Ambulance Service Categories Basic Life Support
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

EMS Medical Director Guidebook
Medical Director Guidebook May 2016 Maine Emergency Medical Services Department of Public Safety 152 State House Station Augusta, ME 04333 www.maine.gov/ems Authors Christopher Paré, Paramedic J. Matthew Sholl, M.D., M.P.H. Eric Wellman, Paramedic Contributors Jay Bradshaw Jonnathan Busko, MD Myles Block, Paramedic Emily Carter, Paramedic Marlene Cormier, M.D. Shawn Evans, Paramedic Kevin Kendall, M.D. Rick Petrie, Paramedic Tim Pieh, M.D. Kerry Pomelow, Paramedic Mike Schmitz, D.O. Nate Yerxa, Paramedic Table of Contents Foreword 1 The Maine EMS System Structure 2 Legal Aspects & System Rules 6 EMS Systems 18 Maine EMS Medical Director Qualifications 23 Medical Oversight 31 EMS Personnel & Providers 36 EMS Operations 38 Interfacility Patient Transport 49 EMS Education 51 Grants & System Funding 55 Quality Assurance & System Improvement 57 Maine EMS Protocols & Standing Orders 65 Appendix A: Disaster Planning 70 Appendix B: Wilderness EMS 80 Appendix C: Tactical EMS 82 Appendix D: Death Situations for Medical Responders 83 Appendix E: Maine EMS Scope of Practice by License Level 88 Appendix F: Maine EMS Interfacility Transport: Decision Tree and Scope of Practice for Transfer by 93 License Level Appendix G: Recommended Service Policies 99 Appendix H: Checklist for the new medical director 100 References 101 Glossary of Acronyms 103 Index 104 FOREWORD The Maine EMS Medical Director’s Guidebook was designed to provide physicians and EMS services with direction on how to navigate the Maine EMS system. Our goal with this guidebook is to educate and in- form all users of the system to the role of EMS physician medical direction. -

First Responder (2013)
THE NATIONAL ACADEMIES PRESS This PDF is available at http://nap.edu/22451 SHARE The Legal Definitions of First Responder (2013) DETAILS 30 pages | 8.5 x 11 | PAPERBACK ISBN 978-0-309-28369-4 | DOI 10.17226/22451 CONTRIBUTORS GET THIS BOOK Bricker, Lew R. C.; Petermann, Tanya N.; Hines, Margaret; and Sands, Jocelyn FIND RELATED TITLES SUGGESTED CITATION National Academies of Sciences, Engineering, and Medicine 2013. The Legal Definitions of First Responder . Washington, DC: The National Academies Press. https://doi.org/10.17226/22451. Visit the National Academies Press at NAP.edu and login or register to get: – Access to free PDF downloads of thousands of scientific reports – 10% off the price of print titles – Email or social media notifications of new titles related to your interests – Special offers and discounts Distribution, posting, or copying of this PDF is strictly prohibited without written permission of the National Academies Press. (Request Permission) Unless otherwise indicated, all materials in this PDF are copyrighted by the National Academy of Sciences. Copyright © National Academy of Sciences. All rights reserved. The Legal Definitions of “First Responder” November 2013 NATIONAL COOPERATIVE HIGHWAY RESEARCH PROGRAM Responsible Senior Program Officer: Stephan A. Parker Research Results Digest 385 THE LEGAL DEFINITIONS OF “FIRST RESPONDER” This digest presents the results of NCHRP Project 20-59(41), “Legal Definition of ‘First Responder’.” The research was conducted by Lew R. C. Bricker, Esquire, and Tanya N. Petermann, Esquire, of Smith Amundsen, Chicago, IL; Margaret Hines, Esquire; and Jocelyn Sands, J. D. James B. McDaniel was the Principal Investigator. INTRODUCTION Congress and in some congressional bills that were not enacted into law. -
Paramedic Treatment Protocols
Paramedic Treatment Protocols West Virginia Office of Emergency Medical Services EMS Protocols Paramedic Treatment Protocol TABLE OF CONTENTS Preface Acknowledgments Using the Protocols INITIAL TREATMENT / UNIVERSAL PATIENT CARE TRAUMA 4100 Severe External Bleeding 4101 Selective Spinal Immobilization 4102 Chest Trauma 4104 Abdominal Trauma 4105 Musculoskeletal Trauma 4106 Head Trauma 4107 Hypoperfusion / Shock 4108 Traumatic Arrest 4109 Burns 4110 Eye Injuries 4111 Tranexamic Acid (TXA) 4112 CARDIAC 4200 Chest Pain 4202 Severe Hypertension 4203 Cardiac Arrest 4205 Tachycardia 4208 Symptomatic Bradycardia 4211 Right Ventricular AMI 4213 Return of Spontaneous Circulation - ROSC 4214 RESPIRATORY 4300 Bronchospasm 4302 Pulmonary Edema 4303 Inhalation Injury 4304 Airway Obstruction 4305 PEDIATRIC 4400 Medical Assessment 4401 Hypoperfusion / Shock 4402 Seizures 4403 Child Neglect / Abuse 4404 Sudden Infant Death Syndrome 4405 Cardiac Arrest 4406 West Virginia Office of Emergency Medical Services – Statewide Protocols Page 1 of 3 Paramedic Treatment Protocol TABLE OF CONTENTS Cardiac Dysrhythmias 4407 Trauma Assessment 4408 Fever 4409 Newborn Infant Care 4410 Pediatric Diabetic Emergencies 4411 Allergic Reaction / Anaphylaxis 4412 Bronchospasm 4413 ENVIRONMENTAL 4500 Allergic Reaction / Anaphylaxis 4501 Heat Exposure 4502 Cold Exposure 4503 Snake Bite 4504 Near Drowning / Drowning 4505 MEDICAL 4600 Hypoperfusion / Shock 4601 Stroke / TIA 4602 Seizures 4603 Diabetic Emergencies 4604 Unconscious / Altered Mental Status 4605 Overdose / Ingestion -

Ambulance Helicopter Contribution to Search and Rescue in North Norway Ragnar Glomseth1, Fritz I
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Springer - Publisher Connector Glomseth et al. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine (2016) 24:109 DOI 10.1186/s13049-016-0302-8 ORIGINAL RESEARCH Open Access Ambulance helicopter contribution to search and rescue in North Norway Ragnar Glomseth1, Fritz I. Gulbrandsen2,3 and Knut Fredriksen1,4* Abstract Background: Search and rescue (SAR) operations constitute a significant proportion of Norwegian ambulance helicopter missions, and they may limit the service’s capacity for medical operations. We compared the relative contribution of the different helicopter resources using a common definition of SAR-operation in order to investigate how the SAR workload had changed over the last years. Methods: We searched the mission databases at the relevant SAR and helicopter emergency medical service (HEMS) bases and the Joint Rescue Coordination Centre (North) for helicopter-supported SAR operations within the potential operation area of the Tromsø HEMS base in 2000–2010. We defined SAR operations as missions over land or sea within 10 nautical miles from the coast with an initial search phase, missions with use of rescue hoist or static rope, and avalanche operations. Results: There were 769 requests in 639 different SAR operations, and 600 missions were completed. The number increased during the study period, from 46 in 2000 to 77 in 2010. The Tromsø HEMS contributed with the highest number of missions and experienced the largest increase, from 10 % of the operations in 2000 to 50 % in 2010. Simple terrain and sea operations dominated, and avalanches accounted for as many as 12 % of all missions. -

NIMS 508 Stillwater Flood Search and Rescue Team
Resource Typing Definition for Response Mass Search and Rescue Operations STILLWATER/FLOOD SEARCH AND RESCUE TEAM DESCRIPTION The Stillwater/Flood Search and Rescue (SAR) Team conducts search, rescue, and recovery operations for humans and animals in stillwater and stillwater/flood environments RESOURCE CATEGORY Search and Rescue RESOURCE KIND Team OVERALL FUNCTION The Stillwater/Flood SAR team: 1. Searches for and rescues individuals who may be injured or otherwise in need of medical attention 2. Provides emergency medical care, including Basic Life Support (BLS) 3. Provides animal rescue 4. Transports humans and animals to the nearest location for secondary land or air transport 5. Provides shore-based and boat-based water rescue for humans and animals 6. Supports helicopter rescue operations and urban SAR in water environments for humans and animals 7. Operates in environments with or without infrastructure, including environments with disrupted access to roadways, utilities, transportation, and medical facilities, and with limited access to shelter, food, and water COMPOSITION AND ORDERING 1. Requestor and provider address certain needs and issues prior to deployment, including: SPECIFICATIONS a. Communications equipment that enables more than intra-team communications, such as programmable interoperable communications equipment with capabilities for command, logistics, military, air, and so on b. Type of incident and operational environment, such as weather event, levy or dam breach, or risk of hazardous materials (HAZMAT) contamination c. Additional specialized personnel, such as advanced medical staff, animal SAR specialists, logistics specialists, advisors, helicopter support staff, or support personnel for unique operating environments d. Additional transportation-related needs, including specific vehicles, boats, trailers, drivers, mechanics, equipment, supplies, fuel, and so on e. -
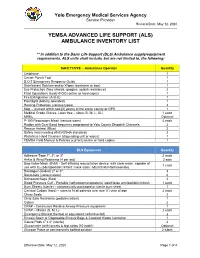
(Als) Ambulance Inventory List
Yolo Emergency Medical Services Agency Service Provider Revised Date: May 12, 2020 YEMSA ADVANCED LIFE SUPPORT (ALS) AMBULANCE INVENTORY LIST ** In addition to the Basic Life Support (BLS) Ambulance supply/equipment requirements, ALS units shall include, but are not limited to, the following: SAFETY/PPE – Ambulance Operator Quantity Cellphone 1 Center Punch Tool 1 D.O.T Emergency Response Guide 1 Disinfectant Solution and/or Wipes (container or box) 1 Eye Protection (face shields, goggles, splash resistance) 2 Field Operations Guide (FOG) online or hard copies 1 Fire Extinguisher (A-B-C) 1 Flashlight (battery operated) 1 Hearing Protection (various types) 2 Map – (current within two [2] years) of the entire county or GPS 1 Medical Grade Gloves, Latex free – sizes (S, M, L, XL) 1 each MREs Optional P-100 Respiratory Mask (various sizes) 4 each Radios with Dual Band frequency programed to Yolo County Dispatch Channels 2 Rescue Helmet (Blue) 2 Safety Vest meeting ANSI/OSHA standards 2 Waterless Hand Cleanser (dispensing unit or wipes) 1 YEMSA Field Manual & Policies (current) online or hard copies 1 BLS Equipment Quantity Adhesive Tape 1", 2", or 3" 2 each Ankle & Wrist Restraints (4 per set) 2 sets Bag-Valve-Mask (BVM) - Self-inflating resuscitation device, with clear mask, capable of 1 each use with O2 (adult/pediatric/infant; mask sizes: adult/child/infant/neonate) Bandages (Rolled) 2" or 3" 3 Band-Aids (various sizes) 6 Biohazard Bags (Red) 2 Blood Pressure Cuff - Portable (sphygmomanometers) (adult/large arm/pediatric/infant) 1 each -

Healthy Choices Get a Head Start on Great Health
Healthy Choices Get a Head Start on Great Health 2015 Benefits Guide MedStar Georgetown University Hospital, Non-union MedStar Health Research Institute MedStar National Rehabilitation Network Non-hospital Based Businesses, South Table of Contents 1 Enrollment Checklist 2 Enrollment Guidelines 3 Online Enrollment Instructions 4 Wellness Resources 4 Your Medical Plan Options 5 COBRA Continued Benefit Coverage 6 2015 Medical Plan Options Chart 8 Prescription Drug Plans 9 Your Dental Plan Options 11 Your Vision Plan Option 12 Flexible Spending Accounts (FSAs) 14 Life Insurance 14 Accidental Death and Dismemberment Insurance 15 Disability Plans 15 Universal Life, Critical Illness and Accident Insurances 16 Legal Resources 16 MedStar Associate Advantages 18 Contact Information i 2015 Annual Enrollment Choices For Healthy Living MedStar Health provides a comprehensive benefits If you are a benefit-eligible associate, take advantage of package for you and your family—MedStar Total MedStar Total Rewards. You must enroll online to receive Rewards. You are responsible for selecting the best mix medical, dental, vision, flexible spending accounts, of benefits to meet your needs and actively managing supplemental life, supplemental accidental death and these benefits and your health throughout the year. Use dismemberment, dependent life, or legal coverage in 2015. this guide to select your MedStar Total Rewards health and welfare package for 2015. Enrollment Checklist Read through this guide to design your MedStar Total Rewards package for 2015. Medical Accidental Death and Dismemberment Elect a healthcare coverage option. Insurance • MedStar Select Plan Consider if additional coverage would give your • CareFirst BlueCross BlueShield Preferred family more peace of mind. Provider Organization (PPO) Plan • Kaiser Permanente Health Maintenance Disability Organization (HMO) Plan MedStar provides full-time associates with short- and long-term disability coverage equal to 60 Dental percent of your base pay, at no cost to you. -

Kern County Sheriff's Office Search and Rescue Policies and Procedures Table of Contents
KERN COUNTY SHERIFF'S OFFICE SEARCH AND RESCUE POLICIES AND PROCEDURES ______________________________________________________________________________ TABLE OF CONTENTS ______________________________________________________________________________ A -- INTRODUCTION A-100 Introduction-Mission Statement A-110 Manual Revisions A-200 Definitions A-300 Organizational Structure B -- RESPONSIBILITIES OF PERSONNEL B-100 Duties of Search and Rescue Coordinator B-200 Duties of Search and Rescue Members C -- SELECTION OF SEARCH AND RESCUE MEMBERSHIP C-100 Selection of Members C-200 Probationary Period C-300 Leave of Absence C-400 Termination D -- SEARCH AND RESCUE RANK STRUCTURE D-100 Rank Structure and Responsibilities D-200 Rank Insignia E -- SEARCH AND RESCUE TRAINING E-100 Training E-200 Training Forecast E-300 Training Documentation F -- SEARCH AND RESCUE MEETINGS F-100 Meetings Page 1 of 1 _____________________________________________________________________________ TABLE OF CONTENTS ______________________________________________________________________________ G -- ADMINISTRATIVE POLICIES G-100 Call-Out Procedures - In County G-200 Call-Out Procedures - Mutual Aid G-300 Aircraft Operations G-400 Incident Command System G-500 Uniforms and Appearance G-600 Donations and Grants G-700 Discipline G-800 Firearms G-900 Injuries G-1000 Media Relations G-1100 Medical Responsibilities G-1200 Member Compensation G-1300 Vehicle Operation G-1400 SAR BLS Policy Page 2 of 2 Page 3 of 3 KERN COUNTY SHERIFF'S OFFICE SEARCH AND RESCUE POLICIES AND PROCEDURES -
Talking Points
DEPARTMENT OF HEALTH & HUMAN SERVICES Centers for Medicare & Medicaid Services 7500 Security Boulevard, Mail Stop S2-12-25 Baltimore, Maryland 21244-1850 Center for Medicaid and State Operations/Survey and Certification Group Ref: S&C-07-19 DATE: April 26, 2007 TO: State Survey Agency Directors FROM: Director Survey and Certification Group SUBJECT: Provision of Emergency Services - Important Requirements for Hospitals Memorandum Summary • All hospitals are required to appraise medical emergencies, provide initial treatment and referral when appropriate, regardless of whether the hospital has an emergency department. • A hospital is not in compliance with the Medicare Conditions of Participation (CoPs) if it relies on 9-1-1 services as a substitute for the hospital’s own ability to provide services otherwise required in the CoPs. This means, among other things, that a hospital may not rely on 9-1-1 services to provide appraisal or initial treatment of individuals in lieu of its own capability to do so. In this memorandum we affirm and explain current regulatory requirements pertaining to a hospital’s ability to meet the emergency needs of individuals. Any hospital participating in Medicare, regardless of the type of hospital and regardless of whether the hospital has an emergency department must have the capability to provide basic emergency care interventions. Requirements Applicable to All Hospitals (except Critical Access Hospitals) The following Medicare hospital Conditions of Participation (CoP) apply to all participating hospitals (except Critical Access Hospitals) and provide a foundation for safe care for all persons, including those with emergency care needs. Critical Access Hospitals (CAHs) are governed by regulations separate from those governing hospitals, and may be found at 42 CFR 485.618. -

Accident Knowledge and Emergency Management
Ris0-R-945(EN) DK9700056 Accident Knowledge and Emergency Management Birgitte Rasmussen, Carsten D. Gr0nberg Ris0 National Laboratory, Roskilde, Denmark March 1997 VOL 2 p III 1 2 Accident Knowledge and Emergency Management Birgitte Rasmussen, Carsten D. Gr0nberg Ris0 National Laboratory, Roskilde, Denmark March 1997 Abstract. The report contains an overall frame for transformation of knowledge and experience from risk analysis to emergency education. An accident model has been developed to describe the emergency situation. A key concept of this model is uncontrolled flow of energy (UFOE), essential ele- ments are the state, location and movement of the energy (and mass). A UFOE can be considered as the driving force of an accident, e.g., an explosion, a fire, a release of heavy gases. As long as the energy is confined, i.e. the location and movement of the energy are under control, the situation is safe, but loss of con- finement will create a hazardous situation that may develop into an accident. A domain model has been developed for representing accident and emergency scenarios occurring in society. The domain model uses three main categories: status, context and objectives. A domain is a group of activities with allied goals and elements and ten specific domains have been investigated: process plant, storage, nuclear power plant, energy distribution, marine transport of goods, marine transport of people, aviation, transport by road, transport by rail and natural disasters. Totally 25 accident cases were consulted and information was extracted for filling into the schematic representations with two to four cases pr. specific domain. The work described in this report is financially supported by EUREKA MEM- brain (Major Emergency Management) project running 1993-1998. -

Basic Life Support Health Care Provider
ELLIS & ASSOCIATES Health Care Provider Basic Life Support MEETS CURRENT CPR & ECC GUIDELINES Ellis & Associates / Safety & Health HEALTH CARE PROVIDER BASIC LIFE SUPPORT - I Ellis & Associates, Inc. P.O. Box 2160, Windermere, FL 34786-2160 www.jellis.com Copyright © 2016 by Ellis & Associates, LLC All rights reserved. No part of this publication may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the publisher, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law. For permission requests, write to the publisher, addressed “Attention: Permissions Coordinator,” at the address below. Ellis & Associates P.O. Box 2160, Windermere, FL 34786-2160 Ordering Information: Quantity sales. Special discounts are available on quantity purchases by corporations, associations, trade bookstores and wholesalers. For details, contact the publisher at the address above. Disclaimer: The procedures and protocols presented in this manual and the course are based on the most current recommendations of responsible medical sources, including the International Liaison Committee on Resuscitation (ILCOR) 2015 Guidelines for CPR & ECC. Ellis & Associates, however, make no guarantee as to, and assume no responsibility for, the correctness, sufficiency, or completeness of such recommendations or information. Additional procedures may be required under particular circumstances. Ellis & Associates disclaims all liability for damages of any kind arising from the use of, reference to, reliance on, or performance based on such information. Library of Congress Cataloging-in-Publication Data Not Available at Time of Printing ISBN 978-0-9961108-0-8 Unless otherwise indicated on the Credits Page, all photographs and illustrations are copyright protected by Ellis & Associates. -

Emergency Medical Services Statutes and Regulations
Emergency Medical Services Statutes and Regulations Printed: August 2016 Effective: September 11, 2016 1 9/16/2016 Statutes and Regulations Table of Contents Title 63 of the Oklahoma Statutes Pages 3 - 13 Sections 1-2501 to 1-2515 Constitution of Oklahoma Pages 14 - 16 Article 10, Section 9 C Title 19 of the Oklahoma Statutes Pages 17 - 24 Sections 371 and 372 Sections 1- 1201 to 1-1221 Section 1-1710.1 Oklahoma Administrative Code Pages 25 - 125 Chapter 641- Emergency Medical Services Subchapter 1- General EMS programs Subchapter 3- Ground ambulance service Subchapter 5- Personnel licenses and certification Subchapter 7- Training programs Subchapter 9- Trauma referral centers Subchapter 11- Specialty care ambulance service Subchapter 13- Air ambulance service Subchapter 15- Emergency medical response agency Subchapter 17- Stretcher aid van services Appendix 1 Summary of rule changes Approved changes to the June 11, 2009 effective date to the September 11, 2016 effective date 2 9/16/2016 §63-1-2501. Short title. Sections 1-2502 through 1-2521 of this title shall be known and may be cited as the "Oklahoma Emergency Response Systems Development Act". Added by Laws 1990, c. 320, § 5, emerg. eff. May 30, 1990. Amended by Laws 1999, c. 156, § 1, eff. Nov. 1, 1999. NOTE: Editorially renumbered from § 1-2401 of this title to avoid a duplication in numbering. §63-1-2502. Legislative findings and declaration. The Legislature hereby finds and declares that: 1. There is a critical shortage of providers of emergency care for: a. the delivery of fast, efficient emergency medical care for the sick and injured at the scene of a medical emergency and during transport to a health care facility, and b.