TB India 2017.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

GOVERNMENT of TELANGANA ABSTRACT Public Services
GOVERNMENT OF TELANGANA ABSTRACT Public Services – Formation /Reorganization of New Districts, Revenue Divisions and Mandals in Telangana State – Re-organization of Circles/Divisions/Sub- Divisions/Mandals in all cadres - Orders – Issued. PANCHAYAT RAJ & RURAL DEVELOPMENT (PR.I) DEPARTENT G.O.Ms.No.71 Dt:11.10.2016 Read the following:- 1. G.O.Ms.No.5, PR&RD(Estt.I) Dept. Dt:16.01.2015 and subsequent amendments, G.O.Ms.No.45, dt:23.5.2015, G.O.Ms.No.59, dt:31.7.2015 and G.O.Ms.No.6, dt:13.01.2016. 2. G.O.Ms.No.221 to 250, Revenue (DA-CMRF) Department, dt:11.10.2016 3. G.O.Ms.No.144, Finance (HRM.I) Department, dt:11.10.2016 4. From the E-in-C, PR, Hyderbad Letter No.B-II/Reorg.district/ 338/2016, Dt.17.9.2016, Dt:29.9.2016 & Dt:08.10.2016. ORDER: In the reference first read above Government have issued orders rationalising the PRI, PIU & Q C wings for effective implementation of works programme in PRED to achieve the targets of the Govt. 2. In the reference second read above Government of Telangana have issued notifications for formation/reorganization of Districts, Divisions and Mandals in the State of Telangana for better administration and development of areas concerned. 3. In the reference 3rd read above, Government have issued orders re- distributing cadre strength among (30) districts. 4. In the reference fourth read above the Engineer-in-Chief, PR has submitted proposals for re-organization of PRED to be co-terminus with the new districts jurisdiction and to change the nomenclature of Superintending Engineer, PR as Regional officer and Executive Engineer of the District Office as District Panchayat Raj Engineer (DPRE). -
JEET Annual Report
It’s Time Joint Effort for Elimination of Tuberculosis (JEET) Annual Report 2018 i Annual Report 2018 iii Annual Report 2018 Welcome to the JEET Annual Report Last year was momentous. Through the JEET (Joint Effort for Elimination of Tuberculosis) partnership, we were able to launch the most comprehensive TB intervention yet, to engage the elusive private healthcare sector in India. JEET takes learnings from previous successful private sector linkage models conducted in Mumbai and Mehsana along with FIND’s widely cited 10 city paediatric TB intervention and scales across the entire nation, covering a population of 996 million across 24 States. India has the dubious distinction of contributing the highest number of tuberculosis cases globally. With an estimated annual incidence of 2.74 million cases, it is not an overstatement that India single- handedly sways global TB statistics. Currently, out of the 2.74 million, only about 1.9 million persons (70%) are reported to the National Tuberculosis Programme (NTP). The remaining are either left undiagnosed or seek care of unknown or sub-standard quality in the unorganised private sector. The RNTCP in India launched the aspirational National Strategic Plan 2017-2025 which aims for elimination of TB from India by 2025. However, it is critical to engage the private sector to reach this ambitious goal. This realisation and need to engage the private sector has been at the foundation of genesis of JEET. JEET aims to generate “top of the mind” awareness amongst private providers regarding TB diagnosis and treatment options. Patients approaching private providers and clinics often have high “customer service” expectations, hence JEET ensures seamless linkages to free public sector testing and treatment for patients accessing care in private sector. -

2018062987.Pdf
.. Notice No.Al/1620/2016-1 NOTICE Sub:- P.S. - TS&SSR 2015 - Naib Tahsildars - Adilabad District - Provisional Adhoc Annual Panel for the year 2015-16 approved by the CCLA, TS, Hyderabad - Published - Objections filed for revision of seniority - Notice Issued for revision of seniorit,{'in-']UftY&r'o'AssistZll1fS""'cfRCf'Se'hTbf"ASsistant Cadre - Reg. Ref:-1.CCLA, TS, Hyderabad Ref.No.Ser.II(2)/1332/2016, Dated: 10.12.2016 2. CCLA, TS, Hyderabad Ref.No.Ser.II (1)/516/2018, Dated: 02.05.2018. 3. Collector, Adilabad Notice No.A1/1620/2016, Dated: 03.05.20.18 4. Smt.K.Srilatha, Naib Tahsildar % RDO Adilabad of Adilabad District Dat ed: 08. 05.20 18'" ..k-··"'·"· .." -:"., .r"'-'P«"····ti"..;}".,.:·8,>:<;'?1"'~,""'··1;.',--'" ':"'~ 5. Collector, Adilabad Lr.No.A1/1620/2016, Dated: 11.06.2018 6. CCLA, TS, Hyderabad Ref.No.Ser.II(2)/1332/2016, Dated: 22.06.2018 $$$ The Chief Commissioner of Land Adrnlnlstration, T.S., Hyderabad vide reference 1st cited has communicated the approved adhoc Naib Tahsildars Panel for the year 2015-16 pertains to Adilabad District and requested to publish the same in all Revenue office calling claims and objections if any within (07) days. Further, the Chief Commissioner of Land Administration, T.S., Hyderabad has requested to furnish publication certificate of above Naib Tahsildars panel. Accordingly, the above approved adhoc Naib Tahsildars Panel for the year 2015-16 of Adilabad District (R'ecefVea/thro'u~:jhVreference'lst cited) has been published at Notice Board of Collectorate, Adilabad, District and requested the District Collector, Mancherial, Asifabad and Nirmal, all the Revenue Divisional Officers, all the Tahsildars and officers concerned to publish the same in the notice boards of their jurisdiction vide Collector, Adilabad Notice No.A1/1620/2016, dated 03-05-2018. -

Telangana State Information Commission
TELANGANA STATE INFORMATION COMMISSION (Under Right to Information Act, 2005) Samachara Hakku Bhavan, D.No.5-4-399, ‘4’ Storied Commercial Complex, Housing Board Building, Mojam Jahi Market, Hyderabad – 500 001. Phone Nos: 040-24740107 (o); 040-24740592(f) Appeal No. 5091/CIC/2018 Dated: 19-8-2019 Appellant : Sri Medi Lakshmi Rajam, Mancherial District Respondent : The Public Information Officer (U/RTI Act, 2005) / O/o. the Circle Inspector of Police, Luxettipet, Mancherial District The Appellate Authority (U/RTI Act, 2005) / O/o. the Commissioner of Police, Ramagundam, Peddapalli District. O R D E R Sri Medi Lakshmi Rajam, Mancherial District has filed 2nd appeal dated 22-03-2018 which was received by this Commission on 24-03-2018 for not getting the information sought by him from the PIO / O/o. the Circle Inspector of Police, Luxettipet, Mancherial District and 1st Appellate Authority / O/o. the Commissioner of Police, Ramagundam, Peddapalli District. The brief facts of the case as per the appeal and other records received along with it are that the appellant herein filed an application dated 13-12-2017 before the PIO requesting to furnish the information under Sec.6(1) of the RTI Act, 2005, on the following points mentioned in his application: TSIC The Public Information Officer / O/o. the Circle Inspector of Police, Luxettipet, Mancherial District, Vide Letter No. 27/CI-M/2018, Dated 15-01-2018, has furnished the information to the appellant. Since the appellant did not receive the complete information from the Public Information Officer, he filed 1st appeal dated 29-01-2018 before the 1st Appellate Authority requesting him to furnish the information sought by him u/s 19(1) of the RTI Act, 2005. -

2350/Sic Bm/2018
Telangana State Information Commission (Under Right to Information Act, 2005) D.No.5-4-399, Samachara Hakku Bhavan (Old ACB Building), Mojam-jahi-Market, Hyderabad – 500 001 Phone: 24740666 Fax: 24740592 Appeal No: 2350/SIC-BM/2018 Date: 07-08-2019 Appellant : Sri. Md. Ashraf, Sirpur-Kagaznagar, Komaram Bheem District. Respondents : Public Information Officer (U/RTI Act, 2005) O/o the District Intermediate Education Officer, Mancherial & Peddapalli, Mancherial District. First Appellate Authority (U/RTI Act, 2005) O/o the District Intermediate Education Officer, Mancherial & Peddapalli, Mancherial District. Order Sri. Md. Ashraf, Sirpur-Kagaznagar, Komaram Bheem District has filed an appeal dated 29-01-2018 which was received by this Commission on 09-02-2018 for not getting the information sought by him from the PIO / O/o the District Intermediate Education Officer, Mancherial & Peddapalli, Mancherial District and the First Appellate Authority / O/o the District Intermediate Education Officer, Mancherial & Peddapalli, Mancherial District. The brief facts of the case as per the appeal and other records received along with it are that the appellant herein filed an application u/s 6(1) of the RTI Act, 2005 datedTSIC 09-10-2017 before the PIO requesting to furnish the below information: The District Intermediate Education Officer, Mancherial & Peddapalli, Mancherial District vide letter No: 132/RTI/2017 dated: 30-11-2017 informed the appellant that the information sought is bulk information hence requested to obtain the information from the concerned colleges. Note: This is system generated copy and no signature is required Stating that the PIO furnished incomplete information, the appellant filed 1st appeal dated 29-01-2018 before the First Appellate Authority u/s 19(1) of RTI Act 2005 requesting to take steps for furnishing the information sought by him. -
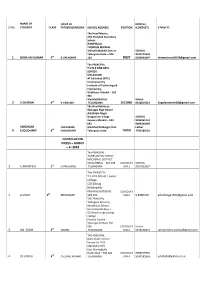
S.No. 1 FIRST 2 SECOND 3 THIRD CONSOLATION PRIZES – GROUP
NAME OF NAME OF MOB.No. S.No. STUDENT CLASS FATHER/GUARDIAN SCHOOL ADDRESS POSITION (CONTACT) E-Mial ID The Head Master, Zilla Parishad Secondary School, HARIPIRALA THORRUR MANDAL MAHABUBABAD District SCHOOL Telangana State – 506 9247175659 1 BOGA SAI KUMAR 6th B.UPENDHER 163 FIRST 8200904407 [email protected] The PRINCIPAL T S W R FINE ARTS SCHOOL MALKAJGIRI AT Edulabad (KITE) Krishnamurthy Institute of Technology & Engineering Ghatkesar Mandal – 501 301 Medchal District School 2 V.CHARAN 6th V.YADAIAH TELANGANA SECOND 9440014522 [email protected] The Head Mistress, Shivappa High School Adj.Shilpa Nagar Naagaaram Village SCHOOL Keesara Mandal – 500 9290261151 083 9000244089 VERENDAR LAKHARAM Medchal/Malkajgiri Dist. Father 3 CHOUDHARY 6th CHOUDHARY Telangana State THIRD 7702589181 CONSOLATION PRIZES – GROUP – A: 2019 The PRINCIPAL TSWRS (BOYS) SCHOOL MACHERIAL DISTRICT MANCHERIAL – 504 208 CONSOLAT SCHOOL 1 G.ARUNTEJA 6th G.RAJALINGU TELANGANA ION-1 9014923037 The PRINCIPAL T.S.W.R.School / Junior College COE (Boys) Bellampally Mancherial District CONSOLAT 2 A.VINAY 6th BHUMAIAH 504 251 ION-2 9.848E+09 [email protected] THE PRINCIPAL Telangana Minority Residential School Hanamkonda Boys-I Old Arushi Engineering College Punnel, Inavole Warangal (Urban) 506 005 CONSOLAT School 3 Md. SADIK 6th JAMEEL TELANGANA ION-3 9948190673 [email protected] THE PRINCIPAL Delhi Public School Survey No.74/9 Mahendra Hills East Marredpally Hyderabad – 500 026 CONSOLAT 9989279910 4 Ch.JUNALI 6th Ch.SUNIL KUMAR TELANGANA ION-4 -

Combined-Adilabad-Districts-4.Pdf
We acknowledge the content from http://nirmal.telangana.gov.in/district-profile The Nirmal district is etched out of erstwhile Adilabad District. The district is located in northern Telangana and borders Maharashtra and the Telangana districts of Asifabad (Komuram Bheem), Adilabad, Mancherial, Jagtial and Nizamabad. The district has two revenue divisions – Nirmal and Bhainsa and 19 mandals, while the district headquarters is located at Nirmal town. Nirmal District derives its name from the king Nimma Rayudu, who played a pivotal role in the development of the region. The district has a great networking of roadways, with the National Highway 44 crisscrossing the district. It has two major RTC depots at Nirmal and at Bhainsa. The district treasures some of the most fertile land in Telangana, with the river Godavari forming the southern border of the district and many small and medium projects being the major irrigation sources. In addition, there are chain tanks built around the Nirmal town. Paddy, cotton, pulses are the primary crops in the district. Nirmal district has rich historical and cultural traditions. It is greatly inclined towards art. Several art forms flourish in the district viz. Bindu Yakshaganam, Bagavatham, Pandavulu, Yellamma Katha, Sharada Kathalu, Kolatam and Jada Koppulu. And the most distinguishing of all, the exotic Nirmal Toys, made of wood, have earned national and international recognition. Travel lovers are sure to find the district a huge attraction for its numerous tourist spots.Sri Gnana Saraswathi Temple situated on the banks of River Godavari at Basar is very famous for Akshara Sweekaram – initiation of children into learning. -

10927/Cic-Bm/2019
TELANGANA STATE INFORMATION COMMISSION (Under Right to Information Act, 2005) Samachara Hakku Bhavan, D.No.5-4-399, ‘4’ Storied Commercial Complex, Housing Board Building, Mojam Jahi Market, Hyderabad – 500 001. Phone Nos: 040-24743399 (O); 040-24740592(F) Appeal No.10927/CIC/2019, Order dated:30-06-2021 Appellant : Sri RAVINDER G, Dandepalli Village & Mandal, Mancherial District. Respondents: The Public Information Officer (U/RTI Act,2005)/ O/o the Station House Officer, Mancherial Police Station, Mancherial Mandal, Mancherial District. Copy to: The First Appellate Authority (U/RTI Act, 2005)/ O/o the Commissioner of Police - Ramagundam, Ramagundam, Peddapalli District. ORDER Sri G. Ravinder has filed 2nd appeal on 13-09-2019 which was received by this Commission on 18-09-2019 for not getting the information sought by him from the Public Information Officer/ O/o the Circle Inspector Police, Mancherial Police Station, Mancherial Mandal, Mancherial District and the First Appellate Authority/ O/o the Commissioner Of Police , Ramagundam, Peddapalli District. The brief facts of this case as per the appeal and other records received along with it are that the appellant herein filed an application dated.12-07-2019 before the Public Information Officer requesting to furnish the information under Sec. 6(1) of the RTI Act, 2005 on the following points mentioned: The PublicTSIC Information Officer, vide Endorsement Lr.No. –Nil- dated 10.08.2019, furnished reply to the appellant. Stating that he is not satisfied with the reply received from the Public Information Officer, the appellant filed 1st appeal dated.26-08-2019 before the First Appellate Authority U/s. -

Under Right to Information Act, 2005) D.No.5-4-399, Samachara Hakku Bhavan (Old ACB Building), Mojam-Jahi-Market, Hyderabad – 500 001 Phone: 24740107, 24740592
Telangana State Information Commission (Under Right to Information Act, 2005) D.No.5-4-399, Samachara Hakku Bhavan (Old ACB Building), Mojam-jahi-Market, Hyderabad – 500 001 Phone: 24740107, 24740592 Appeal No: 24097/SIC-BM/2017, Order dated: 06-12-2018 Appellant : Sri G. Nagaraju, H.No.3-67/4, ACC, Mancherial District – 504 208. Respondents : The Public Information Officer/ (U/RTI Act, 2005) / The Revenue Divisional Officer, Mancherial Division, Mancherial District – 504 208. The First Appellate Authority/ (U/RTI Act, 2005) / The District Revenue Officer, O/o District Collectorate, Mancherial District – 504 208. ORDER Sri G. Nagaraju, H.No.3-67/4, ACC, Mancherial District has filed 2nd appeal dated 30-10-2017 which was received by this Commission on 01-11-2017 for not getting the information sought by him from the Public Information Officer/ Revenue Divisional Officer, Mancherial Division, Mancherial and 1st Appellate Authority/ The District Revenue Officer, O/o District Collectorate, Mancherial. The brief facts of the case as per the appeal and other records received along with it are that the appellant herein filed an application dated: 13-04-2017 before the PIO requesting to furnish the information under Sec.6(1) of the RTI Act, 2005, on the following points mentioned: Stating that the appellant did not receive any information from the Public Information Officer, he filed 1st appeal dated 24-05-2017 before the 1st Appellate Authority requesting him to furnish the information sought by him u/s 19(1) of the RTI Act, 2005. Stating that the appellant did not receive any information from the First Appellate Authority, he preferred this 2nd appeal before this Commission requesting to arrange to furnish the information sought by him u/s 19(3) of the RTI Act, 2005. -

11637/Cic-Srs/2017
TELANGANA STATE INFORMATION COMMISSION (Under Right to Information Act, 2005) Samachara Hakku Bhavan, D.No.5-4-399, ‘4’ Storied Commercial Complex, Housing Board Building, Mojam Jahi Market, Hyderabad – 500 001. Phone Nos: 040-24740107 (o); 040-24740592(f) Appeal No.11637 /CIC/2017 Dated: 7-11-2019 Appellant : Sri Godeisela Chandramogili, Macherial District-504 251 Respondents : 1. The Public Information Officer (U/RTI Act,2005) / O/o. the Chief Commissioner of Land Administration, Telangana State, Nampally Station road, Opp. Annapurna Hotel, Hyderabad-01 2. The Public Information Officer (U/RTI Act,2005) / O/o the District Collector, Mancherial District, Mancherial. 3. The Public Information Officer (U/RTI Act,2005) / O/o the District Collector, Adilabad District, Adilabad The Appellate Authority (U/RTI Act, 2005) / O/o. the Chief Commissioner of Land Administration, Telangana State, Nampally Station road, Opp. Annapurna Hotel, Hyderabad-01 O R D E R 1. Sri Godeisela Chandramogili, Macherial District-504 251 has filed 2nd appeal dated 06-04- 2017 which was received by this Commission on 06-04-2017 for not getting the information sought by him from the PIO /O/o. the Chief Commissioner of Land Administration, Telangana State, Nampally Station road, Opp. Annapurna Hotel, Hyderabad-01 and 1st Appellate Authority / O/o. the Chief Commissioner of Land Administration, Telangana State, Nampally Station road, Opp. Annapurna Hotel, Hyderabad-01 2. The brief facts of the case as per the appeal and other records received along with it are that the appellant herein filed an application dated 17-12-2016 before the PIO requesting to furnish the information under Sec.6(1) of the RTI Act, 2005, on the following points mentioned in his application: TSIC 3. -

Primary Address Location City Mancherial Town And
Primary Address Location City Mancherial Town and Mandal Mancherial District Mancherial Telangana Adilabad Agartala Agartala AGARTALA own, Mouza Sadar Dist West 799001 Agartala AGARTALA Suraj Complex Sadar Bazar Agra Agra Shop No 5, Ground Floor, Kailash Plaza, Shah Market, Agra NA Agra Ground Floor, 6 230, Jagan Plaza, Bharion Park, Belanganj Agra Agra Ground Floor, 9, Laxman Nagar, Arjun Nagar, Agra NA Agra Shop No 7 at LGround Floor, Karim Complex, Fatehabad Road, Agra Agra Shop No B5, Ground Floor, 20 213 B, Silky Mandi Jaipur House, Agra Agra r, Main Market Kasba Jahangirabad, Paragna Tehsil Anoo pshahr, Bulandshahr,Jahangirabad Agra l Municipal No 26 862, Badanpur Kanpur Road, Auriya, Au raiya 206122,Auraiya Agra th Road, Near Galla Mandi Orai, Distt Jalaun 285001 Orai Agra adi Gaon Road Tehsil Konch Distt Jalun 285001 Konch Agra lla Fardanvis, Churki Road, Jalaun U P Jalaun Agra road kosi kalan uttar pradesh 281403 Kosikalan Agra la Road Murari Ka Paich Khurja 203131 Khurja Agra Chandpur Fatak 203001 Bulandshahar Agra Mohalla Sikandrabad Sikandarabad Agra n Road,kasganj Kasganj Agra Hathras 204101 Hathras Agra don Road, Jhansi 284003 Jhansi Agra Road, Aligarh 202001 Aligarh Agra NA Aligarh Agra NA Jhansi Agra NA Agra Agra NA Jhansi Agra NA Aligarh Agra Nagar, Shahganj, MG Road, Agra 282002 Agra Agra ungi, Naurangabad, GT Road, Aligarh 202001 Aligarh Agra h Road, Agra 282005 Agra Agra a, Opp Nagar Nigam, Jhansi 284002 Jhansi Agra a Nagar, Agra 282004 Agra Agra Shrotmuni Ashram, Dist Mathura, 281121 VRINDAVAN Agra abad, 283204 TUNDLA Agra Near Vidya Peeth Inter College, Vidyapeeth Chauraha, Vrindavan Dist. -

Government of India Ministry of Health and Family Welfare Department of Health and Family Welfare Lok Sabha Unstarred Question N
GOVERNMENT OF INDIA MINISTRY OF HEALTH AND FAMILY WELFARE DEPARTMENT OF HEALTH AND FAMILY WELFARE LOK SABHA UNSTARRED QUESTION NO.4235 TO BE ANSWERED ON 13TH DECEMBER, 2019 DIALYSIS CENTRES IN TELANGANA 4235. DR. G. RANJITH REDDY: Will the Minister of HEALTH AND FAMILY WELFARE be pleased to state: (a) the details of dialysis centres set up in the State of Telangana, district-wise; (b) whether the Government is aware that more than 10,000 people are under dialysis in Telangana and if so, the details thereof; (c) whether the Government is aware that dialysis patients are finding it extremely difficult to lead a life as they have to go day-in-and-day-out for dialysis which is crippling their income and they have been demanding for pension for their sustenance; and (d) if so, the details thereof and action taken so far to provide pension to them? ANSWER THE MINISTER OF STATE IN THE MINISTRY OF HEALTH AND FAMILY WELFARE (SHRI ASHWINI KUMAR CHOUBEY) (a) & (b): As per information received from Government of Telangana, the list of Dialysis Centres in Government Hospitals in the state is at Annexure. 2462 patients are undergoing dialysis treatment in the centres established in Government Hospitals. (c) & (d): Public Health is a State subject. The Central Government, however, supplements efforts of States/UTs through technical and financial support. Under Pradhan Mantri National Dialysis Programme (PMNDP). States/UTs are financially supported for providing dialysis services free of cost to the poor. There is no provision of pension under PMNDP. Govt. of Telangana has also informed that pension is not being given to those under dialysis.