Forecasting Hospital Emergency Department Visits For
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

BOH-Agenda-Aug-11-2021.Pdf
Board of Health for Peterborough Public Health AGENDA Board of Health Meeting Wednesday, August 11, 2021 – 5:00 p.m. 1. Call to Order Mayor Andy Mitchell, Chair 1.1. Welcome and Opening Statement Land Acknowledgement We respectfully acknowledge that Peterborough Public Health is located on the Treaty 20 Michi Saagiig territory and in the traditional territory of the Michi Saagiig and Chippewa Nations, collectively known as the Williams Treaties First Nations, which include: Curve Lake, Hiawatha, Alderville, Scugog Island, Rama, Beausoleil, and Georgina Island First Nations. Peterborough Public Health respectfully acknowledges that the Williams Treaties First Nations are the stewards and caretakers of these lands and waters in perpetuity, and that they continue to maintain this responsibility to ensure their health and integrity for generations to come. We are all treaty people. Recognition of Indigenous Cultures We recognize also the unique history, culture and traditions of the many Indigenous Peoples with whom we share this time and space. We give thanks to the Métis, the Inuit, and the many other First Nations people for their contributions as we strengthen ties, serve their communities and responsibly honour all our relations. 2. Confirmation of the Agenda 3. Declaration of Pecuniary Interest 4. Consent Items to be Considered Separately Board Members: Please identify which items you wish to consider separately from section 10 and advise the Chair when requested. For your convenience, circle the item(s) using the following list: 10.2 a b c d e 5. Delegations and Presentations 6. Board Chair Report BOH Agenda Aug 11/21 - Page 1 of 29 7. -

PHPC CPD Symposium Winnipeg, April 26-27, 2020
PHPC CPD Symposium Winnipeg, April 26-27, 2020 Day 1: Sunday April 26th Day 2: Monday April 27th 07:30 Breakfast 08:30 Breakfast Public Health Physicians of Canada Plenary 08:00 09:00 Annual General Meeting A Dialogue with the Public Health Laboratory Network Coffee Break AM Break 8:50 10:30 Innovation Plenary Oral Abstract Presentations Artificial Intelligence - Potential or Peril? 1. The case for and against use of artificial intelligence to promote health equity: 9:00 [Dr. David Buckeridge, McGIll Univ.] learning from efforts to tackle the legacy of silicosis and tuberculosis in south Dr. Kamran Khan, Founder & CEO, BlueDot African miners. Dr. Annalee Yassi, Univ of British Columbia Moderator: Dr. Barry Pakes, University of Toronto 2. Application of artificial intelligence in local public health: implications from a qualitative study – Dr. Jason Morgenstern, McMaster University Break 10:30 11:00 3. A Community Charting System for Public Health. Dr. Andrew Gray & Dr. Rakel Kling, Workshop Northern Health Disrupting the Color-coded Labour Market: In search of a population-centered method of practice for public health physicians. 4. 11:00 Public Health Sector Implications Dr. Sudit Ranade, Lambton Public Health and Amardeep Thind & Judith Belle Brown Dr. Fareen Karachiwalla, York Region Public Health, 5. Lethal But Legal: What an we learn from Nicholas Freudenberg about Corporate Sume Ndumbe-Eyoh (TBC) Malfeasance – Dr. Michael Rachlis, Dalla Lana School of Public Health, Univ of Toronto 12:00 Networking Lunch 12:10 Networking Lunch Outbreak SIMULATION Exercise! DEBATE 13:00 Lead by Dr. Kieran Moore, Kingston, KFL&A Public Health unit "Be it resolved that PHPM practitioners should set aside our Section 3 MOC differences and collaborate more closely with primary care and the Break 14:30 13:30 Panel Discussion broader health care system to improve health." [Integration vs Public Health on Crystal Meth: encroachment - budget, priorities, knowledge] Debaters: Dr. -

Syndromic Surveillance Workshop Agenda
Workshop on Syndromic Surveillance of Health and Climate- Related Impacts: Lessons Learned from the use of Syndromic Surveillance Systems for Health and Climate Effects to Support Decision-Making Nunc in nunc quisMarch leo consectetuer.17 & 18, 2014 Kingston, Frontenac and Lennox & Addington (KFL&A) Public Health An exciting initiative bringing together 221 Portsmouth Ave Kingston, Ontario public health practitioners, Canada epidemiologists, emergency The workshop, hosted by KFL&A Public Health in partnership management officials, with national and international health authorities, is an opportunity for public health professionals and emergency environmental health management officials to discuss lessons learned from the use of experts, and others to syndromic surveillance for climate-related health outcomes, and share best practices to guide the future use of such tools and capabilities for for the use of monitoring environmental causes of health impacts. syndromic The event will incorporate sessions on the use of syndromic surveillance systems surveillance systems in the Canadian, U.S., and international for health and climate contexts, as well as a case study on the 2015 Pan American effects Games in Ontario. The case study will explore how public health can use syndromic surveillance for mass gathering events. The workshop will be an opportunity to consult with participants and collect input through a breakout session aimed at the preparation of a guidance document for the use of syndromic surveillance systems for climate-related impacts. Supported by the Department of Family Medicine, Public Health and Preventive Medicine Residency Program Workshop on Syndromic Surveillance of Health and Climate-Related Impacts: Lessons Learned from the use of Syndromic Surveillance Systems for Health and Climate Effects to Support Decision-Making Kingston, Frontenac and Lennox & Addington Public Health 221 Portsmouth Avenue, Kingston, ON March 17 & 18, 2014 AGENDA Monday, March 17 – Auditoriums A&B 9:00-9:30 Registration 9:30-9:45 Welcome – Dr. -
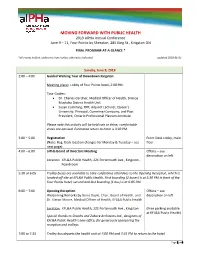
MOVING FORWARD with PUBLIC HEALTH 2019 Alpha Annual Conference June 9 – 11, Four Points by Sheraton, 285 King St., Kingston ON
MOVING FORWARD WITH PUBLIC HEALTH 2019 alPHa Annual Conference June 9 – 11, Four Points by Sheraton, 285 King St., Kingston ON FINAL PROGRAM-AT-A-GLANCE * *all events held at conference hotel unless otherwise indicated updated 2019-06-05 Sunday, June 9, 2019 2:00 – 4:00 Guided Walking Tour of Downtown Kingston Meeting place: Lobby of Four Points hotel, 2:00 PM. Tour Guides: • Dr. Charles Gardner, Medical Officer of Health, Simcoe Muskoka District Health Unit • Susan Cumming, RPP, Adjunct Lecturer, Queen’s University; Principal, Cumming+Company; and Past President, Ontario Professional Planners Institute Please note this activity will be held rain or shine; comfortable shoes are advised. Estimated return to hotel is 3:30 PM. 2:00 – 5:00 Registration Front Desk Lobby, main (Note: Reg. Desk location changes for Monday & Tuesday – see floor next page) 4:00 – 6:00 alPHa Board of Directors Meeting Offsite – see description on left Location: KFL&A Public Health, 221 Portsmouth Ave., Kingston - Boardroom 5:30 or 6:05 Trolley buses are available to take conference attendees to the Opening Reception, which is located off-site at KFL&A Public Health. First boarding (2 buses) is at 5:30 PM in front of the Four Points hotel; second and last boarding (1 bus) is at 6:05 PM. 6:00 – 7:00 Opening Reception Offsite – see Welcoming Remarks by Denis Doyle, Chair, Board of Health, and description on left Dr. Kieran Moore, Medical Officer of Health, KFL&A Public Health Location: KFL&A Public Health, 221 Portsmouth Ave., Kingston (Free parking available at KFL&A Public Health) Special thanks to Shoalts and Zaback Architects Ltd., designers of KFL&A Public Health’s new office, for generously sponsoring the reception and trolleys. -

Next Steps in COVID-19 Response in Long-Term Care and Retirement Homes September 14, 2020 12:00 – 1:00 P.M
Webinar Series: Next Steps in COVID-19 Response in Long-Term Care and Retirement Homes September 14, 2020 12:00 – 1:00 p.m. ET cfhi-fcass.ca | @cfhi_fcass Tanya MacDonald, Dr. Kieran Moore, Medical Theresa Miller Program Director, Officer of Health, Kingston, Providence Manor Resident CFHI Frontenac, Lennox & Addington (KFL&A) Public Health Krystal Mack Dr. David Barber Dr. Pierre Robichaud 22 • Learn from the approach used in Kingston to prepare and prevent outbreaks in LTC facilities SESSION • Offer concrete strategies for organizations to prepare for future OBJECTIVES outbreaks • Share next steps to participate in the LTC+: Acting on Pandemic Learning Together program cfhi-fcass.ca | @cfhi_fcass 3 COVID and long-term care and retirement homes: the Kieran Moore, MD, KFL&A experience CCFP(EM), FCFP, MPH, DTM&H, FRCPC Medical Officer of Health, CEO KFL&A Public Health Professor of Emergency September 14, 2020 Medicine, Queen’s University Program Director, Public Health and Preventive Medicine, Queen’s University Healthy People, Healthy Places Overview • COVID in LTC homes • Ontario’s approach • KFL&A: background • KFL&A pandemic approach • Next steps • Key messages 5 Government of Canada COVID-19 Situational Awareness Dashboard 6 How Canadians contract SARS-CoV-2 GIS Hub is provided by Esri Canada available here 7 Number of COVID-19 Affected Long-Term Care Homes across Jurisdictions in Canada (shown as a percentage of total) Canada 5801 1125 Quebec 2215 568 Ontario 1396 436 New Brunswick 468 2 Saskatchewan 402 3 British Columbia 392 39 -

Sunday April 26
PHPC 2020 CPD Symposium: Schedule April 26-27, 2020 Delta Hotels Winnipeg, Winnipeg, MB Updated February 20, 2020 Sunday April 26 Time Session type Topic 07:30-08:00 Breakfast AGM PHPC Annual General Meeting 08:00-08:50 08:50-09:00 Break Plenary Innovation - Artificial Intelligence 09:00-10:30 Speakers: Dr. Kamren Khan, Founder & CEO, BlueDot (TBC) Moderator: Dr. Barry Pakes , University of Toronto 10:30-11:00 AM Break Workshop Disrupting the color-coded labour market - implications for the public health sector 11:00-12:00 Dr. Fareen Karachiwalla, York Region Public Health, Sume Ndumbe -Eyoh (TBC) 12:00-13:00 Lunch Simulation Hep A foodborne outbreak Lead by Dr. Kieran Moore, Kingston, Frontenac, Lennox and 13:00-14:30 Addington (KFL&A) Public Health unit Section 3 MOC 14:30-15:00 PM Break Panel Discussion Crystal Meth Rural, Remote, Northern Public Health Network & Urban Public 15:00-16:30 Health Network Session Speakers: TBC PHPC Annual Society Dinner & Awards 19:30-22:30 Canadian Museum for Human Rights ~ ERA Bistro (guided museum tour – registration coming soon!) PHPC 2020 CPD Symposium: Schedule April 26-27, 2020 Delta Hotels Winnipeg, Winnipeg, MB Updated February 20, 2020 Monday April 27, 2020 08:30-09:00 Breakfast Plenary Public Health Laboratory Network 09:00-10:30 Moderator: Dr. Barry Pakes 10:30-11:00 AM Break Oral Abstract − The case for and against use of artificial intelligence to Presentations promote health equity: learning from efforts to tackle the (presentation legacy of silicosis and tuberculosis in south African miners order may – Dr. -

COVID-19 Community of Practice for Ontario Family Physicians
COVID-19 Community of Practice for Ontario Family Physicians March 12, 2021 Changing the Way We Work Dr. Kieran Moore The COVID-19 Vaccine: Newly approved Dr. Daniel Warshafsky Dr. Liz Muggah vaccines, public health collaboration, and more Dr. David Kaplan The COVID-19 Vaccine: Newly approved vaccines, public health collaboration, and more Moderator: Dr. Tara Kiran Fidani Chair, Improvement and Innovation Department of Family and Community Medicine, University of Toronto Panelists: • Dr. Kieran Moore, Kingston, ON • Dr. Daniel Warshafsky, Toronto, ON • Dr. Liz Muggah, Ottawa, ON • Dr. David Kaplan, Toronto, ON This one-credit-per-hour Group Learning program has been certified by the College of Family Physicians of Canada and the Ontario Chapter for up to 1 Mainpro+ credits. The COVID-19 Community of Practice for Ontario Family Physician includes a series of planned webinars. Each session is worth 1 Mainpro+ credits, for up to a total of 18 credits. 2 Land Acknowledgement We acknowledge that the lands on which we are hosting this meeting include the traditional territories of many nations. The OCFP and DFCM recognize that the many injustices experienced by the Indigenous Peoples of what we now call Canada continue to affect their health and well-being. The OCFP and DFCM respect that Indigenous people have rich cultural and traditional practices that have been known to improve health outcomes. I invite all of us to reflect on the territories you are calling in from as we commit ourselves to gaining knowledge; forging a new, culturally safe relationship; and contributing to reconciliation. 3 https://www.cmaj.ca/content/early/2021/02/23/cmaj.210112 Changing the way we work A community of practice for family physicians during COVID-19 At the conclusion of this series participants will be able to: • Identify the current best practices for delivery of primary care within the context of COVID-19 and how to incorporate into practice. -

35Th Annual Educational Conference
2015 CLEAR’s Annual Educational Conference Boston, Massachusetts September 17-19, 2015 E-Mail: [email protected] Visit CLEAR on the web: Canada www.clearhq.org Betty Anderson Deputy Complaints Director Joy Aaron College & Association of Registered Nurses Deputy Director of Alberta Maryland Board of PT Examiners E-Mail: [email protected] E-Mail: [email protected] Canada United States James Anliot Bob Albert Director, Healthcare Compliance Services Chief Technoloy Officer Affiliated Monitors, Inc. National Dental Examining E-Mail: [email protected] Council on Board of Canada United States Phone: 613-236-5912 x223 Licensure, E-Mail: [email protected] Jacki Arcelin Enforcement and Canada Licensing and Enforcement Manager Colorado Department of Regulatory Regulation Ben Albritton Agencies - Division of Registrations Assitant Attorney General Phone: 303-894-3005 Alabama Board of Licensure for E-Mail: [email protected] Professional Engineers & Land Surveyors United States E-Mail: [email protected] th United States Sten Ardal 35 Annual CEO Mary Alexander Touchstone Institute CEO E-Mail: [email protected] Infusion Nurses Certification Corporation Educational Canada E-Mail: [email protected] Conference United States Karine Arsenault New Brunswick Association of Dietitians Bruce Allain E-Mail: [email protected] Promoting Regulatory American Association of Nurse Canada Anesthestists Excellence E-Mail: [email protected] Kirsten Ash United States Executive Assistant Alberta College of Occupational -

Extreme Heat Events Guidelines: Technical Guide for Health Care Workers Extreme Heat Events Guidelines: Technical Guide for Health Care Workers
Extreme Heat Events Guidelines: Technical Guide for Health Care Workers Extreme Heat Events Guidelines: Technical Guide for Health Care Workers Prepared by: Water, Air and Climate Change Bureau Healthy Environments and Consumer Safety Branch Health Canada is the federal department responsible for helping the people of Canada maintain and improve their health. We assess the safety of drugs and many consumer products, help improve the safety of food, and provide information to Canadians to help them make healthy decisions. We provide health services to First Na- tions people and to Inuit communities. We work with the provinces to ensure our health care system serves the needs of Canadians. Published by authority of the Minister of Health. Extreme Heat Events Guidelines: Technical Guide for Health Care Workers is available on Internet at the following address: www.healthcanada.gc.ca Également disponible en français sous le titre : Lignes directrices à l’intention des travailleurs de la santé pendant les périodes de chaleur accablante : Un guide technique This publication can be made available in a variety of formats. For further information or to obtain additional copies, please contact: Publications Health Canada Ottawa, Ontario K1A 0K9 Tel.: 613-954-5995 Fax: 613-941-5366 Email: [email protected] © Her Majesty the Queen in Right of Canada, represented by the Minister of Health, 2011 This publication may be reproduced without permission provided the source is fully acknowledged. HC Pub.: 110055 Cat.: H128-1/11-642E ISBN: 978-1-100-18172-1 Acknowledgements Health Canada gratefully acknowledges the contribution of the following people in reviewing chapters. -

Board of Health Agenda Package
City of Hamilton BOARD OF HEALTH Meeting #: 19-003 Date: March 18, 2019 Time: 1:30 p.m. Location: Council Chambers, Hamilton City Hall 71 Main Street West Loren Kolar, Legislative Coordinator (905) 546-2424 ext. 2604 1. CEREMONIAL ACTIVITIES 2. APPROVAL OF AGENDA (Added Items, if applicable, will be noted with *) 3. DECLARATIONS OF INTEREST 4. APPROVAL OF MINUTES OF PREVIOUS MEETING 4.1 February 22, 2019 5. COMMUNICATIONS 5.1 Correspondence from the Regional Municipality of Durham respecting their Cannabis Use in Public Places Resolution Recommendation: Be received. 5.2 Correspondence from the Windsor Essex County Health Unit respecting the Smoke Free Ontario Act, 2017 and Cannabis Legislation Recommendation: Be received. 5.3 Correspondence from the Windsor Essex County Health Unit respecting Ontario's Basic Income Pilot Recommendation: Be received. Page 2 of 107 5.4 Correspondence from the Windsor Essex County Health Unit respecting an Endorsement for Mandatory Food Literacy Curricula in Ontario Schools Recommendation: Be received. 5.5 Correspondence from the Windsor Essex County Health Unit respecting Funding for the Healthy Babies, Healthy Children (HBHC) Program Recommendation: Be received. 5.6 Correspondence from the Windsor Essex County Health Unit respecting an Endorsement of a Universal Student Nutrition Program 2018 Recommendation: Be received 5.7 Correspondence from the Simcoe Muskoka District Health Unit respecting the Public and Environmental Health Implications of Bill 66, Restoring Ontario's Competitiveness Act, 2018 Recommendation: Be received. 5.8 Correspondence from the North Bay Parry Sound District Health Unit respecting Food Insecurity and Bill 60, an Act to Amend the Ministry of Community and Social Services Act to Establish the Social Assistance Research Commission. -
FDA Grants Class II Medical Device Clearance for Aerus Medical Guardian with Activepure Technology
HOME MAIL NEWS SPORTS FINANCE CELEBRITY STYLE MOVIES WEATHER ANSWERS MOBILE Sign in Mail News Coronavirus Originals Canada World Business Entertainment Sports Science & Tech Weather . GET YOUR €100 BONUS Welcome bonus www.spielerschutz.eu Gambling can become addictive. MGA/B2C/114/2005 Bonus conditions apply. ACCESSWIRE FDA Grants Class II Medical Device Clearance for Aerus Medical Guardian with ActivePure Technology June 30, 2020 Continuous, Active Air Purifier Uses NASA-inspired ActivePure Technology DALLAS, TX / ACCESSWIRE / June 30, 2020 / Aerus, committed to providing cutting-edge technologies to create the healthiest indoor environments around the world, announced today that it received Class II Medical Device clearance from the U.S. Food and Drug Administration (FDA) for the Aerus Medical Guardian with ActivePure Technology, the first active air purifier for health care. TRENDING ActivePure is the most powerful surface and air-purification technology ever discovered. It can operate safely in occupied spaces and prevents recontamination in real time. No one has lost quite like Donald Trump 1. in nearly 150 years Sask. restricting most private gatherings 2. to household members only starting Thursday At least 28 people killed in extremist 3. attack in Niger After 60 years, East Jerusalem 4. Palestinians face eviction under Israeli settler rulings After the White House, Trump faces 5. uncertain future and legal threats The Aerus Medical Guardian with ActivePure Technology, a free-standing, portable unit intended for use in professional health-care environments, is a 24/7 airborne contaminant reduction solution. The unit is the first of its kind, using NASA-inspired ActivePure Technology to purify the air continuously and actively without the use of ozone. -

Lyme Disease in Canada
LYME DISEASE IN CANADA A FEDERAL FRAMEWORK Également disponible en français sous le titre : LA MALADIE DE LYME AU CANADA - CADRE FÉDÉRAL This publication can be made available in alternative formats upon request. © Her Majesty the Queen in Right of Canada, as represented by the Minister of Health, 2017 Publication date: May 2017 This publication may be reproduced for personal or internal use only without permission provided the source is fully acknowledged. Cat.: HP40-180/2017E-PDF ISBN: 978-0-660-08445-9 Pub.: 170032 LYME DISEASE IN CANADA - A FEDERAL FRAMEWORK > 2 MESSAGE FROM THE CHIEF PUBLIC HEALTH OFFICER Lyme disease is an emerging infectious disease in many parts of Canada, and the Government of Canada recognizes the impact that it has on Canadians and their families. Efforts to prevent and control Lyme disease are being made by a variety of stakeholders, but more can and should be done. As the interim Chief Public Health Officer, I am concerned about the challenges associated with Lyme disease in Canada. I am grateful to health care providers, patients and their families who took the time to share their experiences. I heard both from patients who have been diagnosed with Lyme disease, as well as others who have experienced various chronic symptoms consistent with Lyme disease or similar ailments. Overwhelmingly, we have heard that patients and the health professionals that care for them wish to see a call to action. As such, this framework includes an Action Plan (Appendix 1), which includes the establishment of a Lyme disease research network. This is an emerging disease and we don’t have all of the answers.