Southend University Hospital Newapproachfocused Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(Public Pack)Agenda Document for Development Control Committee
Public Document Pack SOUTHEND-ON-SEA BOROUGH COUNCIL Development Control Committee Date: Wednesday, 8th June, 2016 Time: 2.00 pm Place: Committee Room 1 - Civic Suite Contact: Tim Row Email: [email protected] A G E N D A 1 Apologies for Absence 2 Declarations of Interest 3 Minutes of the Meeting held on Wednesday 2nd March 2016 (Pages 1 - 36) 4 Minutes of the Meeting held on Wednesday 13th April 2016 (Pages 37 - 70) **** Contents List & Introduction 5 Supplementary Report 6 Report on Planning Applications - Pre-Meeting Site Visits (Pages 75 - 104) Report of Corporate Director for Place 7 Report on Planning Applications - Main Plans List (Pages 105 - 230) Report of Corporate Director for Place 8 Enforcement of Planning Control (Pages 231 - 260) Report of Corporate Director for Place TO: The Chairman & Members of the Development Control Committee: Councillor Waterworth (Chair) Councillors D Garston (Vice-Chair), Arscott, M Assenheim, B Ayling, M Borton, M Butler, Callaghan, Evans, N Folkard, J Garston, Hadley, Jones, Mulroney, Norman MBE, Van Looy and Walker PLEASE NOTE: The minibus for the site visits will depart from the bus stop at the front of the Civic Centre at 11.15 a.m. This page is intentionally left blank Public Document Pack SOUTHEND-ON-SEA BOROUGH COUNCIL Meeting of Development Control Committee Date: Wednesday, 2nd March, 2016 Place: Committee Room 4a - Civic Suite 3 Present: Councillor A Crystall (Chair) Councillors B Ayling, M Borton, M Butler, Byford, Callaghan, Evans, N Folkard, J Garston*, Hadley, Jones*, Kenyon*, D McGlone, K Robinson, M Stafford*, Van Looy and Walker *Substitute in accordance with Council Procedure Rule 31. -
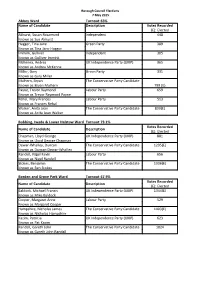
Abbey Ward Turnout 63% Name of Candidate Description Votes
Borough Council Elections 7 May 2015 Abbey Ward Turnout 63% Name of Candidate Description Votes Recorded (E): Elected Akhurst, Susan Rosamund Independent 448 Known as Sue Akhurst Hagger, Tina Jane Green Party 389 Known as Tina Jane Hagger Immink, Gulliver Independent 305 Known as Gulliver Immink McKenna, Andrea UK Independence Party (UKIP) 365 Known as Andrea McKenna Miller, Gary Green Party 331 Known as Gary Miller Mulhern, Bryan The Conservative Party Candidate Known as Bryan Mulhern 799 (E) Payne, Trevor Raymond Labour Party 659 Known as Trevor Raymond Payne Rehal, Mary Frances Labour Party 513 Known as Frances Rehal Walker, Anita Jean The Conservative Party Candidate 839(E) Known as Anita Jean Walker Bobbing, Iwade & Lower Halstow Ward Turnout 73.1% Votes Recorded Name of Candidate Description (E): Elected Chapman, Lloyd George UK Independence Party (UKIP) 881 Known as Lloyd George Chapman Dewar-Whalley, Duncan The Conservative Party Candidate 1295(E) Known as Duncan Dewar-Whalley Randell, Nigel Kevin Labour Party 656 Known as Nigel Randell Stokes, Benjamin The Conservative Party Candidate 1336(E) Known as Ben Stokes Borden and Grove Park Ward Turnout 67.9% Votes Recorded Name of Candidate Description (E): Elected Baldock, Michael Francis UK Independence Party (UKIP) 1344(E) Known as Mike Baldock Cooper, Margaret Anne Labour Party 529 Known as Margaret Cooper Hampshire, Nicholas James The Conservative Party Candidate 1403(E) Known as Nicholas Hampshire Kazim, Patricia UK Independence Party (UKIP) 623 Known as Pat Kazim Randall, Gareth -

SOUTHEND-ON-SEA in the COUNTY of ESSEX T S \ 1
Local Government Boundary Commission For England Report No. 14 LOCAL GOVERNMENT BOUNDARY COMMISSION FOR ENGLAND REPORT NO 14 LOCAL GOVERNMENT BOUNDARY COMMISSION FOR ENGLAND CHAIRMAN Sir Edmund Compton, GCB, KBE DEPUTY CHAIRMAN Mr J M Rankin, QC The Countess of Albemarle, DBS Mr T C Benfield Professor Michael Chisholm Sir Andrew Wheatley, CBE Mr F B Young, CBE wL • To The Rt Hon Roy Jenkins, NIP Secretary of State for the Home Department PROPOSALS FOR FUTURE ELECTORAL ARRANGEMENTS FOR THE BOROUGH OF SOUTHEND-ON-SEA IN THE COUNTY OF ESSEX t S \ 1. We, the Local Government Boundary Commission for England, having carried out 7t our initial review of the electoral arrangements for the borough of Southend- on-Sea in accordance with the requirements of section 63 and Schedule 9 to the Local Government Act 1972, present our proposals for the future electoral arrangements for that borough. 2. In accordance with the procedure laid down in section 60(1) and (2) of the 1972 Act, notice was given on 29 January 197^ that we were to undertake this review. This was incorporated in a consultation letter addressed to the Southend- on-Sea Borough Council, copies of which were circulated to the Essex County Council, 'the Members of Parliament for the constituencies concerned and the headquarters of the main political parties. Copies were also sent to the editors of the local newspapers circulating in the area and to the local government press. Notices inserted in the local press announced the start of the review and invited comments from members of the public and from any interested bodies. -

The Rt Hon William HAGUE Secretary of State for Foreign Affairs Foreign and Commonwealth Office King Charles Street London SW1A 2AH United Kingdom
EUROPEAN COMMISSION Brussels, 21.05.2014 C(2014) 3142 final PUBLIC VERSION This document is made available for information purposes only. SUBJECT: STATE AID SA.38113 (2014/N) – UNITED KINGDOM REGIONAL AID MAP 2014-2020 Sir, 1. PROCEDURE (1) On 28 June 2013 the Commission adopted the Guidelines on regional State aid for 2014-20201 (hereinafter "RAG"). Pursuant to paragraph 178 of the RAG, each Member State should notify to the Commission, following the procedure of Article 108(3) of the Treaty on the Functioning of the European Union ("hereinafter: "TFEU"), a single regional aid map applicable from 1 July 2014 to 31 December 2020. In accordance with paragraph 179 of the RAG, the approved regional aid map is to be published in the Official Journal of the European Union, and will constitute an integral part of the RAG. (2) By letter dated 31 March 2014, registered at the Commission on the same day (2014/036591), the United Kingdom ("UK") authorities submitted a proposal for a regional aid map applicable for the period from 1 July 2014 to 31 December 2020. 2. DESCRIPTION OF THE NOTIFIED REGIONAL AID MAP (3) In their notification, the UK authorities propose a list of regions with a total population of 17.09 million inhabitants, or 27.05% of the national population, for eligibility for 1 OJ C 209, 23.07.2013, p.1 The Rt Hon William HAGUE Secretary of State for Foreign Affairs Foreign and Commonwealth Office King Charles Street London SW1A 2AH United Kingdom Commission européenne, B-1049 Bruxelles/Europese Commissie, B-1049 Brussel – Belgium Telephone: 00- 32 (0) 2 299.11.11. -

Spring 2021 Newsletter
SOUTHEND WEST CONSERVATIVE ASSOCIATION Edition 03-2021 01702 472391 or 07726 204 816 [email protected] southendwestconservatives.com Message from Chairman - Kevin Thomas Hello, I hope you are keeping well, in good spirits and have received your vaccina- tion. It has been a long year and we are still not yet out of lockdown. Our Prime Minister has given us the pathway out and let’s hope there are no setbacks and by the summer we are heading back to a more normal life. It has been the most difficult and strangest of years but for once there is a clearer light at the end of the tunnel for us all to focus on. Our Association continues to advance forward. The focus is now firmly on the forthcoming May elections and our need to get control of Southend Council back in the hands of the Con- servatives. The Conservative Group has achieved so much in opposition and has so many great plans for the future – let’s all get behind our prospective candidates and support them however we can! This is my last Newsletter as your Chairman. I have set out what I aimed to do. I have brought renewed structure to SWCA and the way our Officers work. As a team we have worked on a selection of matters relating to membership, campaigning, finance and admin- istration, putting the Association on a great footing to move forward. SWCA has moved up the rankings of Associations in the Eastern Region. We are now comfortably in the top 10 out of 60+ organisations. -

Agenda Item Number 5.2 Provider Update for Patient Safety and Quality of Care Report Board Meeting Thursday 4 September 2014
Agenda Item Number 5.2 Provider Update for Patient Safety and Quality of Care Report Board Meeting Thursday 4 September 2014 Submitted by: Chief Nurse – Lisa Allen Prepared by: Patient Safety & Quality Team and James Buschor Status: For monitoring Purpose This report gives an overview of the assurance for patient safety and quality of care at the main providers with whom we contract Basildon and Thurrock University Hospitals Foundation Trust (BTUH) Barking Havering and Redbridge Hospital Trust – Queens hospital North East London Foundation Trust (SWE Community Services) Southend University Hospital Foundation Trust South Essex Partnership Trust Spire Hartswood Nuffield Brentwood NHS 111 East of England Ambulance Trust Background This report continues to be developed to provide assurance about patient safety and quality at the providers from which the CCG commission care. Where possible benchmarking data is used, and this report will be developed further over time. Key issues BTUH BTUH was taken out of special measures after it received a ‘good’ rating from CQC on the 9th June. Services were described as effective, caring, responsive and well-led with seven out of eight areas rated as ‘good’ or ‘outstanding. The hospital is the first in the country to be rated as ‘outstanding’ for its maternity care. Barking Havering and Redbridge Hospital Trust BB CCG has received the first draft of BHRT’s improvement plan which will require further work due to new leadership arrangements. Barking, Havering & Redbridge CCGs have noted that there had been some improvement in performance on the emergency care target, but that it was still below target. -

Conservative Future
1955 Supper Club A dining club of Conservatives from all around the local area— Rochford, Castle Point, Southend East, Southend West, Basildon, etc. Lunches are held on the 1st Thursday of each month (April to October) 3 course meal—£16.00 @ Park View Suite, London Road, Chalkwell SOUTHEND WEST 200 Club CONSERVATIVE This is a fund-raising lottery, which pays out once a year. Each number costs £15, and there is a better chance, at 200/1, of winning ASSOCIATION a prize in the 200 Club than in the national lottery! Conservative Future Chairman: Mrs Judith Suttling E-mail: [email protected] is for all those aged under 30 years of age, to meet together to forward the cause of the Conservative Party. Contact 01702 472391 for details. Political Meetings Political meetings are held from time to time. Contact 01702 472391 Iveagh Hall, 67 Leigh Road, Leigh on Sea, Iveagh Club Essex, SS9 1JW The Iveagh Club licensed premises are at 69 Leigh Road, Leigh on Sea, open during most licensing hours. Tea and Coffee are available, as well as competitively-priced beer, wine and spirits. Telephone: 01702 472391 Sandwiches and other light refreshments are also on offer. Members meet socially for a drink and a chat, and maybe a game of e-mail address: [email protected] cribbage or scrabble. There are occasional musical evenings, and other social events. Annual subscription is £20 single or £35 couple, in addition to membership of SWCA. Please contact 01702 473901. Printed by Southend West Conservative Association, Iveagh Hall, 67 Leigh Road, Leigh on Sea, Essex, SS9 1JW Southend West Conservative Association Iveagh Hall Hire By becoming a member of the Southend West Conservative Association (SWCA), you will be joining the Conservative Party in your Iveagh Hall is available for hire to celebrate any occasion at any area. -

Agenda Template
SOUTHEND-ON-SEA BOROUGH COUNCIL Meeting of Development Control Committee Date: Wednesday, 11th November, 2015 Place: Committee Room 4a - Civic Suite Present: Councillor Crystall (Chair) Councillors Assenheim (Vice-Chair), Arscott*, Ayling, Borton, Butler, Byford, Callaghan, Evans, Folkard, D Garston, McGlone, McMahon, Robinson, Van Looy, Velmurugan and Walker *Substitute in accordance with Council Procedure Rule 31. In Attendance: P Geraghty, C Galforg, D Hermitage, T Row, J Rowley, M Warren and J K Williams Start/End Time: Times Not Specified 422 Apologies for Absence Apologies for absence were received from Councillor R E Hadley (Substitute: Councillor Arscott) 423 Declarations of Interest The following interests were declared at the meeting: (a) All Councillors declared a non-pecuniary interest in respect of application no. 15/01604/BC3 on the basis that the applicant is the current Mayor of the Council; (b) Councillor Borton – 15/01458/FUL – Non-pecuniary interest: Trustee of HARP is a member of the Labour Party; (c) Councillor Evans – 15/01458/FUL – Non-pecuniary interest: Previously involved with HARP (withdrew); (d) Councillor D Garston – 15/01458/FUL – Non-pecuniary interest: Member of Leigh Rotary Club supporting HARP; (e) Councillor Jones – 15/01458/FUL – Pecuniary interest (withdrew); (f) Councillor Jones – 15 01189/FULM – Disqualifying non-pecuniary interest: Executive Councillor for Children & Learning; (g) Councillor McMahon – 15/01458/FUL – Non-pecuniary interest: Co-founder of HARP (although no longer a member), overseer of the homeless integration process and homeless resources on behalf of the Council and trustee is a member of the Labour Party; (h) Councillor Robinson – 15/01458/FUL – Non-pecuniary interest: Trustee of HARP is a member of the Labour Party; (i) Councillor Velmurugan – 15/01274/FUL – Non-pecuniary interest: Daughter owns a property in the neighbourhood; (j) Councillor Walker – 15/01274/FUL – Non-pecuniary interest: A friend lives close to the application site. -

Southend University Hospital NHS Foundation Trust
Southend University Hospital NHS Foundation Trust Evidence appendix Prittlewell Chase Date of inspection visit: Southend-on-Sea 21 November to 14 December 2017 Essex SS0 0RY Date of publication: xxxx> 2018 Tel: 01702 435555 www.southend.nhs.uk This evidence appendix provides the supporting evidence that enabled us to come to our judgements of the quality of service provided by this trust. It is based on a combination of information provided to us by the trust, nationally available data, what we found when we inspected, and information given to us from patients, the public and other organisations. For a summary of our inspection findings, see the inspection report for this trust. Facts and data about this trust Southend University Hospital NHS Foundation Trust (SUHFT) provides acute services from its main Southend Hospital site and outlying satellite clinics across Southend-on-Sea, Castle Point and Rochford. The trust employs over 4,500 staff, serves a population of over 350,000 and has a higher combined percentage population over 65 years of age (20.2%) than the England average (16.95%). The trust provides a comprehensive range of acute services including acute medical and surgical specialties, general medicine, general surgery, orthopaedics, ear, nose and throat, ophthalmology, cancer treatments, renal dialysis, obstetrics and gynaecology and children's services. It is the South Essex surgical centre for uro-oncology and gynae-oncology surgery and has a dedicated stroke unit. Also offered are breast screening, ophthalmology and orthodontic services to the wider South Essex population. The current hospital site opened in 1932 with additional extensions added throughout the existing site, the major extension of the tower block was opened in 1966. -
Southend-On-Sea Borough Council Item
Agenda Southend-on-Sea Borough Council Item Report of the Director of Technical & Environmental Services to Development Control Committee On 17th September 2003 Report prepared by : Planning Officers Report on Planning Applications An Open Agenda Item INTRODUCTION (i) Recommendations in capitals at the end of each report are those of the Director of Technical and Environmental Services, are not the decision of the Committee and are subject to Member consideration (ii) All plans have been considered in the context of the Borough Council's Environmental Charter. An assessment of the environmental implications of development proposals is inherent in the development control process and implicit in the reports. (iii) Reports will not necessarily be dealt with in the order in which they are printed. (iv) The following abbreviations are used in the reports:- AW - Anglia Water plc BLP - Borough Local Plan CAA - Civil Aviation Authority DEFRA - Department of Environment, Food and Rural Affairs DELL - Director of Education & Lifelong Learning DLCAS - Director of Leisure Culture & Amenity Services DSC - Director of Social Care DTLR - Department of Transport Local Government & The Regions EA - Environment Agency EPOA - Essex Planning Officers Association ESRSP - Essex and Southend Replacement Structure Plan ODPM - Office of the Deputy Prime Minister PPG - Planning Policy Guidance Note $jkngfq5d.doc Page 1 of 59 Report No: DTES03/172 - FINAL CONTENTS SOS/02/00540/FUL 16a Preston Road, Westcliff-on-Sea 3 SOS/03/00632/FUL 41 Alexandra Street, Southend -

The Rt Hon Boris JOHNSON Secretary of State for Foreign Affairs Foreign and Commonwealth Office King Charles Street London
EUROPEAN COMMISSION Brussels, 5.10.2016 C(2016) 6292 final PUBLIC VERSION This document is made available for information purposes only. Subject: State aid case no. SA.46361 (2016/N) – United Kingdom - Amendment to the regional aid map 2014-2020 of the United Kingdom for the period 2017-2020 Sir, 1. PROCEDURE (1) On 28 June 2013 the Commission adopted the Guidelines on Regional State Aid for 2014-2020 (hereinafter "RAG")1. On the basis of the RAG the United Kingdom ("UK") authorities notified their regional aid map, which was approved by the Commission on 21 May 2014 for the period from 1 July 2014 until 31 December 20202. (2) Pursuant to point 5.6.2 of the RAG, Member States may notify amendments to their regional aid map in the context of the mid-term review in 2016. The amended regional aid maps will be in force from 1 January 2017 until 31 December 2020. 1 OJ C 209, 23.07.2013, p.1 2 Decision for State aid case SA.38113 – United Kingdom Regional aid map 2014-2020, OJ C 233, 18.07.2014, p.21 The Rt Hon Boris JOHNSON Secretary of State for Foreign Affairs Foreign and Commonwealth Office King Charles Street London SW1A 2AH United Kingdom Commission européenne/Europese Commissie, 1049 Bruxelles/Brussel, BELGIQUE/BELGIË - Tel. +32 22991111 (3) The Commission published on 25 June 2016 a Communication amending Annex I to the RAG (hereinafter, the "Communication")3. In this Communication, the Commission presented up-to-date statistical data to be used as a basis for the mid-term review of the list of regions qualifying for regional aid status pursuant to Article 107(3)(a) TFEU (hereinafter referred to as "'a' areas"). -

Final Recommendations on the Future Electoral Arrangements for Swale in Kent
Final recommendations on the future electoral arrangements for Swale in Kent Report to the Secretary of State for the Environment, Transport and the Regions May 2001 LOCAL GOVERNMENT COMMISSION FOR ENGLAND LOCAL GOVERNMENT COMMISSION FOR ENGLAND This report sets out the Commission’s final recommendations on the electoral arrangements for the borough of Swale in Kent. Members of the Commission are: Professor Malcolm Grant (Chairman) Professor Michael Clarke CBE (Deputy Chairman) Peter Brokenshire Kru Desai Pamela Gordon Robin Gray Robert Hughes CBE Barbara Stephens (Chief Executive) © Crown Copyright 2001 Applications for reproduction should be made to: Her Majesty’s Stationery Office Copyright Unit. The mapping in this report is reproduced from OS mapping by the Local Government Commission for England with the permission of the Controller of Her Majesty’s Stationery Office, © Crown Copyright. Unauthorised reproduction infringes Crown Copyright and may lead to prosecution or civil proceedings. Licence Number: GD 03114G. This report is printed on recycled paper. Report no.: 211 ii LOCAL GOVERNMENT COMMISSION FOR ENGLAND CONTENTS page LETTER TO THE SECRETARY OF STATE v SUMMARY vii 1 INTRODUCTION 1 2 CURRENT ELECTORAL ARRANGEMENTS 3 3 DRAFT RECOMMENDATIONS 7 4 RESPONSES TO CONSULTATION 9 5 ANALYSIS AND FINAL RECOMMENDATIONS 13 6 NEXT STEPS 39 APPENDICES A Final Recommendations for Swale: Detailed Mapping 41 B Draft Recommendations for Swale (October 2000) 45 C Code of Practice on Written Consultation 47 A large map illustrating the proposed ward boundaries for Faversham and Sittingbourne is inserted inside the back cover of the report. LOCAL GOVERNMENT COMMISSION FOR ENGLAND iii iv LOCAL GOVERNMENT COMMISSION FOR ENGLAND Local Government Commission for England 9 May 2001 Dear Secretary of State On 9 May 2000 the Commission began a periodic electoral review of Swale under the Local Government Act 1992.