pipetted down to a known volume which varies with the amount of sediment as judged by direct observation. -

Arterial Blood Gases: Acid-Base Balance
EDUCATIONAL COMMENTARY – ARTERIAL BLOOD GASES: ACID-BASE BALANCE Educational commentary is provided through our affiliation with the American Society for Clinical Pathology (ASCP). To obtain FREE CME/CMLE credits click on Earn CE Credits under Continuing Education on the left side of the screen. **Florida licensees, please note: This exercise will appear in CE Broker under the specialty of Blood Gas Analysis. LEARNING OUTCOMES On completion of this exercise, the participant should be able to • identify the important buffering systems in the human body. • explain the Henderson-Hasselbalch equation and its relationship to the bicarbonate/carbonic acid buffer system. • explain the different acid-base disorders, causes associated with them, and compensatory measures. • evaluate acid-base status using patient pH and pCO2 and bicarbonate levels. Introduction Arterial blood gas values are an important tool for assessing oxygenation and ventilation, evaluating acid- base status, and monitoring the effectiveness of therapy. The human body produces a daily net excess of acid through normal metabolic processes: cellular metabolism produces carbonic, sulfuric, and phosphoric acids. Under normal conditions, the body buffers accumulated hydrogen ions (H+) through a variety of buffering systems, the respiratory center, and kidneys to maintain a plasma pH of between 7.35 and 7.45. This tight maintenance of blood pH is essential: even slight changes in pH can alter the functioning of enzymes, the cellular uptake and use of metabolites, and the uptake and release of oxygen. Although diagnoses are made by physicians, laboratory professionals must be able to interpret arterial blood gas values to judge the validity of the laboratory results they report. -

Persistent Lactic Acidosis - Think Beyond Sepsis Emily Pallister1* and Thogulava Kannan2
ISSN: 2377-4630 Pallister and Kannan. Int J Anesthetic Anesthesiol 2019, 6:094 DOI: 10.23937/2377-4630/1410094 Volume 6 | Issue 3 International Journal of Open Access Anesthetics and Anesthesiology CASE REPORT Persistent Lactic Acidosis - Think beyond Sepsis Emily Pallister1* and Thogulava Kannan2 1 Check for ST5 Anaesthetics, University Hospitals of Coventry and Warwickshire, UK updates 2Consultant Anaesthetist, George Eliot Hospital, Nuneaton, UK *Corresponding author: Emily Pallister, ST5 Anaesthetics, University Hospitals of Coventry and Warwickshire, Coventry, UK Introduction • Differential diagnoses for hyperlactatemia beyond sepsis. A 79-year-old patient with type 2 diabetes mellitus was admitted to the Intensive Care Unit for manage- • Remember to check ketones in patients taking ment of Acute Kidney Injury refractory to fluid resusci- Metformin who present with renal impairment. tation. She had felt unwell for three days with poor oral • Recovery can be protracted despite haemofiltration. intake. Admission bloods showed severe lactic acidosis and Acute Kidney Injury (AKI). • Suspect digoxin toxicity in patients on warfarin with acute kidney injury, who develop cardiac manifes- The patient was initially managed with fluid resus- tations. citation in A&E, but there was no improvement in her acid/base balance or AKI. The Intensive Care team were Case Description asked to review the patient and she was subsequently The patient presented to the Emergency Depart- admitted to ICU for planned haemofiltration. ment with a 3 day history of feeling unwell with poor This case presented multiple complex concurrent oral intake. On examination, her heart rate was 48 with issues. Despite haemofiltration, acidosis persisted for blood pressure 139/32. -

Evaluation and Treatment of Alkalosis in Children
Review Article 51 Evaluation and Treatment of Alkalosis in Children Matjaž Kopač1 1 Division of Pediatrics, Department of Nephrology, University Address for correspondence Matjaž Kopač, MD, DSc, Division of Medical Centre Ljubljana, Ljubljana, Slovenia Pediatrics, Department of Nephrology, University Medical Centre Ljubljana, Bohoričeva 20, 1000 Ljubljana, Slovenia J Pediatr Intensive Care 2019;8:51–56. (e-mail: [email protected]). Abstract Alkalosisisadisorderofacid–base balance defined by elevated pH of the arterial blood. Metabolic alkalosis is characterized by primary elevation of the serum bicarbonate. Due to several mechanisms, it is often associated with hypochloremia and hypokalemia and can only persist in the presence of factors causing and maintaining alkalosis. Keywords Respiratory alkalosis is a consequence of dysfunction of respiratory system’s control ► alkalosis center. There are no pathognomonic symptoms. History is important in the evaluation ► children of alkalosis and usually reveals the cause. It is important to evaluate volemia during ► chloride physical examination. Treatment must be causal and prognosis depends on a cause. Introduction hydrogen ion concentration and an alkalosis is a pathologic Alkalosis is a disorder of acid–base balance defined by process that causes a decrease in the hydrogen ion concentra- elevated pH of the arterial blood. According to the origin, it tion. Therefore, acidemia and alkalemia indicate the pH can be metabolic or respiratory. Metabolic alkalosis is char- abnormality while acidosis and alkalosis indicate the patho- acterized by primary elevation of the serum bicarbonate that logic process that is taking place.3 can result from several mechanisms. It is the most common Regulation of hydrogen ion balance is basically similar to form of acid–base balance disorders. -

Inherited Renal Tubulopathies—Challenges and Controversies
G C A T T A C G G C A T genes Review Inherited Renal Tubulopathies—Challenges and Controversies Daniela Iancu 1,* and Emma Ashton 2 1 UCL-Centre for Nephrology, Royal Free Campus, University College London, Rowland Hill Street, London NW3 2PF, UK 2 Rare & Inherited Disease Laboratory, London North Genomic Laboratory Hub, Great Ormond Street Hospital for Children National Health Service Foundation Trust, Levels 4-6 Barclay House 37, Queen Square, London WC1N 3BH, UK; [email protected] * Correspondence: [email protected]; Tel.: +44-2381204172; Fax: +44-020-74726476 Received: 11 February 2020; Accepted: 29 February 2020; Published: 5 March 2020 Abstract: Electrolyte homeostasis is maintained by the kidney through a complex transport function mostly performed by specialized proteins distributed along the renal tubules. Pathogenic variants in the genes encoding these proteins impair this function and have consequences on the whole organism. Establishing a genetic diagnosis in patients with renal tubular dysfunction is a challenging task given the genetic and phenotypic heterogeneity, functional characteristics of the genes involved and the number of yet unknown causes. Part of these difficulties can be overcome by gathering large patient cohorts and applying high-throughput sequencing techniques combined with experimental work to prove functional impact. This approach has led to the identification of a number of genes but also generated controversies about proper interpretation of variants. In this article, we will highlight these challenges and controversies. Keywords: inherited tubulopathies; next generation sequencing; genetic heterogeneity; variant classification. 1. Introduction Mutations in genes that encode transporter proteins in the renal tubule alter kidney capacity to maintain homeostasis and cause diseases recognized under the generic name of inherited tubulopathies. -
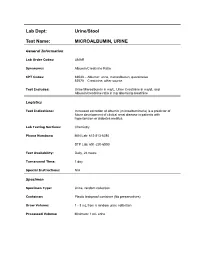
Lab Dept: Urine/Stool Test Name: MICROALBUMIN, URINE
Lab Dept: Urine/Stool Test Name: MICROALBUMIN, URINE General Information Lab Order Codes: UMAR Synonyms: Albumin/Creatinine Ratio CPT Codes: 82043 – Albumin: urine, microalbumin, quantitative 82570 – Creatinine; other source Test Includes: Urine Microalbumin in mg/L, Urine Creatinine in mg/dL and Albumin/creatinine ratio in mg albumin/g creatinine Logistics Test Indications: Increased excretion of albumin (microalbuminuria) is a predictor of future development of clinical renal disease in patients with hypertension or diabetes mellitus. Lab Testing Sections: Chemistry Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 1 day Special Instructions: N/A Specimen Specimen Type: Urine, random collection Container: Plastic leakproof container (No preservatives) Draw Volume: 1 - 3 mL from a random urine collection Processed Volume: Minimum: 1 mL urine Collection: A random urine sample may be obtained by voiding into a urine cup and is often performed at the laboratory. Bring the refrigerated container to the lab. Make sure all specimens submitted to the laboratory are properly labeled with the patient’s name, medical record number and date of birth. Special Processing: Lab Staff: Centrifuge specimen before analysis. Patient Preparation: Sample should not be collected after exertion, in the presence of a urinary tract infection, during acute illness, immediately after surgery, or after acute fluid load. Sample Rejection: Mislabled or unlabeled specimens; samples contaminated with blood Interpretive Reference Range: Albumin/creatinine ratio (A/C <30 mg/g Normal ratio) 30 - 299 mg/g Microalbuminuria >300 mg/g Clinical albuminuria Urine Creatinine: No reference ranges established Critical Values: N/A Limitations: Due to variability in urinary albumin excretion, at least two of three test results measured within a 6-month period should show elevated levels before a patient is designated as having microalbuminuria. -

./0) (Mm...)Conte H
BRITISH 511 Auc,.Auo. 25,25, 19621962 CARBON-MONOXIDE POISONIN6 MEDICAL JOURNAL Br Med J: first published as 10.1136/bmj.2.5303.511 on 25 August 1962. Downloaded from Case Reports HYPERVENTILATION IN Case 1.-A woman aged 61 was found with her head in CARBON-MONOXIDE POISONING a gas-oven. On admission to hospital she was deeply unconscious, with a generalized increase of muscle tone. BY pulse rate 140 a minute, and blood-pressure 110/70 mm. Hg. G. L. LEATHART, M.D., M.R.C.P. There was marked hyperventilation suggesting the possibility of coincident aspirin poisoning. A stomach wash-out, how- Nuflield Department of Industrial Health, the Medical ever, revealed no tablets, and a sample of urine collected School, King's College, Newcastle upon Tyne a few hours later contained no detectable salicylate. In 24 hours she had recovered fully and was transferred to a The recent revival of interest in the use of 5% or 7% mental hospital. carbogen in the treatment of carbon-monoxide poisoning Case 2.-An accountant aged 40 was working late in his has prompted the description of four unusual cases in office and was seen to be well at 9.15 p.m. At 8.45 a.m. which gross hyperventilation occurred. The investiga- the following morning he was found in the office with the tion of these cases was not very thorough, but such cases gas turned on but unlit. He was deeply unconscious with are seen so seldom that it is felt that even this incomplete strikingly deep and rapid respiration suggesting a condition report may be of value in stimulating further research. -

Oral Rehydration of Adult Cattle Using Isotonic Solution of Sugar, Sodium Chloride and Potassium Chloride
Haryana Vet. (Dec., 2019) 58(2), 166-169 Research Article ABSTRACT Fig 2: Transmission electron photomicrograph of monocyte of dog Present study comprised of 72 crossbred cows (group I= 60 endometritic and group II=12 healthy) at 30±2days postpartum. The showing heterochromatin (a), euchromatin (b), cytoplasmic process (c), polymorphonuclear neutrophils (PMN) cell coun Vacuole and nuclear membrane. Uranyl acetate and lead citrate × 25500 Figure 1: Cyclic conditions for PCR profiling for detection of Salmonella genes ASSOCIATION OF SEMEN TRAITS IN CONSECUTIVE EJACULATES WITH FSH-β GENE POLYMORPHISM IN HOLSTEIN-FRIESIAN CROSSBRED BULLS FROM INDIA VIJAY KADAM, ABH trus synchronizathod that synchronizes ovulations is Corresponding author: [email protected] Fig. 1. Histogram depicting frequency distribution of animal named briefly as “Ovsynch” (Pursley et al., 1995). The right score of respondents Clinical Article study was aimed to evaluate the efficacy of different methods of estrus sync Fig. 1. Semilogarithmic plot of plasma concentration time profile of amoxicillin and cloxacillin following single dose (10 mg/kg) i.v. and i.m. administration in sheep (n=4) Haryana Vet. (Dec., 2019) 58(2), 166-169 Research Article 2003) which might lead to increased chances of urolith the time for the urinary tract to restore patency (Parrah, Haryana Vet. (March, 2020) 59(SI), 93-95 Short Communication Research Article formation. The increased hospital incidence can also be 2009) in conjugation with supportive treatments like COMPARATIVE EFFICACY OF SYNCHRONIZATION PROTOCOLS FOR IMPROVING attributed to the proximity of the clinic as well. According to peritoneal lavage, urinary acidifiers and urinary ORAL REHYDRATION OF ADULT CATTLE USING ISOTONIC SOLUTION OF SUGAR, FERTILITY IN POSTPARTUM CROSSBRED DAIRY COWS data published by Department ff Soil Science, Haryana, antiseptics. -

Albuminuria Versus Egfr
Albuminuria versus GFR as markers of diabetic CKD progression KDIGO Controversies Conference: “Diabetic Kidney Disease” New Delhi, March 2012 Richard J MacIsaac PhD FRACP Director of Endocrinology & Diabetes, St Vincent's Hospital Professorial Fellow, University of Melbourne Evolution of Diabetic CKD Incipient Overt Nephropathy Nephropathy GFR 100 Log AER (ml/min) GFR 10 15 20 yrs Normoalbuminuria Microalbuminuria Macroalbuminuria (AER < 20 µµµg/min) (AER 20-200 µµµg/min) (AER > 200 µµµg/min) Stages of CKD Stage eGFR Description Predominant (ml/min/1.73 m2) AER status 1 > 90 Kidney damage with normal/high GFR Normo- Micro- 2 60-89 Kidney damage with mild reduction in GFR Micro- 3 30-59 Kidney damage with moderate reduction in Micro/Macro- GFR 4 15-29 Kidney damage with severe reduction in Macro- GFR 5 < 15 Kidney failure Albuminuria versus GFR as markers of diabetic CKD progression 1. Albuminuria as a predictor of diabetic CKD 2. GFR as a predictor of diabetic CKD 3. Albuminuria & GFR uncoupling/coupling 4. Summary Albuminuria as a marker of diabetic CKD progression • High Variability M N • Low Specificity • Spontaneous Regression µ • Δ AER ≠ Δ GFR Higher levels of urinary albumin excretion within the normal range predict faster decline in glomerular filtration rate in diabetic patients Babazono T et al. Diabetes Care 2009;32:1518-1520 Albuminuria versus GFR as markers of diabetic CKD progression 1. Albuminuria as a predictor of diabetic CKD 2. GFR as a predictor of diabetic CKD 3. ALbuminuria & GFR uncoupling/coupling 4. Summary GFR as