United States Foreign Assistance Oral History Program
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Contemporary Folk Week, July 24-30, 2016
36 24-30 Contemporary Folk Week celebrates our 25th Anniversary with a world-class staff of returning artist/instructors including our first Master Music Maker, folk legend Tom Paxton and the timeless artistry of Janis Ian. We’re honored to also welcome back favorites from last year and previous years including Grammy-winners Kathy Mattea, Jon Vezner, and Don Henry, folk stalwarts Ellis Paul, Cliff Eberhardt and Amy Speace, vocal coaches Siobhan Quinn and Danny Ellis, and music theory guru Ray Chesna. We welcome an exciting new addition to this year’s staff in one of the leading lights in today’s contemporary folk scene, the wonderful Mary Gauthier. Drawing on tradition and innovation, our instructors bring a world of practical and imaginative experience to help you create and perform the music that makes your heart sing. Whether you’re trying out material at a local ‘open mike’, a performer with some experience, a working musician looking for some help in reaching your next goal, or someone who would simply like to feel more confident pulling that guitar out in front of others, we’re here to help, and our foundations are support, fun, and community. Our top-notch staff, knowledgeable in the various aspects of both the art and business of contemporary acoustic music, can help you achieve your goals. In addition, our limited enrollment and small campus encourage community-building at its best – frequent and informal interaction between students and staff, all doing our utmost to ensure that you go home energized and empowered to make the most of your music in hands-on and meaningful ways. -

I^Igtorical ^Siisociation
American i^igtorical ^siisociation SEVENTY-SECOND ANNUAL MEETING NEW YORK HEADQUARTERS: HOTEL STATLER DECEMBER 28, 29, 30 Bring this program with you Extra copies 25 cents Please be certain to visit the hook exhibits The Culture of Contemporary Canada Edited by JULIAN PARK, Professor of European History and International Relations at the University of Buffalo THESE 12 objective essays comprise a lively evaluation of the young culture of Canada. Closely and realistically examined are literature, art, music, the press, theater, education, science, philosophy, the social sci ences, literary scholarship, and French-Canadian culture. The authors, specialists in their fields, point out the efforts being made to improve and consolidate Canada's culture. 419 Pages. Illus. $5.75 The American Way By DEXTER PERKINS, John L. Senior Professor in American Civilization, Cornell University PAST and contemporary aspects of American political thinking are illuminated by these informal but informative essays. Professor Perkins examines the nature and contributions of four political groups—con servatives, liberals, radicals, and socialists, pointing out that the continu ance of healthy, active moderation in American politics depends on the presence of their ideas. 148 Pages. $2.75 A Short History of New Yorh State By DAVID M.ELLIS, James A. Frost, Harold C. Syrett, Harry J. Carman HERE in one readable volume is concise but complete coverage of New York's complicated history from 1609 to the present. In tracing the state's transformation from a predominantly agricultural land into a rich industrial empire, four distinguished historians have drawn a full pic ture of political, economic, social, and cultural developments, giving generous attention to the important period after 1865. -

The RAMPART JOURNAL of Individualist Thought Is Published Quarterly (Maj'ch, June, September and December) by Rampart College
The Wisdom of "Hindsight" by Read Bain I On the Importance of Revisionism for Our Time by Murray N. Rothbard 3 Revisionism: A Key to Peace by llarry Elmer Barnes 8 Rising Germanophohia: The Chief Oh~~tacle to Current World War II Revisionism by Michael F. Connors 75 Revisionism and the Cold War, 1946-1~)66: Some Comments on Its Origins and Consequences by James J. Martin 91 Departments: Onthe Other Hand by Robert Lf.~Fevre 114 V01. II, No. 1 SPRING., 1966 RAMPART JOURNAL of Individualist Thought Editor .. _. __ . .__ _ __ .. __ _. Ruth Dazey Director of Publications - ---.- .. J. Dohn Lewis Published by Pine Tree Press for RAMPART COLLEGE Box 158 Larkspur, Colorado 80118 President -----------------.------------------ William J. Froh Dean . .. .__ ._ Robert LeFevre Board of Academic Advisers Robert L. Cunningham, Ph.D. Bruno Leoni, Ph.D. University of San Francisco University of Pavia San Francisco, California Turin, Italy Arthur A. Ekirch, Ph.D~ James J. Martin, Ph.D. State University of New York Rampart College Graduate School Albany, New York Larkspur, Colorado Georg. Frostenson, Ph.D. Ludwig von Mises, Ph.D. Sollentuna, Sweden New York University New York, New York J. P. Hamilius, Jr., Ph.D. Toshio Murata, M.B.A. College of Esch-sur-Alzette Luxembourg Kanto Gakuin University Yokohama, Japan F. A. Harper, Ph.D. Wm. A. Paton, Ph.D. Institute for Humane Studies University of Michigan Stanford, California Ann Arbor, Michigan F. A. von Hayek, Ph.D. Sylvester Petro, Ll.M. University of Freiburg New York University Freiburg, Germany New York, New York W. -

Chapter 23: War and Revolution, 1914-1919
The Twentieth- Century Crisis 1914–1945 The eriod in Perspective The period between 1914 and 1945 was one of the most destructive in the history of humankind. As many as 60 million people died as a result of World Wars I and II, the global conflicts that began and ended this era. As World War I was followed by revolutions, the Great Depression, totalitarian regimes, and the horrors of World War II, it appeared to many that European civilization had become a nightmare. By 1945, the era of European domination over world affairs had been severely shaken. With the decline of Western power, a new era of world history was about to begin. Primary Sources Library See pages 998–999 for primary source readings to accompany Unit 5. ᮡ Gate, Dachau Memorial Use The World History Primary Source Document Library CD-ROM to find additional primary sources about The Twentieth-Century Crisis. ᮣ Former Russian pris- oners of war honor the American troops who freed them. 710 “Never in the field of human conflict was so much owed by so many to so few.” —Winston Churchill International ➊ ➋ Peacekeeping Until the 1900s, with the exception of the Seven Years’ War, never ➌ in history had there been a conflict that literally spanned the globe. The twentieth century witnessed two world wars and numerous regional conflicts. As the scope of war grew, so did international commitment to collective security, where a group of nations join together to promote peace and protect human life. 1914–1918 1919 1939–1945 World War I League of Nations World War II is fought created to prevent wars is fought ➊ Europe The League of Nations At the end of World War I, the victorious nations set up a “general associa- tion of nations” called the League of Nations, which would settle interna- tional disputes and avoid war. -

Woodrow Wilson Library
WILSON LIBRARY FINDING AID Last updated on November 17, 2010 Only includes monographs. Other materials are cataloged and located separately. I/1 Harley, John Eugene. Selected documents and material for the study of international law and relations, with introductory chapters, special emphasis given international organization and international peace. Los Angeles: Times-Mirror Press, 1923. Inscribed to Wilson by author. I/1. Haldane, Richard Burdon, 1st viscount. Higher nationality: a study in law and ethics. An address delivered before the American Bar Association and Montreal on 1st September, 1913. London: John Murray, 1913. I/1. Ewing, Elbert William Robinson. Legal and historical status of the Dred Scott decision… Washington, D.C.: Cobden Publishing Co., 1909. I/1. Holmes, Oliver Wendell. The common law. Boston: Little, Brown and Company, 1881. Signed by Wilson on title page inside cover above attached photo of author. I/1. Holland, Sir Thomas Erskine. The elements of jurisprudence. New York: Oxford University Press, 1900. I/1. Holst, Hermann Eduard von. The constitutional law of the United States of America. Translated by Alfred Bishop Mason. Chicago: Callaghan & Co., 1887. Signed by Wilson. I/1. Donisthorpe, Wordsworth. Law in a free state. London and New York: Macmillan and Co., 1895. Signed by Wilson on title page. I/1. Greenidge, Abel Hendy Jones. A handbook of Greek constitutional history. Colored map of cosmopolitan Greece, ca. 430 B.C. London: Macmillan and Co., Ltd., 1896. Signed by Wilson on inside cover and title page. I/1. Brunner, Heinrich. The sources of the law in England. An historical introduction to the study of English law. -

AHA Colloquium
Cover.indd 1 13/10/20 12:51 AM Thank you to our generous sponsors: Platinum Gold Bronze Cover2.indd 1 19/10/20 9:42 PM 2021 Annual Meeting Program Program Editorial Staff Debbie Ann Doyle, Editor and Meetings Manager With assistance from Victor Medina Del Toro, Liz Townsend, and Laura Ansley Program Book 2021_FM.indd 1 26/10/20 8:59 PM 400 A Street SE Washington, DC 20003-3889 202-544-2422 E-mail: [email protected] Web: www.historians.org Perspectives: historians.org/perspectives Facebook: facebook.com/AHAhistorians Twitter: @AHAHistorians 2020 Elected Officers President: Mary Lindemann, University of Miami Past President: John R. McNeill, Georgetown University President-elect: Jacqueline Jones, University of Texas at Austin Vice President, Professional Division: Rita Chin, University of Michigan (2023) Vice President, Research Division: Sophia Rosenfeld, University of Pennsylvania (2021) Vice President, Teaching Division: Laura McEnaney, Whittier College (2022) 2020 Elected Councilors Research Division: Melissa Bokovoy, University of New Mexico (2021) Christopher R. Boyer, Northern Arizona University (2022) Sara Georgini, Massachusetts Historical Society (2023) Teaching Division: Craig Perrier, Fairfax County Public Schools Mary Lindemann (2021) Professor of History Alexandra Hui, Mississippi State University (2022) University of Miami Shannon Bontrager, Georgia Highlands College (2023) President of the American Historical Association Professional Division: Mary Elliott, Smithsonian’s National Museum of African American History and Culture (2021) Nerina Rustomji, St. John’s University (2022) Reginald K. Ellis, Florida A&M University (2023) At Large: Sarah Mellors, Missouri State University (2021) 2020 Appointed Officers Executive Director: James Grossman AHR Editor: Alex Lichtenstein, Indiana University, Bloomington Treasurer: William F. -
1 Column Unindented
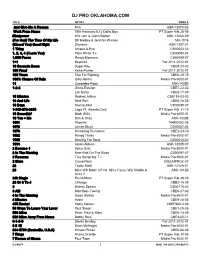
DJ PRO OKLAHOMA.COM TITLE ARTIST SONG # Just Give Me A Reason Pink ASK-1307A-08 Work From Home Fifth Harmony ft.Ty Dolla $ign PT Super Hits 28-06 #thatpower Will.i.am & Justin Bieber ASK-1306A-09 (I've Had) The Time Of My Life Bill Medley & Jennifer Warnes MH-1016 (Kissed You) Good Night Gloriana ASK-1207-01 1 Thing Amerie & Eve CB30053-02 1, 2, 3, 4 (I Love You) Plain White T's CB30094-04 1,000 Faces Randy Montana CB60459-07 1+1 Beyonce Fall 2011-2012-01 10 Seconds Down Sugar Ray CBE9-23-02 100 Proof Kellie Pickler Fall 2011-2012-01 100 Years Five For Fighting CBE6-29-15 100% Chance Of Rain Gary Morris Media Pro 6000-01 11 Cassadee Pope ASK-1403B 1-2-3 Gloria Estefan CBE7-23-03 Len Barry CBE9-11-09 15 Minutes Rodney Atkins CB5134-03-03 18 And Life Skid Row CBE6-26-05 18 Days Saving Abel CB30088-07 1-800-273-8255 Logic Ft. Alessia Cara PT Super Hits 31-10 19 Somethin' Mark Wills Media Pro 6000-01 19 You + Me Dan & Shay ASK-1402B 1901 Phoenix PHM1002-05 1973 James Blunt CB30067-04 1979 Smashing Pumpkins CBE3-24-10 1982 Randy Travis Media Pro 6000-01 1985 Bowling For Soup CB30048-02 1994 Jason Aldean ASK-1303B-07 2 Become 1 Spice Girls Media Pro 6000-01 2 In The Morning New Kids On The Block CB30097-07 2 Reasons Trey Songz ftg. T.I. Media Pro 6000-01 2 Stars Camp Rock DISCMPRCK-07 22 Taylor Swift ASK-1212A-01 23 Mike Will Made It Feat. -

Star Karaoke Song Book
All Star Karaoke Songs by Artist Karaoke Shack Song Books Title DiscID Title DiscID 12 Stones Adam Lambert Crash ASK-003675 Whataya Want From Me ASK109-1-01 Crash ASKCUS2-19 Adele 2AM Club Chasing Pavements ASK831-01 Not Your Boyfriend ASK1305A-08 Hometown Glory ASK1203-05 3 Doors Down I Will Be Waiting ASK1208-04 Be Like That ASK011-1-07 If It Hadn't Been For Love ACSK02-01 Be Like That ASK045-1-01 If It Hadn't Been For Love ASK-085807 Kryptonite ASK011-2-04 If It Hadn't Been For Love ASK831-02 Let Me Go ASK065-1-01 Lovesong ASK831-03 Let Me Go ASK1553-01 Make You Feel My Love ASK831-04 Let Me Go ASK6018-2-08 Rolling In The Deep ACSK02-02 Let Me Go (Rock Version) ASK1539-01 Rolling In The Deep ASK-085808 Loser ASK011-2-06 Rolling In The Deep ASK1563-01 38 Special Rolling In The Deep ASK831-05 Back Where You Belong ASK108-1-01 Rumour Has It ASK110-1-01 Hold On Loosely ASK069-1-01 Rumour Has It ASK1566-01 4Him Rumour Has It ASK831-06 Where There Is Faith ASK068-1-01 Set Fire To The Rain ASK1203-08 Where There Is Faith ASK6020-4-13 Someone Like You ASK1566-02 50 Cent Someone Like You ASK831-07 Disco Inferno ASK041-1-01 Turning Tables ASK110-1-02 Disco Inferno ASK056-1-01 Turning Tables ASK831-08 Disco Inferno ASK058-1-01 Adele (Wvocal) Disco Inferno ASK12008-1-1- Chasing Pavements ASK831-09 01 If It Hadn't Been For Love ASK831-10 Disco Inferno ASK12PK-01- Lovesong ASK831-11 01 Make You Feel My Love ASK831-12 Disco Inferno ASK1537-01 Rolling In The Deep ASK831-13 Disco Inferno ASK6013-1-01 Rumour Has It ASK831-14 Disco Inferno ASK6015-1-01 -

America and the Musical Unconscious E Music a L Unconl S Cious
G Other titles from Atropos Press Music occupies a peculiar role in the field of American Studies. It is undoubtedly (EDS.) “It is not as simple as saying that music REVE/P JULIUS GREVE & SASCHA PÖHLMANN Resonance: Philosophy for Sonic Art recognized as an important form of cultural production, yet the field continues does this or that; exploring the musical On Becoming-Music: to privilege textual and visual forms of art as its objects of examination. The es- unconscious means acknowledging the Between Boredom and Ecstasy says collected in this volume seek to adjust this imbalance by placing music cen- very fact that music always does more.” ter stage while still acknowledging its connections to the fields of literary and Philosophy of Media Sounds ÖHLMANN Hospitality in the Age of visual studies that engage with the specifically American cultural landscape. In Media Representation doing so, they proffer the concept of the ‘musical unconscious’ as an analytical tool of understanding the complexities of the musical production of meanings in various social, political, and technological contexts, in reference to country, www.atropospress.com queer punk, jazz, pop, black metal, film music, blues, carnival music, Muzak, hip-hop, experimental electronic music, protest and campaign songs, minimal ( E music, and of course the kazoo. DS. ) Contributions by Hanjo Berressem, Christian Broecking, Martin Butler, Christof Decker, Mario Dunkel, Benedikt Feiten, Paola Ferrero, Jürgen AMERIC Grandt, Julius Greve, Christian Hänggi, Jan Niklas Jansen, Thoren Opitz, Sascha Pöhlmann, Arthur Sabatini, Christian Schmidt, Björn Sonnenberg- Schrank, Gunter Süß, and Katharina Wiedlack. A A ND TH AMERICA AND THE MUSICAL UNCONSCIOUS E MUSIC A L UNCON S CIOUS ATROPOS PRESS new york • dresden 5 6 4 7 3 8 2 9 1 10 0 11 AMERICA AND THE MUSICAL UNCONSCIOUS JULIUS GREVE & SASCHA PÖHLMANN (EDS.) America and the Musical Unconscious Copyright © 2015 by Julius Greve and Sascha Pöhlmann (Eds.) The rights of the contributions remain with the respective authors. -

TABLE of CONTENTS Year, Song of the Year, Breakthrough Artist of the Year, Breakthrough Songwriter, and Breakthrough Artist- Category 1: Producer of the Year
PRESENTED BY: 32ND ANNUAL MusicRow Subscribed Members will vote to determine award winners. Ballots will be emailed on July 8, 2020. Ballot Voting Period: July 8, 2020 at 11:00 a.m. CST – July 17, 2020 at 5:00 p.m. CST. Winners Announced: August 18, 2020 To become a member, click here. Pictured: Alecia Davis, Kathie Lee Gifford, Sherod Robertson on stage at the 2019 MusicRow Awards. Photo: Steve Lowry By Sarah Skates MusicRow Magazine is proud to reveal the nominees for outside nominations being considered for Breakthrough the 2020 MusicRow Awards. This year’s honors will be Songwriter and Breakthrough Artist-Writer. Male and announced virtually among multiple MusicRow platforms Female Songwriter nominees are based on data from on Tuesday, August 18, 2020. MusicRow’s Top Songwriter Chart. Eligible projects were active between April 1, 2019 to May 31, 2020. Now in its 32nd year, the MusicRow Awards are Nashville’s longest-running music industry trade publication honors. In addition to established awards for Producer of the TABLE OF CONTENTS Year, Song of the Year, Breakthrough Artist of the Year, Breakthrough Songwriter, and Breakthrough Artist- Category 1: Producer of the Year .........................................................4 Writer; the MusicRow Awards expanded with the Category 2: Label of the Year ...............................................................8 additional categories Label of the Year, Talent Agency Category 3: Talent Agency of the Year ..............................................10 of the Year, Robert K. Oermann Discovery Artist of the Category 4: Breakthrough Songwriter of the Year .........................13 Year, Male and Female Songwriters of the Year, and Artist Category 5: Breakthrough Artist-Writer of the Year .......................19 of the Year in 2019. -

ED 194 419 EDRS PRICE Jessup, John E., Jr.: Coakley, Robert W. A
r r DOCUMENT RESUME ED 194 419 SO 012 941 - AUTHOR Jessup, John E., Jr.: Coakley, Robert W. TITLE A Guide to the Study and use of Military History. INSTITUTION Army Center of Military History, Washington, D.C. PUB DATE 79 NOTE 497p.: Photographs on pages 331-336 were removed by ERIC due to poor reproducibility. AVAILABLE FROM Superintendent of Documents, U.S. Government Printing Office, Washington, DC 20402 ($6.50). EDRS PRICE MF02/PC20 Plus Postage. DESCRIPTORS *History: military Personnel: *Military Science: *Military Training: Study Guides ABSTRACT This study guide On military history is intended for use with the young officer just entering upon a military career. There are four major sections to the guide. Part one discusses the scope and value of military history, presents a perspective on military history; and examines essentials of a study program. The study of military history has both an educational and a utilitarian value. It allows soldiers to look upon war as a whole and relate its activities to the periods of peace from which it rises and to which it returns. Military history also helps in developing a professional frame of mind and, in the leadership arena, it shows the great importance of character and integrity. In talking about a study program, the guide says that reading biographies of leading soldiers or statesmen is a good way to begin the study of military history. The best way to keep a study program current is to consult some of the many scholarly historical periodicals such as the "American Historical Review" or the "Journal of Modern History." Part two, which comprises almost half the guide, contains a bibliographical essay on military history, including great military historians and philosophers, world military history, and U.S. -

An Austro-Libertarian View, Vol. III
An Austro-Libertarian View, Vol. III An Austro-Libertarian View ESSAYS BY DAVID GORDON VOLUME III CURRENT AFFAIRS • FOREIGN POLICY AMERICAN HISTORY • EUROPEAN HISTORY Mises Institute 518 West Magnolia Avenue Auburn, Alabama 36832-4501 334.321.2100 www.mises.org An Austro-Libertarian View: Essays by David Gordon. Vol. III: Current Affairs, Foreign Policy, American History, European History. Published 2017 by the Mises Institute. This work is licensed under Creative Commons Attribution-NonCommerical-NoDerivs 4.0 Interna- tional License: http://creativecommons.org/licenses/by-nc-nd/4.0/. ISBN: 978-1-61016-673-7 Table of Contents by Chapter Titles Preface . xiii Foreword . 1 Current Affairs A Propensity to Self-Subversion . 5 “Social Security and Its Discontents” . 9 Achieving Our Country: Leftist Thought in 20th-Century America . 11 The Irrepressible Rothbard: The Rothbard-Rockwell Report Essays of Murray N. Rothbard . 17 While America Sleeps: Self-Delusion, Military Weakness, and the Threat to Peace Today . 23 The War Over Iraq: Saddam’s Tyranny and America’s Mission . 29 Why We Fight: Moral Clarity and the War on Terrorism . 35 Speaking of Liberty . 39 Against Leviathan: Government Power and a Free Society . 45 No Victory, No Peace . 51 Resurgence of the Warfare State: The Crisis Since 9/11 . 57 In Our Hands: A Plan to Replace the Welfare State . 63 World War IV: The Long Struggle Against Islamofascism . 71 Radicals for Capitalism: A Freewheeling History of the Modern American Libertarian Movement . 77 The Meaning of Sarkozy . 85 The Power Problem: How American Military Dominance Makes Us Less Safe, Less Prosperous, and Less Free .