Use of Fentanyl, Butyrfentanyl and Furanylfentanyl As Discussed on Polish Online Forums Devoted to ‘Designer Drugs’
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Review of Synthetic Fentanyl Metabolism and the Metabolism of Select Synthetic Fentanyl Analogues
A review of synthetic fentanyl metabolism and the metabolism of select synthetic fentanyl analogues Gerard Lee A thesis submitted for the completion of a degree in Master of Forensic Science (Professional Practice) in The School of Veterinary and Life Sciences Murdoch University Supervisors: Associate Professor James Speers (Murdoch) Associate Professor Bob Mead (Murdoch) Semester 1, 2019 i Declaration I declare that this thesis does not contain any material submitted previously for the award of any other degree or diploma at any university or other tertiary institution. Furthermore, to the best of my knowledge, it does not contain any material previously published or written by another individual, except where due reference has been made in the text. Finally, I declare that all reported experimentations performed in this research were carried out by myself, except that any contribution by others, with whom I have worked is explicitly acknowledged. ii Acknowledgements I would like to thank my supervisor Bob Mead for his time guiding me and providing feedback on this endeavour. He has been a great help providing insights and advice from when I started university at Murdoch until now for which I am extremely grateful. To James Speers, thank you for helping me find a direction for this project when I started out. And finally, to my family and friends for their encouragement and support. iii Table of Contents Title page. ...............................................................................................................................I -

18 December 2020 – to Date)
(18 December 2020 – to date) MEDICINES AND RELATED SUBSTANCES ACT 101 OF 1965 (Gazette No. 1171, Notice No. 1002 dated 7 July 1965. Commencement date: 1 April 1966 [Proc. No. 94, Gazette No. 1413] SCHEDULES Government Notice 935 in Government Gazette 31387 dated 5 September 2008. Commencement date: 5 September 2008. As amended by: Government Notice R1230 in Government Gazette 32838 dated 31 December 2009. Commencement date: 31 December 2009. Government Notice R227 in Government Gazette 35149 dated 15 March 2012. Commencement date: 15 March 2012. Government Notice R674 in Government Gazette 36827 dated 13 September 2013. Commencement date: 13 September 2013. Government Notice R690 in Government Gazette 36850 dated 20 September 2013. Commencement date: 20 September 2013. Government Notice R104 in Government Gazette 37318 dated 11 February 2014. Commencement date: 11 February 2014. Government Notice R352 in Government Gazette 37622 dated 8 May 2014. Commencement date: 8 May 2014. Government Notice R234 in Government Gazette 38586 dated 20 March 2015. Commencement date: 20 March 2015. Government Notice 254 in Government Gazette 39815 dated 15 March 2016. Commencement date: 15 March 2016. Government Notice 620 in Government Gazette 40041 dated 3 June 2016. Commencement date: 3 June 2016. Prepared by: Page 2 of 199 Government Notice 748 in Government Gazette 41009 dated 28 July 2017. Commencement date: 28 July 2017. Government Notice 1261 in Government Gazette 41256 dated 17 November 2017. Commencement date: 17 November 2017. Government Notice R1098 in Government Gazette 41971 dated 12 October 2018. Commencement date: 12 October 2018. Government Notice R1262 in Government Gazette 42052 dated 23 November 2018. -

Analysis of Synthetic Opioids in Postmortem Blood, Vitreous Humor, and Brain Tissue
City University of New York (CUNY) CUNY Academic Works Student Theses John Jay College of Criminal Justice Fall 12-2018 Analysis of synthetic opioids in postmortem blood, vitreous humor, and brain tissue Rachel K. Chesser CUNY John Jay College, [email protected] How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/jj_etds/88 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] i Analysis of synthetic opioids in postmortem blood, vitreous humor, and brain tissue A thesis presented in partial fulfillment of the requirements for the degree of Master of Science in Forensic Science John Jay College of Criminal Justice City University of New York Rachel Chesser December 2018 ii Analysis of synthetic opioids in postmortem blood, vitreous humor, and brain tissue Rachel Chesser This thesis has been presented to and accepted by the Office of Graduate Studies, John Jay College of Criminal Justice in partial fulfillment of the requirements for the degree of Master of Science in Forensic Science. Thesis Committee Thesis Advisor: Dr. Marta Concheiro-Guisan Second Reader: Dr. Gail Cooper External Reader: Dr. Luke N. Rodda iii Acknowledgements I would like to express my sincerest gratitude to Dr. Marta Concheiro, my advisor, for providing her guidance towards my thesis research and providing me with a strong background on forensic toxicology that allowed me to complete my project. She has been so patient and helpful with me in putting my thesis together and helping me make sense of it for parts I did not understand. -

Recommended Methods for the Identification and Analysis of Fentanyl and Its Analogues in Biological Specimens
Recommended methods for the Identification and Analysis of Fentanyl and its Analogues in Biological Specimens MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES Laboratory and Scientific Section UNITED NATIONS OFFICE ON DRUGS AND CRIME Vienna Recommended Methods for the Identification and Analysis of Fentanyl and its Analogues in Biological Specimens MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES UNITED NATIONS Vienna, 2017 Note Operating and experimental conditions are reproduced from the original reference materials, including unpublished methods, validated and used in selected national laboratories as per the list of references. A number of alternative conditions and substitution of named commercial products may provide comparable results in many cases. However, any modification has to be validated before it is integrated into laboratory routines. ST/NAR/53 Original language: English © United Nations, November 2017. All rights reserved. The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. Mention of names of firms and commercial products does not imply the endorse- ment of the United Nations. This publication has not been formally edited. Publishing production: English, Publishing and Library Section, United Nations Office at Vienna. Acknowledgements The Laboratory and Scientific Section of the UNODC (LSS, headed by Dr. Justice Tettey) wishes to express its appreciation and thanks to Dr. Barry Logan, Center for Forensic Science Research and Education, at the Fredric Rieders Family Founda- tion and NMS Labs, United States; Amanda L.A. -

Understanding and Challenging the Drugs: Chemistry and Toxicology
UNDERSTANDING AND CHALLENGING THE DRUGS: CHEMISTRY AND TOXICOLOGY Presenter: • Dr. Jasmine Drake, Graduate Program Director and Assistant Professor, Administration of Justice Department, Barbara Jordan-Mickey Leland School of Public Affairs, Texas Southern University NACDL Training Defending Drug Overdose Homicides in Pennsylvania Penn State Harrisburg, Middletown, PA November 6th, 2019 11:30- 12:45 p.m. Understanding & Challenging the Drugs: Chemistry & Toxicology Dr. Jasmine Drake, Forensic Science Learning Laboratory, Texas Southern University I. Opioid Drug Classifications A. Types of Opioids B. Classic vs. Synthetic C. Toxicology of Opioids 1) How opioids interact with the body 2) Addiction (psychological vs. physiological II. New Classes of Drugs A. Emerging Threats B. Potency III. National Trends in Opioid Overdose Deaths in the U.S. A. Based on State B. Ethnicity C. Drug-Type (prescription vs. fentanyl vs. heroin) IV. Trends of Opioid Overdose Deaths in Philadelphia A. Based on Ethnicity B. Drug Type (prescription vs. fentanyl vs. heroin) V. Legal Considerations to the Opioid Epidemic A. Punitive Measures vs. Rehabilitative Treatment B. Progressive Jurisdictions Nationwide C. New Legal Measures in Philadelphia VI. Toxicology Reports A. What’s in the report? B. Key Aspects of the Tox Report C. Terminology D. Evaluating and Interpreting the data? E. Questions and considerations. VII. Conclusion and Discussion A. Case Specific Examples B. Sample Toxicology Reports The Opioid Epidemic: What labs have to do with it? Ewa King, Ph.D. Associate Director of Health RIDOH State Health Laboratories Analysis. Answers. Action. www.aphl.org Overview • Overdose trends • Opioids and their effects • Analytical testing approaches • Toxicology laboratories Analysis. Answers. Action. -
Comprehensive Multi-Analytical Screening Of
COMPREHENSIVE MULTI-ANALYTICAL SCREENING OF DRUGS OF ABUSE, INCLUDING NEW PSYCHOACTIVE SUBSTANCES, IN URINE WITH BIOCHIP ARRAYS APPLIED TO THE EVIDENCE ANALYSER Darragh J., Keery L., Keenan R., Stevenson C., Norney G., Benchikh M.E., Rodríguez M.L., McConnell R. I., FitzGerald S.P. Randox Toxicology Ltd., Crumlin, United Kingdom e-mail: [email protected] Introduction Biochip array technology allows the simultaneous detection of multiple drugs from a single undivided sample, which This study summarises the analytical performance of three different biochip arrays applied to the screening of increases the screening capacity and the result output per sample. Polydrug consumption can be detected and by acetylfentanyl, AH-7921, amphetamine, barbiturates, benzodiazepines (including etizolam and clonazepam), incorporating new immunoassays on the biochip surface, this technology has the capacity to adapt to the new trends benzoylecgonine/cocaine, benzylpiperazines, buprenorphine, cannabinoids, carfentanil, dextromethorphan, fentanyl, in the drug market. furanylfentanyl, meprobamate, mescaline, methamphetamine, methadone, mitragynine, MT-45, naloxone, ocfentanyl, opioids, opiates, oxycodone, phencyclidine, phenylpiperazines, salvinorin, sufentanil, synthetic cannabinoids (JWH-018, UR-144, AB-PINACA, AB-CHMINACA), synthetic cathinones [mephedrone, methcathinone, alpha- pyrrolidinopentiophenone (alpha-PVP)], tramadol, tricyclic antidepressants, U-47700, W-19, zolpidem. Methodology Three different biochip arrays were used (DOA ULTRA, -

16.19.20 Nmac 1 Title 16 Occupational And
TITLE 16 OCCUPATIONAL AND PROFESSIONAL LICENSING CHAPTER 19 PHARMACISTS PART 20 CONTROLLED SUBSTANCES 16.19.20.1 ISSUING AGENCY: Regulation and Licensing Department - Board of Pharmacy. [16.19.20.1 NMAC - Rp 16.19.20.1 NMAC, 06-26-2018] 16.19.20.2 SCOPE: All persons or entities that manufacture, distribute, dispense, administer, prescribe, deliver, analyze, or conduct research using controlled substances. [16.19.20.2 NMAC - Rp 16.19.20.2 NMAC, 06-26-2018] 16.19.20.3 STATUTORY AUTHORITY: Section 30-31-11 of the Controlled Substances Act, 30-31-1 through 30-31-42 NMSA 1978, authorizes the board of pharmacy to promulgate regulations and charge reasonable fees for the registration and control of the manufacture, distribution and dispensing of controlled substances. [16.19.20.3 NMAC - Rp 16.19.20.3 NMAC, 06-26-2018] 16.19.20.4 DURATION: Permanent. [16.19.20.4 NMAC - Rp 16.19.20.4 NMAC, 06-26-2018] 16.19.20.5 EFFECTIVE DATE: June 26, 2018, unless a different date is cited at the end of a section. [16.19.20.5 NMAC - Rp 16.19.20.5 NMAC, 06-26-2018] 16.19.20.6 OBJECTIVE: The objective of Part 20 of Chapter 19 is to protect the public health and welfare of the citizens of New Mexico by controlling and monitoring access to controlled substances and to give notice of the board’s designation of particular substances as controlled substances. [16.19.20.6 NMAC - Rp 16.19.20.6 NMAC, 06-26-2018] 16.19.20.7 DEFINITIONS: [RESERVED] [16.19.20.7 NMAC - Rp 16.19.20.7 NMAC, 06-26-2018] 16.19.20.8 REGISTRATION REQUIREMENTS: Persons required to register: A. -

The International Drug Control Conventions
ST/CND/1/Add.1/Rev.3 The International Drug Control Conventions Schedules of the Single Convention on Narcotic Drugs of 1961 as amended by the 1972 Protocol, as at 22 April 2017 UNITED NATIONS New York, 2017 ST/CND/1/Add.1/Rev.3 © United Nations, 2017. All rights reserved, worldwide. Schedules of the Single Convention on Narcotic Drugs of 1961 as amended by the 1972 Protocol, as at 22 April 2017 List of drugs included in Schedule I Acetorphine 3-O-Acetyltetrahydro-7α-(1-hydroxy-1-methylbutyl)- 6,14-endo-ethenooripavine Acetyl-alpha-methylfentanyl N-[1-(α-Methylphenethyl)-4-piperidyl]acetanilide Acetylfentanyl N-phenyl-N-[1-(2-phenylethyl)-4-piperidinyl]acetamide Acetylmethadol 3-Acetoxy-6-dimethylamino-4,4-diphenylheptane AH-7921 3,4-dichloro-N-{[1- (dimethylamino)cyclohexyl]methyl}benzamide Alfentanil N-[1-[2-(4-Ethyl-4,5-dihydro-5-oxo-1H-tetrazol-1-yl) ethyl]-4-(methoxymethyl)-4-piperidinyl]-N- phenylpropanamide Allylprodine 3-Allyl-1-methyl-4-phenyl-4-propionoxypiperidine Alphacetylmethadol α-3-Acetoxy-6-dimethylamino-4,4-diphenylheptane Alphameprodine α-3-Ethyl-1-methyl-4-phenyl-4-propionoxypiperidine Alphamethadol α-6-Dimethylamino-4,4-diphenyl-3-heptanol alpha-Methylfentanyl N-[1-(α-Methylphenethyl)-4-piperidyl]propionanilide alpha-Methylthiofentanyl N-[1-[1-Methyl-2-(2-thienyl)ethyl]-4-piperidyl] propionanilide Alphaprodine α-l,3-Dimethyl-4-phenyl-4-propionoxypiperidine Anileridine 1-p-Aminophenethyl-4-phenylpiperidine-4-carboxylic acid ethyl ester Benzethidine 1-(2-Benzyloxyethyl)-4-phenylpiperidine-4-carboxylic acid ethyl ester -

Supplement 1: Additional Tables and Figures
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Global Health Supplement 1: Additional tables and figures Box S1: Substances included and excluded from the International Narcotic Control Board (INCB) data on narcotic consumption, in alphabetical order. Opioids included in the opioid consumption calculation: 1. (+)-cis-3-methylfental 35. Bezitramide 2. 3-Acetylmorphine 36. Butyrfentanyl 3. 3-Methylfentanyl 37. Carfentanil 4. 3-Methylthiofentanyl 38. Carfentanyl 5. 3-Monoacetylmorphine 39. Clonitazene 6. 4-Fluoroisobutyrfentanyl 40. Codeine 7. 6-Acetylmorphine 41. Codeine-6GLUC 8. 6-Monoacetylmorphine 42. Codeine-6-glucuronide 9. Acetorphine 43. Codeine-Methyl 10. Acetyl-alpha-methylfentanyl 44. Codeine-N-oxide 11. Acetyldihydrocodeine 45. Codoxime 12. Acetylfentanyl 46. Conc. of poppy straw (C) ACA 13. Acetylmethadol 47. Conc. of poppy straw (C) AMA 14. Acetylmorphine 48. Conc. of poppy straw (C) AOA 15. Acrylfentanyl 49. Conc. of poppy straw (C) ATA 16. AH-7921 50. Conc. of poppy straw (C) GW 17. Alfentanil 51. Conc. of poppy straw (M) ACA 18. Allylprodine 52. Conc. of poppy straw (M) AMA 19. Alphacetylmethadol 53. Conc. of poppy straw (M) AOA 20. Alphameprodine 54. Conc. of poppy straw (M) ATA 21. Alphamethadol 55. Conc. of poppy straw (M) GW 22. alpha-Methylfentanyl 56. Conc. of poppy straw (N) GW 23. alpha-Methylthiofentanyl 57. Conc. of poppy straw (O) 24. Alphaprodine 58. Conc. of poppy straw (O) ACA 25. Anileridine 59. Conc. of poppy straw (O) AMA 26. Benzethidine 60. Conc. of poppy straw (O) AOA 27. -
SOP414 Acetyl Fentanyl by LC MS MS
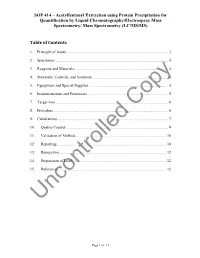
SOP 414 – Acetylfentanyl Extraction using Protein Precipitation for Quantification by Liquid Chromatography/Electrospray Mass Spectrometry/ Mass Spectrometry (LC/MS/MS) Table of Contents 1. Principle of Assay ........................................................................................................ 3 2. Specimens .................................................................................................................... 4 3. Reagents and Materials ................................................................................................ 4 4. Standards, Controls, and Solutions .............................................................................. 4 5. Equipment and Special Supplies ................................................................................. 5 6. Instrumentation and Parameters .................................................................................. 5 7. Target Ions ................................................................................................................... 6 8. Procedure ..................................................................................................................... 6 9. Calculations ................................................................................................................. 7 10. Quality Control ........................................................................................................ 9 11. Validation of Method ............................................................................................ -
![[1-(2-Phenylethyl)Piperidin-4-Yl]Furan- 2-Carboxamide (Furanylfentanyl)](https://docslib.b-cdn.net/cover/8639/1-2-phenylethyl-piperidin-4-yl-furan-2-carboxamide-furanylfentanyl-1718639.webp)
[1-(2-Phenylethyl)Piperidin-4-Yl]Furan- 2-Carboxamide (Furanylfentanyl)
ANNEX 1 Technical report on N-phenyl-N- [1-(2-phenylethyl)piperidin-4-yl]furan- 2-carboxamide (furanylfentanyl) Report prepared by ‘furanylfentanyl’, ‘furanyl-fentanyl’, ‘furanyl fentanyl’, Simon Brandt (1), Simon Elliott (1), Helgi Valur ‘Fu-F’, ‘fentanyl furanyl analogue’. Danielsson, Anabela Almeida, Ana Gallegos, Rita Jorge, Rachel Christie, Michael Evans-Brown, Roumen Sedefov. The REACH registered substances database hosted by the European Chemicals Agency (ECHA) was searched using the CAS registry numbers listed below. The Data sources searches returned no hits. The information in this technical report is derived from: Cursory, though repeated, inspections of English- data reported by the Member States, Turkey and language Internet forums covered Bluelight, Drugs- Norway to the EMCDDA and Europol in accordance forum, ecstasydata.org, Erowid, Eve&Rave, Reddit and with Council Decision 2005/387/JHA on the The Vespiary. information exchange, risk-assessment and control of new psychoactive substances (2) (EMCDDA, 2017c); Additionally, the scientific networks of the authors were and, contacted to obtain information. data collected through systematic searches of open source information, including the scientific and medical literature, patents, official reports, grey literature, Internet drug discussion forums and related Section A. Physical, chemical, websites, and online vendors selling furanylfentanyl. pharmaceutical and pharmacological information Search strategy Literature searches used both chemical structure and A1. Physical, -

Government Notice
DEPARTMENT OF HEALTH MEDICINES AND RELATED SUBSTANCES ACT, 1965 (ACT 101 OF 1965) CONSOLIDATED SCHEDULES 21 JUNE 2019 The Minister of Health has, in terms of section 22A(2) of the Medicines and Related Substances Act, 1965 (Act 101 of 1965), on the recommendation of the South African Health Products Regulatory Authority (SAHPRA), made and updated the Schedules in the Schedule. SCHEDULE In these Schedules, "the Act" means the Medicines and Related Substances Act, 1965 (Act 101 of 1965) Note: Where an alternative schedule(s) is included in natural parentheses at any point of an inscription, this is provided to indicate one or more alternative scheduling designation/s. This is for information only and shall not be used in the interpretation of such inscription. SCHEDULE 0 a. All substances referred to in this Schedule are excluded when specifically packed, labelled, sold and used for – (i) industrial purposes including the manufacture or compounding of consumer items or products which have no pharmacological action or medicinal purpose, and which are intended to be ingested by man or animals as a food or applied to the body as a cosmetic, and which are approved for such use in terms of the Foodstuffs, Cosmetics and Disinfectants Act, 1972 (Act 54 of 1972) or that are registered in terms of the Fertilizers, Farm Feeds, Agricultural Remedies and Stock Remedies Act, 1947 (Act 36 of 1947); and (ii) analytical laboratory purposes. b. This Schedule shall include all substances or mixtures of such substances containing or purporting to contain substances referred to, including the salts and esters of such substances, where the existence of such salts and esters is possible, except where such substances or mixtures of substances are expressly excluded.