Histopathological Changes in the Chorionic Villi and Endometrial Decidual Tissues in the Product of Conception of Spontaneous Abortion Cases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
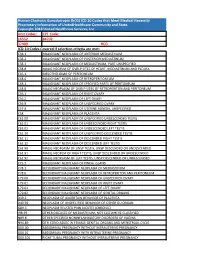
Human Chorionic Gonadotropin (Hcg) ICD 10 Codes That Meet Medical Necessity Proprietary Information of Unitedhealthcare Community and State
Human Chorionic Gonadotropin (hCG) ICD 10 Codes that Meet Medical Necessity Proprietary Information of UnitedHealthcare Community and State. Copyright 2018 United Healthcare Services, Inc Unit Codes: CPT Code: 16552 84702 37409 HCG ICD-10 Codes Covered if selection criteria are met: C38.1 MALIGNANT NEOPLASM OF ANTERIOR MEDIASTINUM C38.2 MALIGNANT NEOPLASM OF POSTERIOR MEDIASTINUM C38.3 MALIGNANT NEOPLASM OF MEDIASTINUM, PART UNSPECIFIED C38.8 MALIG NEOPLM OF OVRLP SITES OF HEART, MEDIASTINUM AND PLEURA C45.1 MESOTHELIOMA OF PERITONEUM C48.0 MALIGNANT NEOPLASM OF RETROPERITONEUM C48.1 MALIGNANT NEOPLASM OF SPECIFIED PARTS OF PERITONEUM C48.8 MALIG NEOPLASM OF OVRLP SITES OF RETROPERITON AND PERITONEUM C56.1 MALIGNANT NEOPLASM OF RIGHT OVARY C56.2 MALIGNANT NEOPLASM OF LEFT OVARY C56.9 MALIGNANT NEOPLASM OF UNSPECIFIED OVARY C57.4 MALIGNANT NEOPLASM OF UTERINE ADNEXA, UNSPECIFIED C58 MALIGNANT NEOPLASM OF PLACENTA C62.00 MALIGNANT NEOPLASM OF UNSPECIFIED UNDESCENDED TESTIS C62.01 MALIGNANT NEOPLASM OF UNDESCENDED RIGHT TESTIS C62.02 MALIGNANT NEOPLASM OF UNDESCENDED LEFT TESTIS C62.10 MALIGNANT NEOPLASM OF UNSPECIFIED DESCENDED TESTIS C62.11 MALIGNANT NEOPLASM OF DESCENDED RIGHT TESTIS C62.12 MALIGNANT NEOPLASM OF DESCENDED LEFT TESTIS C62.90 MALIG NEOPLASM OF UNSP TESTIS, UNSP DESCENDED OR UNDESCENDED C62.91 MALIG NEOPLM OF RIGHT TESTIS, UNSP DESCENDED OR UNDESCENDED C62.92 MALIG NEOPLASM OF LEFT TESTIS, UNSP DESCENDED OR UNDESCENDED C75.3 MALIGNANT NEOPLASM OF PINEAL GLAND C78.1 SECONDARY MALIGNANT NEOPLASM OF MEDIASTINUM C78.6 SECONDARY -

Histomorphological Study of Chorionic Villi in Products of Conception Following First Trimester Abortions
November, 2018/ Vol 4/ Issue 7 Print ISSN: 2456-9887, Online ISSN: 2456-1487 Original Research Article Histomorphological study of chorionic villi in products of conception following first trimester abortions Shilpa MD1, Supreetha MS2, Varshashree3 1Dr. Shilpa, MD, Assistant Professor, 2Dr. Supreetha, MS, Assistant Professor, 3Dr. Varshashree, Post graduate, all authors are affiliated with Department of Pathology, Sri Devaraj Urs Medical College, Tamaka, Kolar, Karnataka, India. Corresponding Author: Dr. Shilpa, MD, Assistant Professor, Department of Pathology, Sri Devaraj Urs Medical College, Tamaka, Kolar, Karnataka, India. Email id: [email protected] ………………………………………………………………………………………………………………………………... Abstract Background: The common problem which occurs in first trimester of pregnancy is miscarriage. Retained products of conception are commonly received specimen for histopathological examination. Apart from confirmation of pregnancy, a careful examination can provide some additional information about the cause or the conditions associated with abortion. Aim: 1. To study various histopathological changes occurring in chorionic villi in first trimester spontaneous abortions and to know the pathogenesis of abortions. Materials and methods: This was a cross sectional retrospective study carried out for over a period of 3 years from January 2015 to January 2018. A total of 235biopsies were obtained from patient with the diagnosis of the first trimester spontaneous abortions were included in this study. Results: In our study most common age group of the abortion was between 21-30 years (63%). Incomplete abortion was the commonest type of abortion (47.7%). Many dysmorphic features were observed in this study like hydropic change (67%), stromal fibrosis (62%), villi with reduced blood vessels (52.7%) and perivillous fibrin deposition. -

Medical Abortion Reference Guide INDUCED ABORTION and POSTABORTION CARE at OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) © 2017, 2018 Ipas
Medical Abortion Reference Guide INDUCED ABORTION AND POSTABORTION CARE AT OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) © 2017, 2018 Ipas ISBN: 1-933095-97-0 Citation: Edelman, A. & Mark, A. (2018). Medical Abortion Reference Guide: Induced abortion and postabortion care at or after 13 weeks gestation (‘second trimester’). Chapel Hill, NC: Ipas. Ipas works globally so that women and girls have improved sexual and reproductive health and rights through enhanced access to and use of safe abortion and contraceptive care. We believe in a world where every woman and girl has the right and ability to determine her own sexuality and reproductive health. Ipas is a registered 501(c)(3) nonprofit organization. All contributions to Ipas are tax deductible to the full extent allowed by law. For more information or to donate to Ipas: Ipas P.O. Box 9990 Chapel Hill, NC 27515 USA 1-919-967-7052 [email protected] www.ipas.org Cover photo: © Ipas The photographs used in this publication are for illustrative purposes only; they do not imply any particular attitudes, behaviors, or actions on the part of any person who appears in the photographs. Printed on recycled paper. Medical Abortion Reference Guide INDUCED ABORTION AND POSTABORTION CARE AT OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) Alison Edelman Senior Clinical Consultant, Ipas Professor, OB/GYN Oregon Health & Science University Alice Mark Associate Medical Director National Abortion Federation About Ipas Ipas works globally so that women and girls have improved sexual and reproductive health and rights through enhanced access to and use of safe abortion and contraceptive care. -

Miscarriage Or Early Pregnancy Loss- Diagnosis and Management (Version 5)
Miscarriage or early pregnancy loss- diagnosis and management (Version 5) Guideline Readership This guideline applies to all women diagnosed with miscarriage in early pregnancy (up to 13 completed weeks) within the Heart of England Foundation Trust and to attending clinicians, sonographers and nursing staff on Gynaecology ward and early pregnancy unit. All care is tailored to individual patient needs, with an in-depth discussion of the intended risks and benefits for any intervention offered to woman with early pregnancy loss. Guideline Objectives The objective of this guideline is to enable all clinicians to recognise the different types of miscarriages and to follow a recognised management pathway so that all women with actual or suspected miscarriage receive, an appropriate and individualised care. Other Guidance Ectopic pregnancy and miscarriage: diagnosis and initial management. NICE guidance Dec 2012 Ratified Date: Insert Date Launch Date: 16 March 2018 Review Date: 16 March 2021 Guideline Author: Dr Rajmohan, Dr Cheema Contents & page numbers: 1. Flowcharts Flowchart 1 – Management of complete miscarriage p3 Flowchart 2 – Management of incomplete miscarriage p4 Flowchart 3 – Management of Missed miscarriage p5 Flowchart 4 - Management of Early fetal demise p6 Flowchart 5 – Medical management of miscarriage p7 Flowchart 6 - Surgical management (SMM) pathway p8 2. Executive summary and Overview p9 3. Body of guideline Types of miscarriage p9 Threatened miscarriage p9 Complete miscarriage p9 Incomplete miscarriage p9 Missed miscarriage -

Mammalogy Lecture 12
Mammalogy Lecture 11 - Reproduction I: General Patterns I. Obviously, reproduction is a very important aspect of biology and whole courses are dedicated to it. It’s easy to understand why reproductive traits would be subject to strong selection because of their direct effects on fitness. II. As we might expect, there are three basic types of mammalian reproduction. These correspond to the three major groups of mammals. Differences among these types reflect the degree of intimacy of fetal-maternal contact. A. Monotreme Type - Retain the primitive amniote pattern, but add a period of lactation. - Egg is very large at ovulation, about 3 mm. It moves down the oviduct where it is fertilized, then it’s coated with albumin, then a shell is laid down by a shell gland, and the shell is mineralized (with CaCO3). - Embryo spends 2-3 weeks in the uterus, then it’s laid. It’s large, 15 mm, when it’s laid. - Embryo growth is supported entirely by the yolk that’s enclosed in the egg. B. Metatherian type: - In some superficial ways it’s similar to monotremes, in that metatherians retain a shell membrane around the fertilized egg; a shell gland is present in Müllerian ducts. - However the shell is never mineralized and young are born live after only ca. 12 days, as we’ve seen, they are very altricial (poorly developed). - Initial intrauterine growth is supported by maternally by a placenta. - Metatherian placenta is the choriovitelline type - yolk-sac placenta (Eutherian placenta is called chorioallantoic placenta) C. Placenta Formation - Let’s look at formation of the placenta in Meta- & Eutherians. -

Ectopic Pregnancy Management: Tubal and Interstitial SIGNS / SYMPTOMS DIAGNOSIS
8/29/19njm Ectopic Pregnancy Management: Tubal and interstitial SIGNS / SYMPTOMS Pain and vaginal bleeding are the hallmark symptoms of ectopic pregnancy. Pain is almost universal; it is generally lower abdominal and unilateral. Bleeding is also very common following a short period of amenorrhea. Physical exam may reveal a tender adnexal mass, often mentioned in texts, but noted clinically only 20 percent of the time. Furthermore, it may easily be confused with a tender corpus luteum of a normal intrauterine pregnancy. Finally signs and symptoms of hemoperitoneum and shock can occur, including a distended, silent, “doughy” abdomen, shoulder pain, bulging cul de sac into the posterior fornix of the vagina, and hypotension. DIAGNOSIS Initially, serum hCG rises, but then usually plateaus or falls. Transvaginal ultrasound scanning is a key diagnostic tool and can rapidly make these diagnoses: 1. Ectopic is ruled out by the presence of an intrauterine pregnancy with the exception of rare heterotopic pregnancy 2. Ectopic is proven when a gestational sac and an embryo with a heartbeat is seen outside of the uterus 3. Ectopic is highly likely if ANY adnexal mass distinct from the corpus luteum or a significant amount of free pelvic fluid is seen. When ultrasound is not definitive, correlation of serum hCG levels is important. If the hCG is above the “discriminatory zone” of 3000 mIU/ml IRP, a gestational sac should be visible on transvaginal ultrasound. The discriminatory zone varies by ultrasound machine and sonographer. If an intrauterine gestational sac is not visible by the time the hCG is at, or above, this threshold, the pregnancy has a high likelihood of being ectopic. -

Equine Placenta – Marvelous Organ and a Lethal Weapon
Equine placenta – marvelous organ and a lethal weapon Malgorzata Pozor, DVM, PhD, Diplomate ACT Introduction Placenta has been defined as: „an apposition between parent (usually maternal) and fetal tissue in order to establish physiological exchange” (1). Another definition of this important organ was proposed by Steven and Morris: „a device consisting of one or more transport epithelia located between fetal and maternal blood supply” (2). The main function of placenta is to provide an interface between the dam and the the fetus and to allow the metabolic exchange of the the nutrients, oxygen and waste material. The maternal circulation is brought into a close apposition to the fetal circulation, while a separation of these two circulatory systems remain separated (3). A degree and complexity of this „intimate relationship” varies greately between species mostly due to the structural diversity of the extraembryonic membranes of the vertebrates. The early feto-maternal exchange in the equine pregnancy is established as early as on day 22 after fertilization. The fetal and choriovitellin circulations are already present, the capsule ruptures and the allantois is already visible (4). The allantois starts expanding by day 32 and vascularizes approximately 90% of the chorion and fuses with it to form chorioallantois by day 38 of gestation (5). The equine placenta continues increasing its complexity till approximately day 150 of gestation. Equids have epitheliochorial placenta, there are six leyers separating maternal and fetal circulation, and there are no erosion of the luminal, maternal epithelium, like in ruminants (6). Thousands of small chorionic microvilli develop and penetrate into endometrial invaginations. -

From Trophoblast to Human Placenta
From Trophoblast to Human Placenta (from The Encyclopedia of Reproduction) Harvey J. Kliman, M.D., Ph.D. Yale University School of Medicine I. Introduction II. Formation of the placenta III. Structure and function of the placenta IV. Complications of pregnancy related to trophoblasts and the placenta Glossary amnion the inner layer of the external membranes in direct contact with the amnionic fluid. chorion the outer layer of the external membranes composed of trophoblasts and extracellular matrix in direct contact with the uterus. chorionic plate the connective tissue that separates the amnionic fluid from the maternal blood on the fetal surface of the placenta. chorionic villous the final ramification of the fetal circulation within the placenta. cytotrophoblast a mononuclear cell which is the precursor cell of all other trophoblasts. decidua the transformed endometrium of pregnancy intervillous space the space in between the chorionic villi where the maternal blood circulates within the placenta invasive trophoblast the population of trophoblasts that leave the placenta, infiltrates the endo– and myometrium and penetrates the maternal spiral arteries, transforming them into low capacitance blood channels. Sunday, October 29, 2006 Page 1 of 19 From Trophoblasts to Human Placenta Harvey Kliman junctional trophoblast the specialized trophoblast that keep the placenta and external membranes attached to the uterus. spiral arteries the maternal arteries that travel through the myo– and endometrium which deliver blood to the placenta. syncytiotrophoblast the multinucleated trophoblast that forms the outer layer of the chorionic villi responsible for nutrient exchange and hormone production. I. Introduction The precursor cells of the human placenta—the trophoblasts—first appear four days after fertilization as the outer layer of cells of the blastocyst. -
Placenta-4-2-15.Pdf
3.2.2015 PLACENTA Dr. Archana Rani Associate Professor Department of Anatomy KGMU UP, Lucknow Implantation • Begins on the 6th day after fertilization • Embedding of blastocyst in the wall of uterus • Disappearance of zona pellucida • Cells of the trophoblast stick to the endometrium • After implantation of the embryo, the uterine endometrium is called the decidua Implantation Site of implantation • Normal site - At the junction of fundus and posterior wall of uterus - At upper uterine segment Interstitial Implantation The Decidua After implantation of the embryo, the uterine endometrium is called the decidua. Subdivisions of Decidua Formation of Chorionic Villi • Villi are the essential functional elements of the placenta. • Small finger like processes. • Surrounded by maternal blood. • Fetal blood circulates in their substance through capillaries. • Called as Chorionic villi as arises as offshoots from chorion. Stages in formation of Chorionic villi Early stages in formation of Chorionic villi (9th day) Formation of Chorionic villi Lacunar spaces filled with maternal blood Primary Villus (Day 13-14) All elements (syncytium, cytotrophoblast and extraembryonic mesoderm) take part in formation of chorionic villi. Three stages in formation of chorionic villi are seen: Primary villus: central core of cytotrophoblast covered by a layer of syncytiotrophoblast. Adjoining villi are separated by an intervillous space. Secondary Villus (Early 3rd week) Central core of extraembryonic mesoderm covered successively by cyto and syncytiotrophoblasts. Tertiary Villus (End of 3rd week) Appearance of blood vessels in the mesoderm forming core of each villus. Formation of cytotrophoblastic shell Anchoring villi & its subdivisions Fully formed Placenta (4th month) DEFINITION • Placenta is a fetomaternal organ which is the primary site of nutrient and gas exchange between the fetus and the mother. -
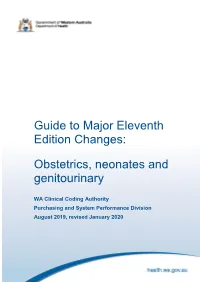
Guide to Major Eleventh Edition Changes: Obstetrics, Neonates And
Guide to Major Eleventh Edition Changes: Obstetrics, neonates and genitourinary WA Clinical Coding Authority Purchasing and System Performance Division August 2019, revised January 2020 1 Contents Chapter 15 Pregnancy, childbirth and the puerperium 3 ACS 1500 Diagnosis sequencing in obstetric episodes of care 3 ACS 1505 Delivery and assisted delivery codes 3 Delivery of baby prior to the admitted episode of care 5 ACS 1550 Discharge/transfer in labour 7 Transfer in first stage of labour 7 Transfer in third stage of labour 7 Failed induction of labour 9 Postpartum haemorrhage 9 ACS 1551 Obstetric perineal lacerations/grazes 11 ACS 1511 Termination of pregnancy (abortion) 11 ACS 1544 Complications following pregnancy with abortive outcome 14 Complications following abortion 14 Admission for retained products of conception following abortion 16 Hypoglycaemia in gestational diabetes mellitus 16 Mental Health and pregnancy 16 Neonates 16 Genitourinary 17 Acknowledgement 17 2 This guide was updated in January 2020 with creation of Examples 6, 7 and 19. Chapter 15 Pregnancy, childbirth and the puerperium Amendments include: Changes to code titles to specify ‘in pregnancy, childbirth and the puerperium.’ Changes to ACS titles for 1500 Diagnosis sequencing in obstetric episodes of care, 1511 Termination of pregnancy (abortion) and 1544 Complications following pregnancy with abortive outcome. Deletion of Excludes notes throughout ICD-10-AM to promote multiple condition coding. Clarification that codes from other chapters may be assigned to add specificity. Creation of four character codes to classify failed medical and surgical induction of labour. Indexing amendments to clarify code assignment for failed trial of labour and failure to progress unspecified, with or without identification of an underlying cause. -
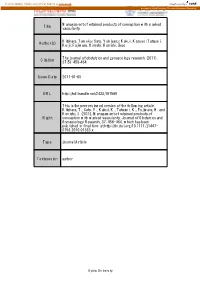
Title Management of Retained Products of Conception with Marked
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Kyoto University Research Information Repository Management of retained products of conception with marked Title vascularity. Kitahara, Tomoko; Sato, Yukiyasu; Kakui, Kazuyo; Tatsumi, Author(s) Keiji; Fujiwara, Hiroshi; Konishi, Ikuo The journal of obstetrics and gynaecology research (2011), Citation 37(5): 458-464 Issue Date 2011-01-05 URL http://hdl.handle.net/2433/197589 This is the peer reviewed version of the following article: Kitahara, T., Sato, Y., Kakui, K., Tatsumi, K., Fujiwara, H. and Konishi, I. (2011), Management of retained products of Right conception with marked vascularity. Journal of Obstetrics and Gynaecology Research, 37: 458‒464, which has been published in final form at http://dx.doi.org/10.1111/j.1447- 0756.2010.01363.x Type Journal Article Textversion author Kyoto University 1 Management of Retained Products of Conception with Marked Vascularity 2 3 Tomoko Kitahara, Yukiyasu Sato*, Kazuyo Kakui, Keiji Tatsumi, Hiroshi Fujiwara, and 4 Ikuo Konishi 5 6 Department of Gynecology and Obstetrics, Kyoto University Graduate School of 7 Medicine 8 9 *Address correspondence and reprint requests to: Yukiyasu Sato, M.D., Ph.D. 10 Department of Gynecology and Obstetrics, Kyoto University Graduate School of 11 Medicine, Sakyo-ku, Kyoto 606-8507, Japan. 12 Tel; 81-75-751-3269: Fax; 81-75-761-3967: E-mail; [email protected] 13 14 Short title; Management of Hypervascular RPOC 15 Keywords; color Doppler, uterine artery embolization, expectant management 16 1 1 Abstract 2 3 Cases of retained products of conception (RPOC) with marked vascularity present a 4 clinical challenge because simple dilation and curettage (D&C) can lead to 5 life-threatening hemorrhage. -

Placental Pathology: Its Impact on Explaining Prenatal and Perinatal Death
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2004 Placental pathology: its impact on explaining prenatal and perinatal death Stallmach, Thomas ; Hebisch, Gundula Abstract: This review considers six main situations in which pathologists are expected to report and interpret placental messages for obstetricians, neonatologists and, indirectly, parents: (1) abortion is the body’s corrective response to the embryonic defect suggested by malformed chorionic villi; (2) in- fection causing chorionic villous inflammation is specific and haematogenous; pathogen identification is mandatory, in contrast to chorioamnionitis caused by increased local immunosuppression allowing indis- criminate bacterial entry; (3) prematurity and (4) intrauterine growth restriction are often associated with pregnancy-specific disease (pre-eclampsia) or pre-existing maternal conditions (systemic lupus); parental studies may improve outcome in subsequent pregnancies; (5) intrauterine death near term is often due to placental dysmaturity featuring a severely reduced number of syncytiocapillary membranes; it accounts for the death in utero of 3 in 1000 pregnancies; detection helps to minimise recurrence in subsequent pregnancies; (6) twins are best confirmed as monozygous by the absence of chorionic tissue in thedivid- ing membranes; most monochorionic twins have vascular connections whose detailed analysis is requested only if there are inter-twin differences in growth and colour. From a formal point of view, many morebits of pathology than discussed in this review can be found in placentas and, with the advances in ultrasonog- raphy, might even be seen prior to birth. The extent of such a disturbance might ultimately affect fetal growth, which is amenable to prenatal detection offering the chances for an appropriate management.