Bob Bethell Joint Committee on Home and Community Based Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Journal of the House
4 JOURNAL OF THE HOUSE Journal of the House FIRST DAY HALL OF THE HOUSE OF REPRESENTATIVES, TOPEKA, KS, Monday, January 11, 2021, 2:00 p.m. This being the day fixed by the Constitution of the State of Kansas for the assembling of the 2021 session of the legislature, the House of Representatives was called to order at 2:00 p.m. by Catherine Gunsalus, Assistant Secretary of State. Assistant Secretary of State Catherine Gunsalus announced the appointment of Susan Kannarr as temporary Chief Clerk of the House. State of Kansas Office of Secretary of State I, CATHERINE GUNSALUS, Assistant Secretary of State, do hereby certify that the following persons were elected members of the House of Representatives of the State of Kansas for a two-year term beginning on the second Monday of January, A.D. 2021. IN TESTIMONY WHEREOF, I hereto set my hand and cause to be affixed my official seal. Done at the city of Topeka, this 30th day of November, A.D. 2020. CATHERINE GUNSALUS Assistant Secretary of State Members of the House of Representatives were then called in groups, came forward, took and subscribed, or affirmed, to their respective oaths of office, administered to them by Chief Justice Marla Luckert, Kansas Supreme Court as follows: State of Kansas, County of Shawnee, ss: We and each of us, do solemnly swear or affirm, that we will support the Constitution of the United States and the Constitution of the State of Kansas, and faithfully discharge the duties of the office of Representative of the State of Kansas, so help me God. -

Report of the Robert G. (Bob) Bethell Joint Committee on Home and Community Based Services and Kancare Oversight to the 2021 Kansas Legislature
JOINT COMMITTEE Report of the Robert G. (Bob) Bethell Joint Committee on Home and Community Based Services and KanCare Oversight to the 2021 Kansas Legislature CHAIRPERSON: Representative Brenda Landwehr VICE-CHAIRPERSON: Senator Gene Suellentrop OTHER MEMBERS: Senators Ed Berger, Bud Estes, Richard Hilderbrand, and Pat Pettey; Representatives Barbara Ballard, John Barker, Will Carpenter, Susan Concannon, and Monica Murnan CHARGE ● KSA 2020 Supp. 39-7,160 directs the Committee to oversee long-term care services, including home and community based services (HCBS). The Committee is to oversee the savings resulting from the transfer of individuals from state or private institutions to HCBS and to ensure that any proceeds resulting from the successful transfer be applied to the system for the provision of services for long-term care. Further, the Committee is to oversee the Children’s Health Insurance Program (CHIP), the Program for All-Inclusive Care for the Elderly (PACE), and the state Medicaid program (KanCare), and monitor and study the implementation and operations of these programs including, but not limited to, access to and quality of services provided and any financial information and budgetary issues. February 2021 Robert G. (Bob) Bethell Joint Committee on Home and Community Based Services and KanCare Oversight ANNUAL REPORT Conclusions and Recommendations The Robert G. (Bob) Bethell Joint Committee on Home and Community Based Services and KanCare Oversight recommends: ● The House Committee on Health and Human Services and the -
Robert G. (Bob) Bethell Joint Committee on Home and Community Based Services and Kancare Oversight
For additional information contact: Kari M. Bruffett Kansas Health Institute 212 SW Eighth Avenue, Suite 300 Topeka, Kansas 66603-3936 Tel. 785.233.5443 Email: [email protected] Website: www.khi.org Robert G. (Bob) Bethell Joint Committee on Home and Community Based Services and KanCare Oversight December 15, 2020 Integrated Care Kari M. Bruffett Vice President for Policy Kansas Health Institute Informing Policy. Improving Health. The Kansas Health Institute supports effective policymaking through nonpartisan research, education and engagement. KHI believes evidence-based information, objective analysis and civil dialogue enable policy leaders to be champions for a healthier Kansas. Established in 1995 with a multiyear grant from the Kansas Health Foundation, KHI is a nonprofit, nonpartisan educational organization based in Topeka. 1 ǀ Page Chair Landwehr and Members of the Committee: Thank you for the opportunity to introduce a discussion of the integration of primary medical and behavioral health care. My name is Kari Bruffett, and I am vice president for policy at the Kansas Health Institute (KHI). KHI is a nonprofit, nonpartisan educational organization based in Topeka, founded in 1995 with a multiyear grant from the Kansas Health Foundation. KHI had the honor to help facilitate the working groups for the Special Committee on Mental Health Modernization and Reform. I would like to draw your attention to a list of the membership of the System Capacity and Transformation Working Group, which developed a recommendation I’ll describe shortly. The Special Committee, as many of you know, was tasked with analyzing the state’s behavioral health system and developing a strategic effort to modernize the system. -

Districts & Incumbents
Plan: District Court - House Plan Type: House Administrator KLRD User: KLRD Districts & Their Incumbents Wednesday, June 6, 2012 5:42 PM District Name Party Previous District 001 Doug Gatewood Democrat 1 002 Jerry D. Williams Democrat 8 002 Robert Grant Democrat 2 003 Terry Calloway Republican 3 004 005 Bill Feuerborn Democrat 5 005 Caryn Tyson Republican 4 006 Jene Vickrey Republican 6 007 Richard Proehl Republican 7 008 Sheryl Spalding Republican 29 009 010 Terri Lois Gregory Republican 10 010 Anthony Brown Republican 38 011 James Kelly Republican 12 012 Virgil Peck Jr. Republican 11 013 Forrest Knox Republican 13 014 015 016 Amanda Grosserode Republican 16 017 018 John Rubin Republican 18 019 Kay Wolf Republican 21 020 Rob Bruchman Republican 20 020 Pat Colloton Republican 28 021 Barbara Bollier Republican 25 022 Gregory Smith Republican 22 Page 1 Plan: District Court - House Administrator: KLRD Type: House User: KLRD District Name Party Previous District 023 Kelly Meigs Republican 17 024 Brett Hildabrand Republican 23 025 Mike Slattery Democrat 24 026 027 Charlotte O'Hara Republican 27 028 029 Jim Denning Republican 19 030 Lance Kinzer Republican 14 030 Ron Worley Republican 30 031 Louis Ruiz Democrat 32 032 Michael Peterson Democrat 37 033 Tom Burroughs Democrat 33 034 Valdenia Winn Democrat 34 035 Broderick Henderson Democrat 35 036 Kathy Wolfe Moore Democrat 36 037 Stan Frownfelter Democrat 31 038 039 Owen Donohoe Republican 39 040 041 Jana Taylor Goodman Republican 41 042 Melanie Meier Democrat 40 042 Connie O'Brien Republican 42 043 044 Barbara Ballard Democrat 44 045 Tom Sloan Republican 45 046 Paul Davis Democrat 46 047 Ramon Gonzalez Jr. -

2004 Primary Election Results
Kansas Secretary of State Page 1 2004 Primary Election Official Vote Totals Race Candidate Votes Percent United States Senate D-Robert A. Conroy 61,052 55.9 % D-Lee Jones 48,133 44.0 % R-Samuel D. Brownback 286,839 86.9 % R-Arch Naramore 42,880 13.0 % United States House of Representatives 001 R-Jerry Moran 94,098 100.0 % United States House of Representatives 002 D-Nancy Boyda 36,771 100.0 % R-Jim Ryun 69,368 100.0 % United States House of Representatives 003 D-Dennis Moore 33,466 100.0 % R-Kris Kobach 39,129 44.0 % R-Patricia Lightner 10,836 12.1 % R-Adam Taff 38,922 43.7 % United States House of Representatives 004 D-Michael Kinard 14,308 73.0 % D-Marty Mork 5,279 26.9 % R-Todd Tiahrt 53,202 100.0 % Kansas Senate 001 D-Tom Kautz 2,007 58.8 % D-Galen Weiland 1,401 41.1 % R-Richard S. Karnowski 937 8.0 % R-Trent LeDoux 2,683 23.0 % R-Steve Lukert 3,381 29.0 % R-Dennis D. Pyle 4,642 39.8 % Kansas Senate 002 D-Marci Francisco 2,999 100.0 % R-Mark Buhler 3,221 63.0 % R-Don Johnson 1,889 36.9 % Kansas Senate 003 D-Jan Justice 3,036 71.5 % D-Edward (Ed) Sass 1,207 28.4 % R-Connie O'Brien 2,673 33.6 % R-Roger C. Pine 3,760 47.2 % R-Chuck Quinn 586 7.3 % R-Richard Rodewald 933 11.7 % Kansas Senate 004 D-David Haley 5,140 100.0 % Kansas Senate 005 D-Mark S. -

Interim Committee Memberships
Kansas Legislative Research Department November 29, 2018 2018 INTERIM COMMITTEE MEMBERSHIPS Special Committees Commerce Federal and State Affairs Statutory Joint Committees Administrative Rules and Regulations Corrections and Juvenile Justice Oversight Home and Community Based Services & KanCare Oversight, Robert G. (Bob) Bethell Information Technology Kansas Security Legislative Budget Pensions, Investments and Benefits Special Claims Against the State State Building Construction State-Tribal Relations Other Capitol Preservation Committee Health Care Stabilization Fund Oversight Committee Senate Confirmation Oversight Child Welfare System Task Force Joint Legislative Transportation Vision Task Force Legislative Task Force on Dyslexia Statewide Broadband Expansion Planning Task Force Kansas Legislative Research Department 2 ICML – November 29, 2018 SPECIAL COMMITTEES Commerce Federal and State Affairs Kansas Legislative Research Department 3 ICML – November 29, 2018 Kansas Legislative Research Department 4 ICML – November 29, 2018 SPECIAL COMMITTEE ON COMMERCE* Senate House Kansas Legislative Research Department Office of Revisor of Statutes Reed Holwegner Chuck Reimer Edward Penner Kyle Hamilton Chris Courtwright Dylan Dear STUDY TOPICS The Committee is directed to: ● Consider investment analyses to be performed on economic development projects that receive state support; ● Review the substance of those bills introduced during the 2018 Legislative Session pertaining to the evaluation and transparency of economic development programs and, if applicable, introduce new legislation that forges together the best elements of those proposals; and ● Develop criteria that standing committees of the House and Senate may use when approving the creation of new programs or incentives that meet the future needs of the Kansas economy. Approved Meeting Days: 1 day * To date, the LCC has not designated a Committee chairperson (House or Senate), nor designated this Committee’s size. -
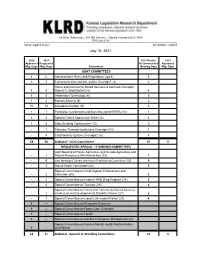
Item No. 2 Request Interim Days and Letters
68-West–Statehouse | 300 SW 10th Ave. | Topeka, Kansas 66612-1504 (785) 296-3181 [email protected] kslegislature.org/klrd July 15, 2021 2020 2021 2021 Prelim. 2021 Approved Requested Recommended Approved Mtg. Days Mtg. Days Committees Meeting Days Mtg. Days JOINT COMMITTEES 4 6 Administrative Rules and Regulations ( pg 1) 6 3 3 Corrections and Juvenile Justice Oversight1 (2) 3 Home and Community Based Services & KanCare Oversight, 4 4 Robert G. (Bob) Bethell (4) 4 5 6 Information Technology (6) 5 1 2 Kansas Security (8) 2 10 10 Legislative Budget (9) 6 1 1 Pensions, Investments and Benefits (Joint KPERS)(10) 1 3 4 Special Claims Against the State (12) 4 3 5 State Building Construction2 (13) 5 -- 1 Fiduciary Financial Institutions Oversight (14) 1 -- 4 Child Welfare System Oversight (16) 4 34 46 Subtotal—Joint Committees 41 0 REQUESTED SPECIAL / STANDING COMMITTEES Joint Meeting of House Agriculture and Senate Agriculture and -- 1 Natural Resources (Pet Animal Act) (18) 1 -- 9 Joint Meeting of Senate and House Redistricting Committees2 (20 9 -- 3 House Water Committee2 (22) 3 Special Committee on Child Support Enforcement and -- 2 Collection (24) 2 -- 2 Special Committee on Federal 340B Drug Program (24) 2 -- 4 Special Committee on Taxation (26) 2 Special Committee on Home and Community Based Services -- 2 Intellectual and Developmental Disability Waiver (27) 2 -- 4 Special Committee on Liquor Law modernization (29) 4 6 -- Special Committee on Economic Recovery 6 -- Special Committee on Foster Care Oversight 0 -- Special Committee on Health 6 -- Special Committee on Kansas Emergency Management Act Special Committee on Kansas Mental Health Modernization 6 -- and Reform 24 27 Subtotal—Special or Standing Committees 25 0 2020 2021 2021 Prelim. -

Legislative Directory
State of Kansas Legislative Directory 83rd Legislature 2009 Regular Session Published by Ron Thornburgh, Secretary of State 2009 Legislative Directory Table of Contents United States Senators ....................................................................................................... 1 United States Representatives ............................................................................................ 2 Kansas State Officers.......................................................................................................... 4 State Board of Education .................................................................................................... 6 Legislative telephone numbers and Web sites ................................................................... 8 Kansas Senate By district .................................................................................................................... 9 Officers and standing committees ............................................................................. 11 Capitol office addresses and phone numbers ............................................................ 12 Home/business contact information .......................................................................... 14 Kansas House of Representatives By district .................................................................................................................. 24 Officers and standing committees ............................................................................. 31 Capitol office -

Official Primary Election Results
Kansas Secretary of State Page 1 2010 Primary Election Official Vote Totals Race Candidate Votes Percent United States Senate D-Robert A. Conroy 7,857 9.5 % D-David Haley 15,731 19.1 % D-Lisa Johnston 25,695 31.2 % D-Charles Schollenberger 19,426 23.6 % D-Patrick Wiesner 13,481 16.4 % R-Tom Little 10,256 3.1 % R-Robert (Bob) Londerholm 8,278 2.5 % R-Jerry Moran 163,483 49.7 % R-Todd Tiahrt 146,702 44.6 % United States House of Representatives 001 D-Alan Jilka 15,399 100.0 % R-Jim Barnett 25,047 25.0 % R-Sue (Holloway) Boldra 7,892 7.8 % R-Marck Cobb 1,768 1.7 % R-Tim Huelskamp 34,819 34.8 % R-Tracey Mann 21,161 21.1 % R-Rob Wasinger 9,296 9.2 % United States House of Representatives 002 D-Cheryl Hudspeth 10,030 44.1 % D-Thomas Koch 8,086 35.6 % D-Sean Tevis 4,579 20.1 % R-Lynn Jenkins 41,458 57.1 % R-Dennis Pyle 31,085 42.8 % United States House of Representatives 003 D-Stephene Moore 16,756 78.0 % D-Thomas Scherer 4,709 21.9 % R-Dan Gilyeat 2,581 3.5 % R-Dave King 820 1.1 % R-Garry R. Klotz 1,873 2.5 % R-Patricia Lightner 26,695 36.8 % R-Jerry M. Malone 2,099 2.8 % R-Craig McPherson 2,664 3.6 % R-John Timothy Rysavy (Rez) 1,633 2.2 % R-Jean Ann Uvodich 1,934 2.6 % R-Kevin Yoder 32,210 44.4 % United States House of Representatives 004 D-Raj Goyle 17,146 79.7 % D-Robert Tillman 4,358 20.2 % R-Jim Anderson 10,294 12.7 % R-Wink Hartman 18,365 22.8 % R-Mike Pompeo 31,180 38.7 % R-Paij Rutschman 1,596 1.9 % R-Jean Kurtis Schodorf 19,099 23.7 % Kansas Secretary of State Page 2 2010 Primary Election Official Vote Totals Race Candidate Votes Percent Governor / Lt. -

Candidates for the 2010 General (Official) Candidate Office District Position Division Party Title First Name Middle Last Name S
Candidates for the 2010 General (official) Candidate Office District Position Division Party Title First Name Middle Last Name Suffix Ballot City Running Mate Ballot City Lisa Johnston United States Senate 0 0 0 Democratic Ms. Lisa Johnston Overland Park Jerry Moran United States Senate 0 0 0 Republican Mr. Jerry Moran Hays Michael Wm. Dann United States Senate 0 0 0 Libertarian Mr. Michael Wm. Dann Baldwin City Joseph (Joe) K. Bellis United States Senate 0 0 0 Reform Mr. Joseph (Joe) K. Bellis Overland Park Alan Jilka United States House of Representatives 1 0 0 Democratic Mr. Alan Jilka Salina Tim Huelskamp United States House of Representatives 1 0 0 Republican Mr. Tim Huelskamp Fowler Jack Warner United States House of Representatives 1 0 0 Libertarian Mr. Jack Warner Wright Cheryl Hudspeth United States House of Representatives 2 0 0 Democratic Ms. Cheryl Hudspeth Girard Lynn Jenkins United States House of Representatives 2 0 0 Republican Ms. Lynn Jenkins Topeka Robert Garrard United States House of Representatives 2 0 0 Libertarian Mr. Robert Garrard Edgerton Stephene Moore United States House of Representatives 3 0 0 Democratic Mrs. Stephene Moore Lenexa Kevin Yoder United States House of Representatives 3 0 0 Republican Mr. Kevin Yoder Overland Park Jasmin Talbert United States House of Representatives 3 0 0 Libertarian Ms. Jasmin Talbert Kansas City Raj Goyle United States House of Representatives 4 0 0 Democratic Mr. Raj Goyle Wichita Mike Pompeo United States House of Representatives 4 0 0 Republican Mr. Mike Pompeo Wichita Shawn Smith United States House of Representatives 4 0 0 Libertarian Mr. -

Medical Marijuana—Will Likely Resurface, All Will Be in the Form of New Bills
GREEN SHEET DRAFT: January 4, 2017 12:22 PM KHI.ORG Informing Policy. Improving Health. 2017 KANSAS LEGISLATIVE PREVIEW Anticipating key health policy themes Introduction Democrats. Forty-six of the representatives are new for 2017, but six of them have previously served The 2017 legislative session will mark the in the House. (These numbers include the recent first year of a two-year cycle. While issues announcement of Rep. Marvin Kleeb’s retirement on from previous sessions—such as the status Jan. 10 and the election of his successor, Abraham of the state’s psychiatric hospitals, Medicaid Rafie.) ISSUE BRIEF expansion and medical marijuana—will likely resurface, all will be in the form of new bills. KanCare Dozens of new faces in the Capitol also mean the Legislature itself will have a new During the 2017 session, legislators will have the character. opportunity to debate and respond to a number of issues related to the current and future operation of As a result of the general election in the Kansas Medicaid program, known as KanCare. November 2016, the Kansas Senate has gone from 32 Republicans and eight Democrats to 31 Republicans and nine KanCare 2.0 Democrats. Fourteen of the senators Although the initial three-year term of state contracts are new, although five of them were in for the three KanCare managed care organizations the Kansas House in 2016. The Kansas (MCOs) ended December 31, 2015, the MCOs have House went from 97 Republicans and continued to operate under an optional two-year 28 Democrats to 85 Republicans and 40 extension of the original term of their contracts. -

Legislative Directory 84Th Kansas Legislature 2011 Regular Session
Legislative Directory 84th Kansas Legislature 2011 Regular Session Published by Kris W. Kobach Secretary of State 2011 Legislative Directory Table of Contents United States Senators ....................................................................................................... 1 United States Representatives ............................................................................................ 2 Kansas State Officers.......................................................................................................... 4 State Board of Education .................................................................................................... 6 Legislative telephone numbers and Web sites ................................................................... 8 Kansas Senate By district .................................................................................................................... 9 Officers and standing committees ............................................................................. 11 Capitol office addresses and phone numbers ............................................................ 12 Home/business contact information .......................................................................... 14 Kansas House of Representatives By district .................................................................................................................. 24 Officers and standing committees ............................................................................. 31 Capitol office addresses