Pembrolizumab in Combination with the Oncolytic Virus Pelareorep and Chemotherapy In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Oncolytic Viruses PANVAC and Pelareorep As Treatment for Metastatic Breast Cancer
Oncolytic Viruses PANVAC and Pelareorep as Treatment for Metastatic Breast Cancer Willie Mieke Iwema Rijksuniversiteit Groningen S2673622 BSc Thesis Life science & Technology July 5, 2019 Department of Medical Microbiology: Molecular Virology D. Bhatt PhD candidate Prof. dr. C.A.H.H. Daemen Table of content 1. Introduction ................................................................................................................................ 4 2. PANVAC ....................................................................................................................................... 7 2.1 Vaccinia virus mechanism of action .............................................................................................. 7 2.2 Activation of the host immune system .......................................................................................... 8 2.3 PANVAC in advanced carcinomas ................................................................................................. 9 2.4 PANVAC and docetaxel in metastatic breast cancer ................................................................... 11 3. Pelareorep ................................................................................................................................. 13 3.1 Reovirus mechanism of action .................................................................................................... 13 3.2 Activation of the host immune system ........................................................................................ 14 3.3 Pelareorep -

Pembrolizumab in Combination with the Oncolytic Virus Pelareorep And
Published OnlineFirst November 6, 2019; DOI: 10.1158/1078-0432.CCR-19-2078 CLINICAL CANCER RESEARCH | CLINICAL TRIALS: IMMUNOTHERAPY Pembrolizumab in Combination with the Oncolytic Virus Pelareorep and Chemotherapy in Patients with Advanced Pancreatic Adenocarcinoma: A Phase Ib Study A C Devalingam Mahalingam1,2, Grey A. Wilkinson3, Kevin H. Eng4, Paul Fields5, Patrick Raber5, Jennifer L. Moseley2, Karol Cheetham3, Matt Coffey3, Gerard Nuovo6, Pawel Kalinski4, Bin Zhang1, Sukeshi Patel Arora2, and Christos Fountzilas4 ABSTRACT ◥ Background: Pelareorep is an intravenously delivered oncolytic achieved partial response for 17.4 months. Two additional patients reovirus that can induce a T-cell–inflamed phenotype in pancreatic achieved stable disease, lasting 9 and 4 months, respectively. ductal adenocarcinoma (PDAC). Tumor tissues from patients Treatment was well tolerated, with mostly grade 1 or 2 treat- treated with pelareorep have shown reovirus replication, T-cell ment-related adverse events, including flu-like symptoms. Viral infiltration, and upregulation of PD-L1. We hypothesized that replication was observed in on-treatment tumor biopsies. T-cell pelareorep in combination with pembrolizumab and chemotherapy receptor sequencing from peripheral blood revealed the creation of in patients with PDAC would be safe and effective. new T-cell clones during treatment. High peripheral clonality and Methods: A phase Ib single-arm study enrolled patients with changes in the expression of immune genes were observed in PDAC who progressed after first-line treatment. Patients received patients with clinical benefit. pelareorep, pembrolizumab, and either 5-fluorouracil, gemcitabine, Conclusions: Pelareorep and pembrolizumab added to che- or irinotecan until disease progression or unacceptable toxicity. motherapy did not add significant toxicity and showed encour- Study objectives included safety and dose-limiting toxicities, tumor aging efficacy. -

Supplementary Table 1: Adhesion Genes Data Set
Supplementary Table 1: Adhesion genes data set PROBE Entrez Gene ID Celera Gene ID Gene_Symbol Gene_Name 160832 1 hCG201364.3 A1BG alpha-1-B glycoprotein 223658 1 hCG201364.3 A1BG alpha-1-B glycoprotein 212988 102 hCG40040.3 ADAM10 ADAM metallopeptidase domain 10 133411 4185 hCG28232.2 ADAM11 ADAM metallopeptidase domain 11 110695 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 195222 8038 hCG40937.4 ADAM12 ADAM metallopeptidase domain 12 (meltrin alpha) 165344 8751 hCG20021.3 ADAM15 ADAM metallopeptidase domain 15 (metargidin) 189065 6868 null ADAM17 ADAM metallopeptidase domain 17 (tumor necrosis factor, alpha, converting enzyme) 108119 8728 hCG15398.4 ADAM19 ADAM metallopeptidase domain 19 (meltrin beta) 117763 8748 hCG20675.3 ADAM20 ADAM metallopeptidase domain 20 126448 8747 hCG1785634.2 ADAM21 ADAM metallopeptidase domain 21 208981 8747 hCG1785634.2|hCG2042897 ADAM21 ADAM metallopeptidase domain 21 180903 53616 hCG17212.4 ADAM22 ADAM metallopeptidase domain 22 177272 8745 hCG1811623.1 ADAM23 ADAM metallopeptidase domain 23 102384 10863 hCG1818505.1 ADAM28 ADAM metallopeptidase domain 28 119968 11086 hCG1786734.2 ADAM29 ADAM metallopeptidase domain 29 205542 11085 hCG1997196.1 ADAM30 ADAM metallopeptidase domain 30 148417 80332 hCG39255.4 ADAM33 ADAM metallopeptidase domain 33 140492 8756 hCG1789002.2 ADAM7 ADAM metallopeptidase domain 7 122603 101 hCG1816947.1 ADAM8 ADAM metallopeptidase domain 8 183965 8754 hCG1996391 ADAM9 ADAM metallopeptidase domain 9 (meltrin gamma) 129974 27299 hCG15447.3 ADAMDEC1 ADAM-like, -

Cd1b Tetramers Bind T Cell Receptors to Identify a Mycobacterial
Published August 1, 2011 Brief Definitive Report CD1b tetramers bind T cell receptors to identify a mycobacterial glycolipid- reactive T cell repertoire in humans Anne G. Kasmar,1 Ildiko van Rhijn,1,2 Tan-Yun Cheng,1 Marie Turner,3 Chetan Seshadri,1 Andre Schiefner,4 Ravi C. Kalathur,4 John W. Annand,1 Annemieke de Jong,1 John Shires,5 Luis Leon,1 Michael Brenner,1 Ian A. Wilson,4 John D. Altman,5 and D. Branch Moody1 1Division of Rheumatology, Immunology and Allergy, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA 02115 2Department of Infectious Diseases and Immunology, Faculty of Veterinary Medicine, Utrecht University, 3508 TD Utrecht, Netherlands 3Tuberculosis Treatment Unit, Lemuel Shattuck Hospital, Jamaica Plain, MA 02130 4Department of Molecular Biology and Skaggs Institute for Chemical Biology, the Scripps Research Institute, La Jolla, CA 92037 Downloaded from 5Emory Vaccine Center, Atlanta, GA 30329 Microbial lipids activate T cells by binding directly to CD1 and T cell receptors (TCRs) or by indirect effects on antigen-presenting cells involving induction of lipid autoantigens, CD1 transcription, or cytokine release. To distinguish among direct and indirect mechanisms, we developed fluorescent human CD1b tetramers and measured T cell staining. CD1b tetramer staining of T cells requires glucose monomycolate (GMM) antigens, is specific for TCR jem.rupress.org structure, and is blocked by a recombinant clonotypic TCR comprised of TRAV17 and TRBV4-1, proving that CD1b–glycolipid complexes bind the TCR. GMM-loaded tetramers brightly stain a small subpopulation of blood-derived cells from humans infected with Mycobacterium tuberculosis, providing direct detection of a CD1b-reactive T cell reper- toire. -
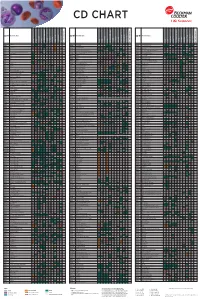
Flow Reagents Single Color Antibodies CD Chart
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n -

Immunotherapy in Myeloma Horizons Infosheet Clinical Trials and Novel Drugs
Immunotherapy in myeloma Horizons Infosheet Clinical trials and novel drugs This Horizons Infosheet provides information on immunotherapy, a type of treatment being investigated in myeloma. The Horizons Infosheet series What is immunotherapy? provides information relating Immunotherapy is a type of cancer to novel drugs and treatment treatment which helps the immune strategies that are currently being system to recognise and kill cancer investigated for the treatment of cells. Many myeloma treatments are myeloma. The series also aims to immunotherapies. highlight the considerable amount of research currently taking place in What is the immune system? the field of myeloma. The immune system is made up of The drugs and novel strategies specialised cells, tissues and organs described in the Horizons Infosheets which work together in a process may not be licensed and/or known as an immune response. An approved for use in myeloma. You immune response protects the body may, however, be able to access from foreign organisms (such as them as part of a clinical trial. bacteria or viruses) that enter the body. Infoline: 0800 980 3332 1 The immune system also identifies of mechanisms, allowing them and kills faulty or abnormal cells in to multiply and grow in the body. the body. Immunotherapy stimulates the immune system to work harder or White blood cells, produced in the smarter to kill myeloma cells. bone marrow, are an important part of the immune system. Different The complexity of the immune types of white blood cell, such as system means that there are plasma cells and T cells, perform many ways in which it can be specific immune functions. -

Targeting EZH2 Increases Therapeutic Efficacy of PD-1 Check-Point Blockade in Models of Prostate Cancer Supplement Figures and T
Targeting EZH2 Increases Therapeutic Efficacy of PD-1 Check-Point Blockade in Models of Prostate Cancer Supplement Figures and Tables 1 Fig. S1. (A) Schema and genotyping PCR example for the creation of EM and EMC genetically engineered mice. (B) Three-dimensional PCa organoids generated from EM mice (without PSACreERT2) alleles. When treated with tamoxifen, demonstrates no loss of H3K27me3 or EDU staining, indicating specificity of tamoxifen-PSACreERT2 mediated deletion of the Ezh2 set domain. (C) Principle component analysis (PCA) following chemical and genetic inhibition of Ezh2 catalytic function results in significant changes in gene expression. 2 Fig. S2. (A) A 29-gene signature derived from Fig. 1C demonstrates complete independence from a previously published polycomb repression signature. (B) Our 29 gene signature demonstrates significant correlation with a previously published polycomb repression signature in 2 independent human PCa gene expression datasets. (C) EZH2 activity is not determined by EZH2 mRNA expression. 3 Fig. S3. A 29-gene signature derived from Fig 1C was used to generate signature scores for each patient within four independent human prostate cancer RNA-seq datasets. Patients were ranked highest score to lowest score and subject to quartile separation. First (blue) and fourth (red) quartiles were analyzed by supervised clustering to demonstrate expression differences within patients with most lowest EZH2 activity and most highest EZH2 activity. 4 Fig. S4. Genes representing IFN signaling (STAT1, IRF9), Th1 chemokines (CXCL10, CXCL11), and MHC Class I molecules (B2M, HLA-A) were shown to be enriched in PCa patients with low EZH2 activity. 5 Fig. S5. Treatment of 22Rv1 human 2D cell lines with the demonstrated conditions for 96 hours show that EZH2 inhibition increases expression of dsRNA (green = dsRNA, blue = nuclei). -

Supplementary Table 1: Differentially Methylated Genes and Functions of the Genes Before/After Treatment with A) Doxorubicin and B) FUMI and in C) Responders Vs
Supplementary Table 1: Differentially methylated genes and functions of the genes before/after treatment with a) doxorubicin and b) FUMI and in c) responders vs. non- responders for doxorubicin and d) FUMI Differentially methylated genes before/after treatment a. Doxo GENE FUNCTION CCL5, CCL8, CCL15, CCL21, CCR1, CD33, IL5, immunoregulatory and inflammatory processes IL8, IL24, IL26, TNFSF11 CCNA1, CCND2, CDKN2A cell cycle regulators ESR1, FGF2, FGF14, FGF18 growth factors WT1, RASSF5, RASSF6 tumor suppressor b. FUMI GENE FUNCTION CCL7, CCL15, CD28, CD33, CD40, CD69, TNFSF18 immunoregulatory and inflammatory processes CCND2, CDKN2A cell cycle regulators IGF2BP1, IGFBP3 growth factors HOXB4, HOXB6, HOXC8 regulation of cell transcription WT1, RASSF6 tumor suppressor Differentially methylated genes in responders vs. non-responders c. Doxo GENE FUNCTION CBR1, CCL4, CCL8, CCR1, CCR7, CD1A, CD1B, immunoregulatory and inflammatory processes CD1D, CD1E, CD33, CD40, IL5, IL8, IL20, IL22, TLR4 CCNA1, CCND2, CDKN2A cell cycle regulators ESR2, ERBB3, FGF11, FGF12, FGF14, FGF17 growth factors WNT4, WNT16, WNT10A implicated in oncogenesis TNFSF12, TNFSF15 apoptosis FOXL1, FOXL2, FOSL1,HOXA2, HOXA7, HOXA11, HOXA13, HOXB4, HOXB6, HOXB8, HOXB9, HOXC8, regulation of cell transcription HOXD8, HOXD9, HOXD11 GSTP1, MGMT DNA repair APC, WT1 tumor suppressor d. FUMI GENE FUNCTION CCL1, CCL3, CCL5,CCL14, CD1B, CD33, CD40, CD69, immunoregulatory and inflammatory IL20, IL32 processes CCNA1, CCND2, CDKN2A cell cycle regulators IGF2BP1, IGFBP3, IGFBP7, EGFR, ESR2,RARB2 -

Current Trends in Cancer Immunotherapy
biomedicines Review Current Trends in Cancer Immunotherapy Ivan Y. Filin 1 , Valeriya V. Solovyeva 1 , Kristina V. Kitaeva 1, Catrin S. Rutland 2 and Albert A. Rizvanov 1,3,* 1 Institute of Fundamental Medicine and Biology, Kazan Federal University, 420008 Kazan, Russia; [email protected] (I.Y.F.); [email protected] (V.V.S.); [email protected] (K.V.K.) 2 Faculty of Medicine and Health Science, University of Nottingham, Nottingham NG7 2QL, UK; [email protected] 3 Republic Clinical Hospital, 420064 Kazan, Russia * Correspondence: [email protected]; Tel.: +7-905-316-7599 Received: 9 November 2020; Accepted: 16 December 2020; Published: 17 December 2020 Abstract: The search for an effective drug to treat oncological diseases, which have become the main scourge of mankind, has generated a lot of methods for studying this affliction. It has also become a serious challenge for scientists and clinicians who have needed to invent new ways of overcoming the problems encountered during treatments, and have also made important discoveries pertaining to fundamental issues relating to the emergence and development of malignant neoplasms. Understanding the basics of the human immune system interactions with tumor cells has enabled new cancer immunotherapy strategies. The initial successes observed in immunotherapy led to new methods of treating cancer and attracted the attention of the scientific and clinical communities due to the prospects of these methods. Nevertheless, there are still many problems that prevent immunotherapy from calling itself an effective drug in the fight against malignant neoplasms. This review examines the current state of affairs for each immunotherapy method, the effectiveness of the strategies under study, as well as possible ways to overcome the problems that have arisen and increase their therapeutic potentials. -

Discovery of Deoxyceramides and Diacylglycerols As Cd1b Scaffold Lipids Among Diverse Groove-Blocking Lipids of the Human CD1 System
Discovery of deoxyceramides and diacylglycerols as CD1b scaffold lipids among diverse groove-blocking lipids of the human CD1 system Shouxiong Huanga, Tan-Yun Chenga, David C. Younga, Emilie Layrea, Cressida A. Madigana, John Shiresb, Vincenzo Cerundoloc, John D. Altmanb, and D. Branch Moodya,1 aDepartment of Medicine, Division of Rheumatology, Immunology and Allergy, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA 02115; bEmory Vaccine Center, Emory School of Medicine, Atlanta, GA 30322; and cMedical Research Council Human Immunology Unit, Weatherall Institute of Molecular Medicine, University of Oxford, Oxford OX3 9DS, United Kingdom Edited* by Peter Cresswell, Yale University School of Medicine, New Haven, CT, and approved October 17, 2011 (received for review August 10, 2011) Unlike the dominant role of one class II invariant chain peptide (CLIP) environment (7, 8). The differing pH requirements for antigen in blocking MHC class II, comparative lipidomics analysis shows that loading, combined with enrichment of endogenous lipids in the human cluster of differentiation (CD) proteins CD1a, CD1b, CD1c, secretory pathway and exogenous lipids endosomes, are coalescing and CD1d bind lipids corresponding to hundreds of diverse accurate into a two-step model of lipid antigen presentation. First, newly mass retention time values. Although most ions were observed in translated CD1 proteins, aided by the microsomal triglyceride association with several CD1 proteins, ligands binding selectively to transport protein (MTP) (9), -

Mechanisms and Consequences of Antigen Presentation By
Series: The Biology of Antigen Presentation Feature Review Mechanisms and Consequences of Antigen Presentation by CD1 1, 1 1,2 Luc Van Kaer, * Lan Wu, and Sebastian Joyce The CD1 proteins are a family of non-polymorphic and MHC class I-related Trends molecules that present lipid antigens to subsets of T lymphocytes with innate- or The CD1–lipid presentation system adaptive-like immune functions. Recent studies have provided new insight into allows the immune system to sense alterations in lipid homeostasis, and the identity of immunogenic CD1 antigens and the mechanisms that control the complements the classical MHC–pep- generation and loading of these antigens onto CD1 molecules. Furthermore, tide presentation system. There are substantial progress has been made in identifying CD1-restricted T cells and remarkable similarities and surprising differences in the way that TCRs decoding the diverse immunological functions of distinct CD1-restricted T cell engage CD1–lipid versus MHC–pep- subsets. These findings shed new light on the contributions of the CD1 antigen- tide complexes. presentation pathway to normal health and to a diverse array of pathologies, and Group 1 CD1 proteins (CD1a–c) pre- provide a new impetus for exploiting this fascinating recognition system for the sent a variety of endogenous, myco- development of vaccines and immunotherapies. bacterial, and potentially other bacterial lipids to T cells. CD1b-restricted T cells include subsets expressing germline- Antigen-Presentation Systems encoded TCRs. Products encoded by the major histocompatibility complex (MHC) region of the vertebrate Group 2 CD1 proteins (CD1d) present genome bind peptide fragments from pathogens and display them at the surface of antigen- diverse endogenous and exogenous presenting cells (APCs) for appraisal by T lymphocytes [1].