Pharmacological Mechanisms of Analgesic Nephropathy JULIAN H
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacokinetics of Salicylic Acid Following Intravenous and Oral Administration of Sodium Salicylate in Sheep
animals Article Pharmacokinetics of Salicylic Acid Following Intravenous and Oral Administration of Sodium Salicylate in Sheep Shashwati Mathurkar 1,*, Preet Singh 2 ID , Kavitha Kongara 2 and Paul Chambers 2 1 1B, He Awa Crescent, Waikanae 5036, New Zealand 2 School of Veterinary Sciences, College of Sciences, Massey University, Palmerston North 4474, New Zealand; [email protected] (P.S.); [email protected] (K.K.); [email protected] (P.C.) * Correspondence: [email protected]; Tel.: +64-221-678-035 Received: 13 June 2018; Accepted: 16 July 2018; Published: 18 July 2018 Simple Summary: Scarcity of non-steroidal anti-inflammatory drugs (NSAID) to minimise the pain in sheep instigated the current study. The aim of this study was to know the pharmacokinetic parameters of salicylic acid in New Zealand sheep after administration of multiple intravenous and oral doses of sodium salicylate (sodium salt of salicylic acid). Results of the study suggest that the half-life of the drug was shorter and clearance was faster after intravenous administration as compared to that of the oral administration. The minimum effective concentration required to produce analgesia in humans (16.8 µL) was achieved in sheep for about 0.17 h in the current study after intravenous administration of 100 and 200 mg/kg body weight of sodium salicylate. However, oral administration of these doses failed to achieve the minimum effective concentration as mentioned above. This study is of significance as it adds valuable information on pharmacokinetics and its variation due to breed, species, age, gender and environmental conditions. -
Orphenadrine Hydrochloride 50Mg/5Ml Oral Solution Rare (Affect More Than 1 in 10,000 People) N Forgetting Things More Than Usual
Uncommon (affect more than 1 in 1000 people) n Constipation Package Leaflet: Information for the user n Greater sensitivity to things around you or feeling nervous n Feeling light-headed and an unusual feeling of excitement (elation) n Difficulty sleeping or feeling tired. Orphenadrine Hydrochloride 50mg/5ml Oral Solution Rare (affect more than 1 in 10,000 people) n Forgetting things more than usual. Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. Reporting of side effects n Keep this leaflet. You may need to read it again. If you get any side effects, talk to your doctor, n If you have any further questions, ask your doctor pharmacist or nurse. This includes any possible side or pharmacist. effects not listed in this leaflet. You can also report n This medicine has been prescribed for you only. side effects directly (see details below). By reporting Do not pass it on to others. It may harm them, even side effects you can help provide more information on if their signs of illness are the same as yours. the safety of this medicine. n If you get any side effects, talk to your doctor or United Kingdom pharmacist. This includes any possible side effects not listed in this Yellow Card Scheme leaflet. See section 4. Website: www.mhra.gov.uk/yellowcard or search for MHRA Yellow Card in the Google Play or What is in this leaflet: Apple App Store. 1. What Orphenadrine Hydrochloride Oral Solution is and what is it used for 2. -

Management of Poisoning
MOH CLINICAL PRACTICE GUIDELINES December/2011 Management of Poisoning Health Ministry of Sciences Chapter of Emergency College of College of Family Manpower Authority Physicians Physicians, Physicians Academy of Medicine, Singapore Singapore Singapore Singapore Medical Pharmaceutical Society Society for Emergency Toxicology Singapore Paediatric Association of Singapore Medicine in Singapore Society (Singapore) Society Executive summary of recommendations Details of recommendations can be found in the main text at the pages indicated. Principles of management of acute poisoning – resuscitating the poisoned patient GPP In a critically poisoned patient, measures beyond standard resuscitative protocol like those listed above need to be implemented and a specialist experienced in poisoning management should be consulted (pg 55). GPP D Prolonged resuscitation should be attempted in drug-induced cardiac arrest (pg 55). Grade D, Level 3 1 C Titrated doses of naloxone, together with bag-valve-mask ventilation, should be administered for suspected opioid-induced coma, prior to intubation for respiratory insuffi ciency (pg 56). Grade C, Level 2+ D In bradycardia due to calcium channel or beta-blocker toxicity that is refractory to conventional vasopressor therapy, intravenous calcium, glucagon or insulin should be used (pg 57). Grade D, Level 3 B Patients with actual or potential life threatening cardiac arrhythmia, hyperkalaemia or rapidly progressive toxicity from digoxin poisoning should be treated with digoxin-specifi c antibodies (pg 57). Grade B, Level 2++ B Titrated doses of benzodiazepine should be given in hyperadrenergic- induced tachycardia states resulting from poisoning (pg 57). Grade B, Level 1+ D Non-selective beta-blockers, like propranolol, should be avoided in stimulant toxicity as unopposed alpha agonism may worsen accompanying hypertension (pg 57). -

Epithelial Delamination Is Protective During Pharmaceutical-Induced Enteropathy
Epithelial delamination is protective during pharmaceutical-induced enteropathy Scott T. Espenschieda, Mark R. Cronana, Molly A. Mattya, Olaf Muellera, Matthew R. Redinbob,c,d, David M. Tobina,e,f, and John F. Rawlsa,e,1 aDepartment of Molecular Genetics and Microbiology, Duke University School of Medicine, Durham, NC 27710; bDepartment of Chemistry, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599; cDepartment of Biochemistry, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC 27599; dDepartment of Microbiology and Immunology, University of North Carolina at Chapel Hill School of Medicine, Chapel Hill, NC 27599; eDepartment of Medicine, Duke University School of Medicine, Durham, NC 27710; and fDepartment of Immunology, Duke University School of Medicine, Durham, NC 27710 Edited by Dennis L. Kasper, Harvard Medical School, Boston, MA, and approved July 15, 2019 (received for review February 12, 2019) Intestinal epithelial cell (IEC) shedding is a fundamental response to in mediating intestinal responses to injury remains poorly un- intestinal damage, yet underlying mechanisms and functions have derstood for most xenobiotics. been difficult to define. Here we model chronic intestinal damage in Gastrointestinal pathology is common in people using phar- zebrafish larvae using the nonsteroidal antiinflammatory drug maceuticals, including nonsteroidal antiinflammatory drugs (NSAID) Glafenine. Glafenine induced the unfolded protein response (NSAIDs) (11). While gastric ulceration has historically been a (UPR) and inflammatory pathways in IECs, leading to delamination. defining clinical presentation of NSAID-induced enteropathy, Glafenine-induced inflammation was augmented by microbial colo- small intestinal pathology has also been observed, although the nizationandassociatedwithchanges in intestinal and environmental incidence may be underreported due to diagnostic limitations microbiotas. -

Risk Based Requirements for Medicines Handling
Risk based requirements for medicines handling Including requirements for Schedule 4 Restricted medicines Contents 1. Introduction 2 2. Summary of roles and responsibilities 3 3. Schedule 4 Restricted medicines 4 4. Medicines acquisition 4 5. Storage of medicines, including control of access to storage 4 5.1. Staff access to medicines storage areas 5 5.2. Storage of S4R medicines 5 5.3. Storage of S4R medicines for medical emergencies 6 5.4. Access to storage for S4R and S8 medicines 6 5.5. Pharmacy Department access, including after hours 7 5.6. After-hours access to S8 medicines in the Pharmacy Department 7 5.7. Storage of nitrous oxide 8 5.8. Management of patients’ own medicines 8 6. Distribution of medicines 9 6.1. Distribution outside Pharmacy Department operating hours 10 6.2. Distribution of S4R and S8 medicines 10 7. Administration of medicines to patients 11 7.1. Self-administration of scheduled medicines by patients 11 7.2. Administration of S8 medicines 11 8. Supply of medicines to patients 12 8.1. Supply of scheduled medicines to patients by health professionals other than pharmacists 12 9. Record keeping 13 9.1. General record keeping requirements for S4R medicines 13 9.2. Management of the distribution and archiving of S8 registers 14 9.3. Inventories of S4R medicines 14 9.4. Inventories of S8 medicines 15 10. Destruction and discards of S4R and S8 medicines 15 11. Management of oral liquid S4R and S8 medicines 16 12. Cannabis based products 17 13. Management of opioid pharmacotherapy 18 14. -

Sodium-Salicylate-European-Public-Mrl-Assessment-Report-Epmar-Committee-Veterinary
27 October 2010 EMA/CVMP/562066/2007 Veterinary Medicines and Product Data Management Committee for Medicinal Products for Veterinary Use European public MRL assessment report (EPMAR) Sodium salicylate (turkeys) On 12 October 2010 the European Commission adopted a Regulation1 establishing provisional maximum residue limits for sodium salicylate in turkeys, valid throughout the European Union. These provisional maximum residue limits were based on the favourable opinion and the assessment report adopted by the Committee for Medicinal Products for Veterinary Use. In turkeys, sodium salicylate is intended for use orally as an antipyretic in the treatment of acute respiratory diseases. Sodium salicylate was previously assessed for the purpose of establishing maximum residue limits and was entered in Annex II of Regulation (EEC) No 2377/902 (no MRL required) for topical use in all food producing species except fish and for oral use in bovine and porcine species. Chevita Tierarzneimittel GmbH submitted to the European Medicines Agency on 4 January 2007 an application for the extension of existing entry in Annex II of Regulation (EEC) No 2377/90 for sodium salicylates to turkeys. On 12 December 2007 the Committee for Medicinal Products for Veterinary Use adopted an opinion recommending the amendment of the entry in Annex II of Regulation (EEC) No 2377/90 to include sodium salicylate for oral use in turkeys. The European Commission subsequently returned the opinion to the Committee to consider whether its opinion should be reviewed to take into account issues raised during the Commission’s inter service consultation and in particular to consider whether establishment of maximum residue limits for sodium salicylate in turkeys should be established. -

Prescription Regulations Summary Chart Who Hold an Approval to Prescribe Methadone from Their
Products included in the Triplicate Prescription Program* This is a reference list provided for convenience. While all generic medication names appear, only sample brand names are provided and it should not be viewed as an all-inclusive listing of all trade names of drugs included in the Triplicate Prescription Program. BUPRENORPHINE METHADONE BuTrans, Suboxone** Metadol, Methadose - May only be prescribed by physicians Prescription regulations summary chart who hold an approval to prescribe methadone from their BUTALBITAL PREPARATIONS provincial regulatory body*** Summary of federal and provincial laws governing prescription drug ordering, Fiorinal, Fiorinal C ¼ & C ½, Pronal, Ratio-Tecnal, records, prescription requirements, and refills Ratio-Tecnal C ¼ & C ½, Trianal, Trianal C ½ METHYLPHENIDATE Biphentin®, Foquest®, and Concerta® brands are excluded Revised 2019 BUTORPHANOL from TPP prescr ip t i o n p a d req u ir e m e n t s (generic versions Butorphanol NS, PMS-Butorphanol, Torbutrol (Vet), of these products require a triplicate presc ription) Torbugesic (Vet) Apo-Methyphenidate, PHL-Methylphenidate, PMS- Prescription regulations DEXTROPROPOXYPHENE Methylphenidate, PMS-Methylphenidate ER, Ratio- None identified Methylphenidate, Ritalin, Ritalin SR, Sandoz- According to the Standards of Practice for Pharmacists and Pharmacy Technicians: Methylphenidate SR, Teva-Methylphenidate ER-C FENTANYL/SUFENTANIL/ALFENTANIL 6.4 Neither a pharmacist nor a pharmacy technician may dispense a drug or blood product under a Alfentanil Injection, -

Synthesis and Pharmacological Evaluation of Fenamate Analogues: 1,3,4-Oxadiazol-2-Ones and 1,3,4- Oxadiazole-2-Thiones
Scientia Pharmaceutica (Sci. Pharm.) 71,331-356 (2003) O Osterreichische Apotheker-Verlagsgesellschaft m. b.H., Wien, Printed in Austria Synthesis and Pharmacological Evaluation of Fenamate Analogues: 1,3,4-Oxadiazol-2-ones and 1,3,4- Oxadiazole-2-thiones Aida A. ~l-~zzoun~'*,Yousreya A ~aklad',Herbert ~artsch~,~afaaA. 2aghary4, Waleed M. lbrahims, Mosaad S. ~oharned~. Pharmaceutical Sciences Dept. (Pharmaceutical Chemistry goup' and Pharmacology group2), National Research Center, Tahrir St. Dokki, Giza, Egypt. 3~nstitutflir Pharmazeutische Chemie, Pharrnazie Zentrum der Universitilt Wien. 4~harmaceuticalChemistry Dept. ,' Organic Chemistry Dept. , Helwan University , Faculty of Pharmacy, Ein Helwan Cairo, Egypt. Abstract A series of fenamate pyridyl or quinolinyl analogues of 1,3,4-oxadiazol-2-ones 5a-d and 6a-r, and 1,3,4-oxadiazole-2-thiones 5e-g and 6s-v, respectively, have been synthesized and evaluated for their analgesic (hot-plate) , antiinflammatory (carrageenin induced rat's paw edema) and ulcerogenic effects as well as plasma prostaglandin E2 (PGE2) level. The highest analgesic activity was achieved with compound 5a (0.5 ,0.6 ,0.7 mrnolkg b.wt.) in respect with mefenamic acid (0.4 mmollkg b.wt.). Compounds 6h, 61 and 5g showed 93, 88 and 84% inhibition, respectively on the carrageenan-induced rat's paw edema at dose level of O.lrnrnol/kg b.wt, compared with 58% inhibition of mefenamic acid (0.2mmoll kg b.wt.). Moreover, the highest inhibitory activity on plasma PGE2 level was displayed also with 6h, 61 and 5g (71, 70,68.5% respectively, 0.lmmolkg b.wt.) compared with indomethacin (60%, 0.01 mmolkg b.wt.) as a reference drug. -

NINDS Custom Collection II
ACACETIN ACEBUTOLOL HYDROCHLORIDE ACECLIDINE HYDROCHLORIDE ACEMETACIN ACETAMINOPHEN ACETAMINOSALOL ACETANILIDE ACETARSOL ACETAZOLAMIDE ACETOHYDROXAMIC ACID ACETRIAZOIC ACID ACETYL TYROSINE ETHYL ESTER ACETYLCARNITINE ACETYLCHOLINE ACETYLCYSTEINE ACETYLGLUCOSAMINE ACETYLGLUTAMIC ACID ACETYL-L-LEUCINE ACETYLPHENYLALANINE ACETYLSEROTONIN ACETYLTRYPTOPHAN ACEXAMIC ACID ACIVICIN ACLACINOMYCIN A1 ACONITINE ACRIFLAVINIUM HYDROCHLORIDE ACRISORCIN ACTINONIN ACYCLOVIR ADENOSINE PHOSPHATE ADENOSINE ADRENALINE BITARTRATE AESCULIN AJMALINE AKLAVINE HYDROCHLORIDE ALANYL-dl-LEUCINE ALANYL-dl-PHENYLALANINE ALAPROCLATE ALBENDAZOLE ALBUTEROL ALEXIDINE HYDROCHLORIDE ALLANTOIN ALLOPURINOL ALMOTRIPTAN ALOIN ALPRENOLOL ALTRETAMINE ALVERINE CITRATE AMANTADINE HYDROCHLORIDE AMBROXOL HYDROCHLORIDE AMCINONIDE AMIKACIN SULFATE AMILORIDE HYDROCHLORIDE 3-AMINOBENZAMIDE gamma-AMINOBUTYRIC ACID AMINOCAPROIC ACID N- (2-AMINOETHYL)-4-CHLOROBENZAMIDE (RO-16-6491) AMINOGLUTETHIMIDE AMINOHIPPURIC ACID AMINOHYDROXYBUTYRIC ACID AMINOLEVULINIC ACID HYDROCHLORIDE AMINOPHENAZONE 3-AMINOPROPANESULPHONIC ACID AMINOPYRIDINE 9-AMINO-1,2,3,4-TETRAHYDROACRIDINE HYDROCHLORIDE AMINOTHIAZOLE AMIODARONE HYDROCHLORIDE AMIPRILOSE AMITRIPTYLINE HYDROCHLORIDE AMLODIPINE BESYLATE AMODIAQUINE DIHYDROCHLORIDE AMOXEPINE AMOXICILLIN AMPICILLIN SODIUM AMPROLIUM AMRINONE AMYGDALIN ANABASAMINE HYDROCHLORIDE ANABASINE HYDROCHLORIDE ANCITABINE HYDROCHLORIDE ANDROSTERONE SODIUM SULFATE ANIRACETAM ANISINDIONE ANISODAMINE ANISOMYCIN ANTAZOLINE PHOSPHATE ANTHRALIN ANTIMYCIN A (A1 shown) ANTIPYRINE APHYLLIC -

Extraction and Evaporation: Experiment 1 Separating the Components of a Mixture1 Week 1
Organic Chemistry I Laboratory Extraction and Evaporation: Experiment 1 Separating the Components of a Mixture1 Week 1 Background Reading Zubrick, J. W. The Organic Chem Lab Survival Manual, 4th edition, Wiley & Sons, Inc., New York, 1997. Keeping a Notebook: Pg 12-24. Interpreting Handbooks: Pg 26-31, 34-44. Extraction and Washing: Pg 148-168. Background Senario One of the many places organic chemists are employed is in private laboratories associated with consulting firms. The purpose of these labs is generally to provide chemical analysis or synthesis of material for customers. The first few labs in CHM 220 will teach you the basic techniques needed to analyze and purify mixtures to determine the individual components. This first lab will involve determining the composition of a possible pharmaceutical preparation. Watchdog agencies exist which monitor the pharmaceuticals sold over the counter in the United States. These agencies will use private laboratory firms to analyze products suspected of violating enforced standards. For example, a new brand of analgesic may appear on drugstore shelves at a low price. The label indicates that the tablets were manufactured in the United States by a legitimate pharmaceutical company. However, the labels may reveal discrepancies and the appearance/quality of the tablets could lead an investigator to suspect that they might be counterfeit. Such knockoffs of a domestic product can be manufactured cheaply elsewhere and smuggled into the US, where they are sold for high profits. This laboratory exercise places you in the position of analyzing a suspected counterfeit analgesic preparation. The label on the suspected bottle lists the ingredients per tablet as aspirin (200 mg), acetaminophen (250 mg), and sucrose (50 mg). -

Acute Poisoning: Understanding 90% of Cases in a Nutshell S L Greene, P I Dargan, a L Jones
204 REVIEW Postgrad Med J: first published as 10.1136/pgmj.2004.027813 on 5 April 2005. Downloaded from Acute poisoning: understanding 90% of cases in a nutshell S L Greene, P I Dargan, A L Jones ............................................................................................................................... Postgrad Med J 2005;81:204–216. doi: 10.1136/pgmj.2004.024794 The acutely poisoned patient remains a common problem Paracetamol remains the most common drug taken in overdose in the UK (50% of intentional facing doctors working in acute medicine in the United self poisoning presentations).19 Non-steroidal Kingdom and worldwide. This review examines the initial anti-inflammatory drugs (NSAIDs), benzodiaze- management of the acutely poisoned patient. Aspects of pines/zopiclone, aspirin, compound analgesics, drugs of misuse including opioids, tricyclic general management are reviewed including immediate antidepressants (TCAs), and selective serotonin interventions, investigations, gastrointestinal reuptake inhibitors (SSRIs) comprise most of the decontamination techniques, use of antidotes, methods to remaining 50% (box 1). Reductions in the price of drugs of misuse have led to increased cocaine, increase poison elimination, and psychological MDMA (ecstasy), and c-hydroxybutyrate (GHB) assessment. More common and serious poisonings caused toxicity related ED attendances.10 Clinicians by paracetamol, salicylates, opioids, tricyclic should also be aware that severe toxicity can result from exposure to non-licensed pharmaco- -
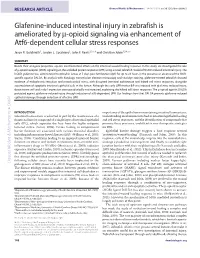
Glafenine-Induced Intestinal Injury in Zebrafish Is Ameliorated by -Opioid Signaling Via Enhancement of Atf6-Dependent Cellular Stress Responses
RESEARCH ARTICLE Disease Models & Mechanisms 6, 146-159 (2013) doi:10.1242/dmm.009852 Glafenine-induced intestinal injury in zebrafish is ameliorated by -opioid signaling via enhancement of Atf6-dependent cellular stress responses Jason R. Goldsmith1, Jordan L. Cocchiaro2, John F. Rawls2,3,*,‡ and Christian Jobin1,3,4,*,‡ SUMMARY Beside their analgesic properties, opiates exert beneficial effects on the intestinal wound healing response. In this study, we investigated the role of -opioid receptor (MOR) signaling on the unfolded protein response (UPR) using a novel zebrafish model of NSAID-induced intestinal injury. The NSAID glafenine was administered to zebrafish larvae at 5 days post-fertilization (dpf) for up to 24 hours in the presence or absence of the MOR- specific agonist DALDA. By analysis with histology, transmission electron microscopy and vital dye staining, glafenine-treated zebrafish showed evidence of endoplasmic reticulum and mitochondrial stress, with disrupted intestinal architecture and halted cell stress responses, alongside accumulation of apoptotic intestinal epithelial cells in the lumen. Although the early UPR marker BiP was induced with glafenine-induced injury, downstream atf6 and s-xbp1 expression were paradoxically not increased, explaining the halted cell stress responses. The -opioid agonist DALDA protected against glafenine-induced injury through induction of atf6-dependent UPR. Our findings show that DALDA prevents glafenine-induced epithelial damage through induction of effective UPR. DMM INTRODUCTION importance of the epithelium in maintaining intestinal homeostasis, Intestinal homeostasis is achieved in part by the maintenance of a understanding mechanisms involved in intestinal epithelial healing functional barrier composed of a single layer of intestinal epithelial and cell stress responses, and the identification of compounds that cells (IEC), which separates the host from the highly antigenic promote these processes, could lead to new therapeutic strategies lumenal milieu (Sartor, 2008).