Mechanisms of Mixed Chimerism-Based Transplant Tolerance
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Strokovno Poročilo UKCL 2019
STROKOVNO POROČILO 2019 STROKOVNO POROČILO 2019 Univerzitetni klinični center Ljubljana, Zaloška cesta 2, 1000 Ljubljana Odgovorna oseba: prof. dr. Jadranka Buturović Ponikar, dr. med., strokovna direktorica UKC Ljubljana Besedila za poročilo so prispevali: prof. dr. Zlatko Fras, mag. Jana Brguljan Hitij, prof. dr. Aleš Blinc, prof. dr. Matjaž Šinkovec, prof. dr. Marko Noč, prof. dr. Marjeta Terčelj, prof. dr. Borut Štabuc, prof. dr. Miha Arnol, doc. dr. Andrej Janež, prof. dr. Samo Zver, prof. dr. Matija Tomšič, Gregor Veninšek, doc. dr. Miran Brvar, dr. Hugon Možina, prof. dr. Matjaž Veselko, dr. Nikola Lakić, prof. dr. Roman Bošnjak, prof. dr. Uroš Ahčan, prof. dr. Matej Cimerman, prof. dr. Aleš Tomažič, dr. Tomaž Štupnik, asist. Bojan Štrus, prof. dr. Andrej Kansky, prof. dr. Vesna Novak Jankovič, doc. dr. Igor Frangež, prof. dr. Simon Podnar, prof. dr. Uroš Rot, doc., prof. dr. Adolf Lukanovič, doc. dr. Borut Kobal, Mag. Gorazd Kavšek, prof. dr. Eda Vrtačnik Bokal, Leon Meglič, prof. dr. Borut Peterlin, doc.dr. Marko Pokorn, doc. dr. Anamarija Meglič, prim. Mojca Brecelj Kobe, prof. dr.Tadej Avčin, Uroš Krivec, prof. dr. Rok Orel, prof. dr. Tadej Battellino, prof. dr. Tanja Kersnik Levart, prof. dr. Janez Jazbec, prof. dr. Darja Paro Panjan, prof. dr. David Neubauer, mag. Mojca Tomažič, asist. dr. Veronika Velenšek, prof. dr. Milan Petelin, prof. dr. Martina Drevenšek, dr. Rok Kosem, doc.dr. Milan Kuhar, doc. dr. Tatjana Lejko Zupanc, prof. dr. Mojca Globočnik Petrović, prof. dr. Vane Antolič, doc. dr. Aleksandar Aničin, prim. asist. Tanja Planinšek Ručigaj, doc.dr.. Dimitrij Kuhelj, doc. dr. Katja Zaletel, prof. dr. Milan Skitek, prof. -

Newsletteralumni News of the Newyork-Presbyterian Hospital/Columbia University Department of Surgery Volume 13, Number 1 Summer 2010
NEWSLETTERAlumni News of the NewYork-Presbyterian Hospital/Columbia University Department of Surgery Volume 13, Number 1 Summer 2010 CUMC 2007-2009 Transplant Activity Profile* Activity Kidney Liver Heart Lung Pancreas Baseline list at year start 694 274 174 136 24 Deceased donor transplant 123 124 93 57 11 Living donor transplant 138 17 — 0 — Transplant rate from list 33% 50% 51% 57% 35% Mortality rate while on list 9% 9% 9% 15% 0% New listings 411 217 144 68 23 Wait list at year finish 735 305 204 53 36 2007-June 2008 Percent 1-Year Survival No % No % No % No % No % Adult grafts 610 91 279 86 169 84 123 89 6 100 Adult patients 517 96 262 88 159 84 116 91 5 100 Pediatric grafts 13 100 38 86 51 91 3 100 0 — Pediatric patients 11 100 34 97 47 90 2 100 0 — Summary Data Total 2009 living donor transplants 155 (89% Kidney) Total 2009 deceased donor transplants 408 (30% Kidney, 30% Liver) 2007-June 2008 adult 1-year patient survival range 84% Heart to 100% Pancreas 2007-June 2008 pediatric 1-year patient survival range 90% Heart to 100% Kidney or lung *Health Resource and Service Administration’s Scientific Registry of Transplant Recipients (SRTR) Ed Note. The figure shows the US waiting list for whole organs which will only be partially fulfilled by some 8,000 deceased donors, along with 6,600 living donors, who will provide 28,000 to 29,000 organs in 2010. The Medical Center’s role in this process is summarized in the table, and the articles that follow my note expand on this incredible short fall and its potential solutions. -
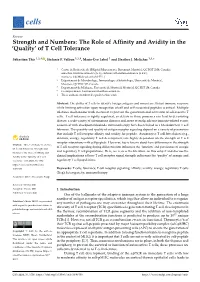
Of T Cell Tolerance
cells Review Strength and Numbers: The Role of Affinity and Avidity in the ‘Quality’ of T Cell Tolerance Sébastien This 1,2,† , Stefanie F. Valbon 1,2,†, Marie-Ève Lebel 1 and Heather J. Melichar 1,3,* 1 Centre de Recherche de l’Hôpital Maisonneuve-Rosemont, Montréal, QC H1T 2M4, Canada; [email protected] (S.T.); [email protected] (S.F.V.); [email protected] (M.-È.L.) 2 Département de Microbiologie, Immunologie et Infectiologie, Université de Montréal, Montréal, QC H3C 3J7, Canada 3 Département de Médecine, Université de Montréal, Montréal, QC H3T 1J4, Canada * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: The ability of T cells to identify foreign antigens and mount an efficient immune response while limiting activation upon recognition of self and self-associated peptides is critical. Multiple tolerance mechanisms work in concert to prevent the generation and activation of self-reactive T cells. T cell tolerance is tightly regulated, as defects in these processes can lead to devastating disease; a wide variety of autoimmune diseases and, more recently, adverse immune-related events associated with checkpoint blockade immunotherapy have been linked to a breakdown in T cell tolerance. The quantity and quality of antigen receptor signaling depend on a variety of parameters that include T cell receptor affinity and avidity for peptide. Autoreactive T cell fate choices (e.g., deletion, anergy, regulatory T cell development) are highly dependent on the strength of T cell receptor interactions with self-peptide. However, less is known about how differences in the strength Citation: This, S.; Valbon, S.F.; Lebel, of T cell receptor signaling during differentiation influences the ‘function’ and persistence of anergic M.-È.; Melichar, H.J. -

Prenatal Allospecific NK Cell Tolerance Hinges on Instructive
Prenatal Allospecific NK Cell Tolerance Hinges on Instructive Allorecognition through the Activating Receptor during Development This information is current as of September 23, 2021. Amir M. Alhajjat, Beverly S. Strong, Amanda E. Lee, Lucas E. Turner, Ram K. Wadhwani, John R. Ortaldo, Jonathan W. Heusel and Aimen F. Shaaban J Immunol 2015; 195:1506-1516; Prepublished online 1 July 2015; Downloaded from doi: 10.4049/jimmunol.1500463 http://www.jimmunol.org/content/195/4/1506 http://www.jimmunol.org/ Supplementary http://www.jimmunol.org/content/suppl/2015/07/01/jimmunol.150046 Material 3.DCSupplemental References This article cites 45 articles, 24 of which you can access for free at: http://www.jimmunol.org/content/195/4/1506.full#ref-list-1 Why The JI? Submit online. by guest on September 23, 2021 • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2015 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Prenatal Allospecific NK Cell Tolerance Hinges on Instructive Allorecognition through the Activating Receptor during Development Amir M. -

Type 1 Regulatory T Cells: a New Mechanism of Peripheral Immune Tolerance
Cellular & Molecular Immunology (2015) 12, 566–571 ß 2015 CSI and USTC. All rights reserved 1672-7681/15 $32.00 www.nature.com/cmi REVIEW Type 1 regulatory T cells: a new mechanism of peripheral immune tolerance Hanyu Zeng, Rong Zhang, Boquan Jin and Lihua Chen The lack of immune response to an antigen, a process known as immune tolerance, is essential for the preservation of immune homeostasis. To date, two mechanisms that drive immune tolerance have been described extensively: central tolerance and peripheral tolerance. Under the new nomenclature, thymus-derived regulatory T (tTreg) cells are the major mediators of central immune tolerance, whereas peripherally derived regulatory T (pTreg) cells function to regulate 1 peripheral immune tolerance. A third type of Treg cells, termed iTreg, represents only the in vitro-induced Treg cells . Depending on whether the cells stably express Foxp3, pTreg, and iTreg cells may be divided into two subsets: the classical 1 1 1 2 2 CD4 Foxp3 Treg cells and the CD4 Foxp3 type 1 regulatory T (Tr1) cells . This review focuses on the discovery, associated biomarkers, regulatory functions, methods of induction, association with disease, and clinical trials of Tr1 cells. Cellular & Molecular Immunology (2015) 12, 566–571; doi:10.1038/cmi.2015.44; published online 8 June 2015 Keywords: biomarkers; clinical trials; regulatory functions; type 1 regulatory T cells INTRODUCTION functions of these cells and ultimately to apply this knowledge The induction and formation of peripheral immune tolerance to the treatment of associated diseases. is essential to maintaining stability of the immune system. In addition to the immune system’s major roles in regulating THE DISCOVERY OF TR1 CELLS clonal deletion, antigen sequestration, and expression at privi- Tr1 cells were first described by Roncarolo et al. -

Transplanted Thymus Thymus Nor the Development of Impairs Neither the Recovery of Recipient Depleted Lymphocyte Infusion
CD4+ T Cell −Depleted Lymphocyte Infusion Impairs Neither the Recovery of Recipient Thymus nor the Development of Transplanted Thymus This information is current as of September 26, 2021. Ming Shi, Ming Li, Yunze Cui, Lin Liu, Yasushi Adachi and Susumu Ikehara J Immunol 2013; 190:2976-2983; Prepublished online 4 February 2013; doi: 10.4049/jimmunol.1201605 Downloaded from http://www.jimmunol.org/content/190/6/2976 Supplementary http://www.jimmunol.org/content/suppl/2013/02/04/jimmunol.120160 http://www.jimmunol.org/ Material 5.DC1 References This article cites 36 articles, 10 of which you can access for free at: http://www.jimmunol.org/content/190/6/2976.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision by guest on September 26, 2021 • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Author Choice Freely available online through The Journal of Immunology Author Choice option Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2013 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology CD4+ T Cell–Depleted Lymphocyte Infusion Impairs Neither the Recovery of Recipient Thymus nor the Development of Transplanted Thymus Ming Shi,* Ming Li,* Yunze Cui,*,† Lin Liu,* Yasushi Adachi,*,‡ and Susumu Ikehara* Thymus transplantation, in conjunction with bone marrow transplantation (BMT), has been attracting attention for the treatment of various diseases. -

Plasmodium Asexual Growth and Sexual Development in the Haematopoietic Niche of the Host
REVIEWS Plasmodium asexual growth and sexual development in the haematopoietic niche of the host Kannan Venugopal 1, Franziska Hentzschel1, Gediminas Valkiūnas2 and Matthias Marti 1* Abstract | Plasmodium spp. parasites are the causative agents of malaria in humans and animals, and they are exceptionally diverse in their morphology and life cycles. They grow and develop in a wide range of host environments, both within blood- feeding mosquitoes, their definitive hosts, and in vertebrates, which are intermediate hosts. This diversity is testament to their exceptional adaptability and poses a major challenge for developing effective strategies to reduce the disease burden and transmission. Following one asexual amplification cycle in the liver, parasites reach high burdens by rounds of asexual replication within red blood cells. A few of these blood- stage parasites make a developmental switch into the sexual stage (or gametocyte), which is essential for transmission. The bone marrow, in particular the haematopoietic niche (in rodents, also the spleen), is a major site of parasite growth and sexual development. This Review focuses on our current understanding of blood-stage parasite development and vascular and tissue sequestration, which is responsible for disease symptoms and complications, and when involving the bone marrow, provides a niche for asexual replication and gametocyte development. Understanding these processes provides an opportunity for novel therapies and interventions. Gametogenesis Malaria is one of the major life- threatening infectious Malaria parasites have a complex life cycle marked Maturation of male and female diseases in humans and is particularly prevalent in trop- by successive rounds of asexual replication across gametes. ical and subtropical low- income regions of the world. -
Thymus Transplantation Reference Number: CP.MP.189 Coding Implications Date of Last Revision: 06/21 Revision Log
Clinical Policy: Thymus Transplantation Reference Number: CP.MP.189 Coding Implications Date of Last Revision: 06/21 Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Complete DiGeorge anomaly is a disorder in which a person has no thymus function. Without thymus function, bone marrow stem cells do not develop into T cells, which results in immunodeficiency. Without successful treatment, patients usually die by 2 years of age. Thymus transplantation with and without immunosuppression has resulted in the development good T cell function in complete DiGeorge anomaly subjects.1 Policy/Criteria I. It is the policy of health plans affiliated with Centene Corporation® that thymus transplant (use of RVT-802) requires secondary review, due to limited evidence, when meeting all of the following: A. Complete or “atypical” DiGeorge syndrome with poor thymus function, per medical testing laboratory studies and physical examination, as confirmed by the thymus transplant clinical trial (NCT01220531); B. Immunodeficiency, or severe autoimmunity for which development of naïve T cells would be expected to lead to clinical improvement; C. Flow cytometry and phytohaemagglutinin (PHA) studies are planned to occur twice, once within 3 months of transplantation and once within one month of transplantation. Studies must be performed in a CLIA or CAP certified laboratory, preferably Duke Clinical Immunology Laboratory; D. None of the following contraindications: 1. Malignancy, except for non-melanoma localized skin cancer that has been treated appropriately, a malignancy that has been completely resected, or a treated malignancy determined to have a small likelihood of recurrence and acceptable future risks; 2. -

Thymocytes May Persist and Differentiate Without Any Input from Bone Marrow Progenitors
Brief Definitive Report Thymocytes may persist and differentiate without any input from bone marrow progenitors Laetitia Peaudecerf,1 Sara Lemos,1 Alessia Galgano,1 Gerald Krenn,1 Florence Vasseur,1 James P. Di Santo,2 Sophie Ezine,1 and Benedita Rocha1 1Institut National de la Santé et de la Recherche Médicale, Unit 1020, Faculty of Medicine Descartes Paris V, 75015 Paris, France 2Innate Immunity Unit, Pasteur Institute, 75724 Paris, France Thymus transplants can correct deficiencies of the thymus epithelium caused by the com- plete DiGeorge syndrome or FOXN1 mutations. However, thymus transplants were never used to correct T cell–intrinsic deficiencies because it is generally believed that thymocytes have short intrinsic lifespans. This notion is based on thymus transplantation experiments where it was shown that thymus-resident cells were rapidly replaced by progenitors origi- nating in the bone marrow. In contrast, here we show that neonatal thymi transplanted into interleukin 7 receptor–deficient hosts harbor populations with extensive capacity to self-renew, and maintain continuous thymocyte generation and export. These thymus transplants reconstitute the full diversity of peripheral T cell repertoires one month after surgery, which is the earliest time point studied. Moreover, transplantation experiments performed across major histocompatibility barriers show that allogeneic transplanted thymi are not rejected, and allogeneic cells do not induce graft-versus-host disease; transplants induced partial or total protection to infection. These results challenge the current dogma that thymocytes cannot self-renew, and indicate a potential use of neonatal thymus trans- plants to correct T cell–intrinsic deficiencies. Finally, as found with mature T cells, they show that thymocyte survival is determined by the competition between incoming progeni- tors and resident cells. -

The Role of Natural Killer Cells in Pathogenesis of Autoimmune Diseases
Review paper DOI: 10.5114/ceji.2015.56971 The role of natural killer cells in pathogenesis of autoimmune diseases Katarzyna PoPKo, ElżbiEta GórsKa Medical University of Warsaw, Poland Abstract There is growing evidence that NK cell-mediated immunoregulation plays an important role in the control of autoimmunity. NK cells are a subset of lymphocytes that generally contribute to innate immu- nity but have also a great impact on the function of t and b lymphocytes. the major role of nK cells is cytotoxic reaction against neoplastic, infected and autoreactive cells, but they regulatory function seems to play more important role in the pathogenesis of autoimmune diseases. Numerous studies suggested the involvement of nK cells in pathogenesis of such a common autoimmune diseases as juvenile rheu- matoid arthritis, type i diabetes and autoimmune thyroid diseases. the defects of nK cells regulatory function as well as cytotoxic abilities are common in patients with autoimmune diseases with serious consequences including HLH hemophagocytic lymphocytosis (HLH) and macrophage activation syn- drome (Mas). the early diagnosis of nK cells defect responsible for the loss of the protective abilities is crucial for the prevention of life-threatening complications and implementation of necessary treatment. Key words: nK cells, autoimmune reaction, Hashimoto thyroiditis, type 1 diabetes, juvenile rheumatoid arthritis. (Cent Eur J immunol 2015; 40 (4): 470-476) Natural killer cells function receptors (2B4) play activating roles [6-8]. The inhibition Natural killer cells are a subset of lymphocytes that of NK cell activation depends on the presence of MHC contribute to innate immunity. They are developed in the class I molecules. -

Results of Gal-Knockout Porcine Thymokidney Xenografts
Results of Gal-Knockout Porcine Thymokidney Xenografts The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Griesemer, A. D., A. Hirakata, A. Shimizu, S. Moran, A. Tena, H. Iwaki, Y. Ishikawa, et al. 2009. “Results of Gal-Knockout Porcine Thymokidney Xenografts.” American Journal of Transplantation 9 (12) (December): 2669–2678. doi:10.1111/j.1600-6143.2009.02849.x. Published Version doi:10.1111/j.1600-6143.2009.02849.x Citable link https://nrs.harvard.edu/URN-3:HUL.INSTREPOS:37364476 Terms of Use This article was downloaded from Harvard University’s DASH repository, WARNING: This file should NOT have been available for downloading from Harvard University’s DASH repository.;This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http://nrs.harvard.edu/ urn-3:HUL.InstRepos:dash.current.terms-of-use#LAA NIH Public Access Author Manuscript Am J Transplant. Author manuscript; available in PMC 2010 November 20. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: Am J Transplant. 2009 December ; 9(12): 2669±2678. doi:10.1111/j.1600-6143.2009.02849.x. Results of Gal-Knockout porcine thymokidney xenografts Adam D. Griesemer1, Atsushi Hirakata1, Akira Shimizu1, Shannon Moran1, Aseda Tena1, Hideyuki Iwaki1, Yoshinori Ishikawa1, Patrick Schule1, J. Scott Arn1, Simon C. Robson2, Jay A. Fishman3, Megan Sykes1, David H. Sachs1, and Kazuhiko Yamada1,4 1Transplantation Biology Research Center, Massachusetts General Hospital, Harvard Medical School, Boston, MA 2Transplant Center, Department of Medicine, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA 3Division of Infectious Diseases, Massachusetts General Hospital, Harvard Medical School, Boston, MA. -

Regulatory T-Cell Therapy in Crohn's Disease: Challenges and Advances
Recent advances in basic science Regulatory T- cell therapy in Crohn’s disease: Gut: first published as 10.1136/gutjnl-2019-319850 on 24 January 2020. Downloaded from challenges and advances Jennie N Clough ,1,2 Omer S Omer,1,3 Scott Tasker ,4 Graham M Lord,1,5 Peter M Irving 1,3 1School of Immunology and ABStract pathological process increasingly recognised as Microbial Sciences, King’s The prevalence of IBD is rising in the Western world. driving intestinal inflammation and autoimmunity College London, London, UK 2NIHR Biomedical Research Despite an increasing repertoire of therapeutic targets, a is the loss of immune homeostasis secondary to Centre at Guy’s and Saint significant proportion of patients suffer chronic morbidity. qualitative or quantitative defects in the regulatory Thomas’ NHS Foundation Trust Studies in mice and humans have highlighted the critical T- cell (Treg) pool. and King’s College, London, UK + 3 role of regulatory T cells in immune homeostasis, with Tregs are CD4 T cells that characteristically Department of defects in number and suppressive function of regulatory Gastroenterology, Guy’s and express the high- affinity IL-2 receptor α-chain Saint Thomas’ Hospitals NHS T cells seen in patients with Crohn’s disease. We review (CD25) and master transcription factor Forkhead Trust, London, UK the function of regulatory T cells and the pathways by box P-3 (Foxp3) which is essential for their suppres- 4 Division of Transplantation which they exert immune tolerance in the intestinal sive phenotype and stability.4–6