IRS2 Mutations Linked to Invasion in Pleomorphic Invasive Lobular Carcinoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Fiction of Gothic Egypt and British Imperial Paranoia: the Curse of the Suez Canal
The Fiction of Gothic Egypt and British Imperial Paranoia: The Curse of the Suez Canal AILISE BULFIN Trinity College, Dublin “Ah, my nineteenth-century friend, your father stole me from the land of my birth, and from the resting place the gods decreed for me; but beware, for retribution is pursuing you, and is even now close upon your heels.” —Guy Boothby, Pharos the Egyptian, 1899 What of this piercing of the sands? What of this union of the seas?… What good or ill from LESSEPS’ cut Eastward and Westward shall proceed? —“Latest—From the Sphinx,” Punch, 57 (27 November 1869), 210 IN 1859 FERDINAND DE LESSEPS began his great endeavour to sunder the isthmus of Suez and connect the Mediterranean with the Red Sea, the Occident with the Orient, simultaneously altering the ge- ography of the earth and irrevocably upsetting the precarious global balance of power. Ten years later the eyes of the world were upon Egypt as the Suez Canal was inaugurated amidst extravagant Franco-Egyp- tian celebrations in which a glittering cast of international dignitar- ies participated. That the opening of the canal would be momentous was acknowledged at the time, though the nature of its impact was a matter for speculation, as the question posed above by Punch implies. While its codevelopers France and Egypt pinned great hopes on the ca- nal, Britain was understandably suspicious of an endeavor that could potentially undermine its global imperial dominance—it would bring India nearer, but also make it more vulnerable to rival powers. The inauguration celebrations -
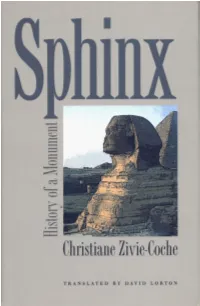
Sphinx Sphinx
SPHINX SPHINX History of a Monument CHRISTIANE ZIVIE-COCHE translated from the French by DAVID LORTON Cornell University Press Ithaca & London Original French edition, Sphinx! Le Pen la Terreur: Histoire d'une Statue, copyright © 1997 by Editions Noesis, Paris. All Rights Reserved. English translation copyright © 2002 by Cornell University All rights reserved. Except for brief quotations in a review, this book, or parts thereof, must not be reproduced in any form without permission in writing from the publisher. For information, address Cornell University Press, Sage House, 512 East State Street, Ithaca, New York 14850. First published 2002 by Cornell University Press Printed in the United States of America Library of Congress Cataloging-in-Publication Data Zivie-Coche, Christiane. Sphinx : history of a moument / Christiane Zivie-Coche ; translated from the French By David Lorton. p. cm. Includes bibliographical references and index. ISBN 0-8014-3962-0 (cloth : alk. paper) 1. Great Sphinx (Egypt)—History. I.Tide. DT62.S7 Z58 2002 932—dc2i 2002005494 Cornell University Press strives to use environmentally responsible suppliers and materials to the fullest extent possible in the publishing of its books. Such materi als include vegetable-based, low-VOC inks and acid-free papers that are recycled, totally chlorine-free, or partly composed of nonwood fibers. For further informa tion, visit our website at www.cornellpress.cornell.edu. Cloth printing 10 987654321 TO YOU PIEDRA en la piedra, el hombre, donde estuvo? —Canto general, Pablo Neruda Contents Acknowledgments ix Translator's Note xi Chronology xiii Introduction I 1. Sphinx—Sphinxes 4 The Hybrid Nature of the Sphinx The Word Sphinx 2. -

Lipid Related Genes Altered in NASH Connect Inflammation in Liver Pathogenesis Progression to HCC: a Canonical Pathway
Lipid related genes altered in NASH connect inflammation in liver pathogenesis progression to HCC: a canonical pathway Christophe Desterke1, Franck Chiappini2* 1 Inserm, U935, Villejuif, F-94800, France 2 Cell Growth and Tissue Repair (CRRET) Laboratory, Université Paris-Est Créteil (UPEC), EA 4397 / ERL CNRS 9215, F-94010, Créteil, France. Corresponding author: *Franck Chiappini. Laboratoire du CRRET (Croissance, Réparation et Régénération Tissulaires), Université Paris-Est Créteil, 61 avenue du Général de Gaulle F- 94010, Créteil Cedex, Val de Marne, France. Email address: [email protected]; Tel: +33(0)145177080; Fax: +33(0)145171816 Supplementary Information Supplementary Datasets Table S1: Text-mining list of genes associated in PubMed literature with lipid related keywords. Supplementary Datasets Table S2: Expression fold change of lipid related genes found differentially expressed between NASH and healthy obese liver samples. Supplementary Datasets Table S3: Liver as principal filter for prioritization of lipid related genes found differentially expressed in NASH. Supplementary Datasets Table S4: Gene prioritization secondary filters (immunological, inflammation, liver pathogenesis progression) table found with lipid related genes differentially expressed in NASH. Supplementary Datasets Table S5: Identification of protein partners of YWHAZ gene using InnateDB database. Supplementary Datasets Table S1: Text-mining list of genes associated in PubMed literature with lipid related keywords. Ranking of "lipidic" textmining Gene symbol -

Alien Invasions, Vulnerable Bodies: Science Fiction and the Biopolitics of Embodiment from H
1 Alien Invasions, Vulnerable Bodies: Science Fiction and the Biopolitics of Embodiment from H. G. Wells to Octavia Butler By Rosalind Diaz A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in English in the Graduate Division of the University of California, Berkeley Committee in charge: Professor Katherine Snyder, Chair Professor Mark Goble Professor Mel Chen Fall 2018 1 Alien Invasions, Vulnerable Bodies: Science Fiction and the Biopolitics of Embodiment from H. G. Wells to Octavia Butler © 2018 Rosalind Diaz 1 Abstract Alien Invasions, Vulnerable Bodies: Science Fiction and the Biopolitics of Embodiment from H. G. Wells to Octavia Butler by Rosalind Diaz Doctor of Philosophy in English University of California, Berkeley Professor Katherine Snyder, Chair This dissertation turns to alien invasion narratives to elucidate the social, ethical and political consequences associated with the modern body as an entity with clearly defined borders. The imperatives of liberalism and neoliberalism constitute the modern body as a white, male, heteronormative body, navigating appropriate relationships to production and consumption. How does the human body emerge as a bounded entity in science and science fiction from the nineteenth century onward? Alien invasion narratives offer a fruitful way to trace this concept and its development over time. These narratives model proper ways of attending to one’s body as well as proper ways of defending oneself—and, by extension, the planet—from alien invasion. The present inquiry focuses on three different alien invasion narratives, beginning with H. G. Wells’s influential The War of the Worlds (1897), before moving to consider a pair of twentieth- century American texts: Philip Kaufman’s film Invasion of the Body Snatchers (1978) and Octavia Butler’s novel Fledgling (2005). -

Teaching Social Studies Through Film
Teaching Social Studies Through Film Written, Produced, and Directed by John Burkowski Jr. Xose Manuel Alvarino Social Studies Teacher Social Studies Teacher Miami-Dade County Miami-Dade County Academy for Advanced Academics at Hialeah Gardens Middle School Florida International University 11690 NW 92 Ave 11200 SW 8 St. Hialeah Gardens, FL 33018 VH130 Telephone: 305-817-0017 Miami, FL 33199 E-mail: [email protected] Telephone: 305-348-7043 E-mail: [email protected] For information concerning IMPACT II opportunities, Adapter and Disseminator grants, please contact: The Education Fund 305-892-5099, Ext. 18 E-mail: [email protected] Web site: www.educationfund.org - 1 - INTRODUCTION Students are entertained and acquire knowledge through images; Internet, television, and films are examples. Though the printed word is essential in learning, educators have been taking notice of the new visual and oratory stimuli and incorporated them into classroom teaching. The purpose of this idea packet is to further introduce teacher colleagues to this methodology and share a compilation of films which may be easily implemented in secondary social studies instruction. Though this project focuses in grades 6-12 social studies we believe that media should be infused into all K-12 subject areas, from language arts, math, and foreign languages, to science, the arts, physical education, and more. In this day and age, students have become accustomed to acquiring knowledge through mediums such as television and movies. Though books and text are essential in learning, teachers should take notice of the new visual stimuli. Films are familiar in the everyday lives of students. -

Costimulation of Resting B Lymphocytes Alters the IL-4
Cell Research, (2001); 11(1):44-54 Costimulation of resting B lymphocytes alters the IL-4-activated IRS2 signaling pathway in a STAT6 independent manner: impli- cations for cell survival and proliferation ZAMORANO JOSE*, ANN E KELLY, JONATHAN AUSTRIAN, HELEN Y WANG, ACHSAH D KEEGAN** Department of Immunology, Jerome Holland Labs, American Red Cross, Rockville, MD, USA ABSTRACT IL-4 is an important B cell survival and growth factor. IL-4 induced the tyrosine phosphorylation of IRS2 in resting B lymphocytes and in LPS- or CD40L-activated blasts. Phosphorylated IRS2 coprecipitated with the p85 subunit of PI 3' kinase in both resting and activated cells. By contrast, association of phosphory- lated IRS2 with GRB2 was not detected in resting B cells after IL-4 treatment although both proteins were expressed. However, IL-4 induced association of IRS2 with GRB2 in B cell blasts. The pattern of IL-4- induced recruitment of p85 and GRB2 to IRS2 observed in B cells derived from STAT6 null mice was identical to that observed for normal mice. While IL-4 alone does not induce activation of MEK, a MEK1 inhibitor suppressed the IL-4-induced proliferative response of LPS-activated B cell blasts. These results demonstrate that costimulation of splenic B cells alters IL-4-induced signal transduction independent of STAT6 leading to proliferation. Furthermore, proliferation induced by IL-4 in LPS-activated blasts is de- pendent upon the MAP kinase pathway. Key words: B lymphocytes, IL-4, survival, proliferation. INTRODUCTION Interleukin-4 (IL-4), a cytokine produced by T The inappropriate enhancement of lymphocyte cells, mast cells, and basophils, has profound ef- survival due to a block in programmed cell death fects on the growth and differentiation of B and T and/or an enhancement of entry into the cell cycle lymphocytes[3]. -

Neuronal Insulin Receptor Substrate 2 (IRS2) Expression Is Regulated by ZBP89 and SP1 Binding to the IRS2 Promoter
199 Neuronal insulin receptor substrate 2 (IRS2) expression is regulated by ZBP89 and SP1 binding to the IRS2 promoter Michael Udelhoven, Mareike Pasieka, Uschi Leeser, Wilhelm Krone and Markus Schubert Department of Internal Medicine II, Center for Molecular Medicine Cologne (CMMC) and Cologne Excellence Cluster on Cellular Stress Responses in Aging-associated Diseases (CECAD), University of Cologne, Kerpener Straße 62, 50937 Cologne, Germany (Correspondence should be addressed to M Schubert; Email: [email protected]) Abstract Since neuronal insulin receptor substrate 2 (IRS2)-mediated phosphoinositide-3-kinase (PI3K) via increased ZBP89 binding signals coordinate key processes in rodent physiology such as to the promoter. Serum starvation caused increased SP1 binding food intake, fertility, longevity, and aging-related behavior, we at one specific SP1 site and decreased binding to another, analyzed the mechanisms of neuronal IRS2 expression in proving a regulatory interaction between the different binding neuroblastoma (SHSY5Y) and hypothalamic (GT1-7) cell lines. sites within this promoter cassette to tightly control IRS2 Using dual luciferase reporter assays and IRS2 promoter expression. Mutants containing all the possible combinations of deletion constructs, we identified a regulatory cassette within one, two, three, or all the four SP1 binding sites of the IRS2 the IRS2 promoter between K779 and K679 bp from the promoter revealed that SP1 binding to one particular site is translational start which is responsible for w50% of neuronal most important for promoter activation. Stable downregulation IRS2 promoter activity.Chromatin immunoprecipitation assays of ZBP89 using siRNA substantially increased IRS2 mRNA and electromobility shift assay revealed four overlapping and protein expression. -

Identifying Spatial Invasion of Pandemics on Metapopulation
Identifying spatial invasion of pandemics on metapopulation networks via anatomizing arrival history* Jian-Bo Wang, Student Member, IEEE, Lin Wang, Member, IEEE, and Xiang Li, Senior Member, IEEE Abstract—Spatial spread of infectious diseases among pop- During almost the same epoch, the theory of complex ulations via the mobility of humans is highly stochastic and networks has been developed as a valuable tool for modeling heterogeneous. Accurate forecast/mining of the spread process the structure and dynamics of/on complex systems [13]-[16]. is often hard to be achieved by using statistical or mechanical models. Here we propose a new reverse problem, which aims In the study of network epidemiology, networks are often to identify the stochastically spatial spread process itself from used to describe the epidemic spreading from human to observable information regarding the arrival history of infectious human via contacts, where nodes represent persons and edges cases in each subpopulation. We solved the problem by devel- represent interpersonal contacts [17]-[22]. To characterize the oping an efficient optimization algorithm based on dynamical spatial spread between different geo-locations, simple network programming, which comprises three procedures: i, anatomizing the whole spread process among all subpopulations into disjoint models are generalized with metapopulation framework, in componential patches; ii, inferring the most probable invasion which each node represents a population of individuals that pathways underlying each patch via maximum likelihood estima- reside at the same geo-region (e.g. a city), and the edge tion; iii, recovering the whole process by assembling the invasion describes the traffic route that drives the individual mobility pathways in each patch iteratively, without burdens in parameter between populations [18], [19]. -

A Novel JAK1 Mutant Breast Implant-Associated Anaplastic Large Cell Lymphoma Patient-Derived Xenograft Fostering Pre- Clinical Discoveries
Cancers 2019 S1 of S18 Supplementary Materials: A Novel JAK1 Mutant Breast Implant-Associated Anaplastic Large Cell Lymphoma Patient-Derived Xenograft Fostering Pre- Clinical Discoveries Danilo Fiore, Luca Vincenzo Cappelli, Paul Zumbo, Jude M. Phillip, Zhaoqi Liu, Shuhua Cheng, Liron Yoffe, Paola Ghione, Federica Di Maggio, Ahmet Dogan, Inna Khodos, Elisa de Stanchina, Joseph Casano, Clarisse Kayembe, Wayne Tam, Doron Betel, Robin Foa’, Leandro Cerchietti, Raul Rabadan, Steven Horwitz, David M. Weinstock and Giorgio Inghirami A B C Figure S1. (A) Histology micrografts on IL89 PDTX show overall similarity between T1 T3 and T7 passages (upper panels). Immunohistochemical stains with the indicated antibodies (anti-CD3, anti- CD25 and anti-CD8 [x20]) (lower panels). (B) Flow cytometry panel comprehensive of the most represented surface T-cell lymphoma markers, including: CD2, CD3, CD4, CD5, CD8, CD16, CD25, CD30, CD56, TCRab, TCRgd. IL89 PDTX passage T3 is here depicted for illustration purposes. (C) Analysis of the TCR gamma specific rearrangement clonality in IL89 diagnostic sample and correspondent PDTX after 1 and 5 passages (T1 and T5). A WT Primary p.G1097D IL89 T1 p.G1097D IL89 T5 p.G1097D IL89 cell line B Figure S2. (A) Sanger sequencing confirms the presence of the JAK1 p.G1097D mutation in IL89 PDTX samples and in the cell line, but the mutation is undetectable in the primary due to the low sensitivity of the technique. (B) Manual backtracking of mutations in the primary tumor using deep sequencing data allowed for the identification of several hits at a very low VAF compared to the PDTX-T5. A B IL89 CTRL 30 CTRL Ruxoli?nib S 20 M Ruxoli?nib A R G 10 0 1 2 3 4 5 6 7 8 9 0 1 2 3 4 1 1 1 1 1 WEEKS AFTER ENGRAFTMENT Figure S3. -

Assessing the Relationship Between Propagule Pressure and Invasion Risk in Ballast Water
ASSESSING THE RELATIONSHIP BETWEEN PROPAGULE PRESSURE AND INVASION RISK IN BALLAST WATER Committee on Assessing Numeric Limits for Living Organisms in Ballast Water Water Science and Technology Board Division on Earth and Life Studies THE NATIONAL ACADEMIES PRESS Washington, D.C. www.nap.edu PREPUBLICATION COPY THE NATIONAL ACADEMIES PRESS 500 Fifth Street, N.W. Washington, DC 20001 NOTICE: The project that is the subject of this report was approved by the Governing Board of the National Research Council, whose members are drawn from the councils of the National Academy of Sciences, the National Academy of Engineering, and the Institute of Medicine. The members of the panel responsible for the report were chosen for their special competences and with regard for appropriate balance. Support for this study was provided by the EPA under contract no. EP-C-09-003, TO#11. Any opinions, findings, conclusions, or recommendations expressed in this publication are those of the author(s) and do not necessarily reflect the views of the organizations or agencies that provided support for the project. International Standard Book Number X-XXX-XXXXX-X Library of Congress Catalog Card Number XX-XXXXX Additional copies of this report are available from the National Academies Press, 500 5th Street, N.W., Lockbox 285, Washington, DC 20055; (800) 624-6242 or (202) 334-3313 (in the Washington metropolitan area); Internet, http://www.nap.edu. Copyright 2011 by the National Academy of Sciences. All rights reserved. Printed in the United States of America. PREPUBLICATION COPY The National Academy of Sciences is a private, nonprofit, self-perpetuating society of distinguished scholars engaged in scientific and engineering research, dedicated to the furtherance of science and technology and to their use for the general welfare. -

Rethinking Regulatory Reform: Toxics, Politics, and Ethics
Notes Rethinking Regulatory Reform: Toxics, Politics, and Ethics Jay Michaelson When do we kill people for a desired goal? With the value of life rhetorically paramount in American culture, only extreme cases-war and capital punishment, for instance-tend to be regarded (hardly unanimously) as "acceptable" instances of state-sanctioned killing. Yet the state allows lives to be lost all the time. In less obvious instances of state control, such as regulating safety' or allocating scarce resources,2 the state must make difficult, "tragic" choices of how many lives to sacrifice in exchange for benefits that may not be coequal with life itself In the end, we Americans kill people when we want to do so; the important questions are what values justify our actions and how we weigh competing claims on human life. Regulation, then, is more than simple control, more than a dry pantomime of acronyms and number crunching; it is a process of harm allocation that reflects the state's ethical values even as it subverts them. In regulating toxics, 4 for example, the Environmental Protection Agency (EPA) and others must set "acceptable" levels of risk posed by toxic substances, i.e., determine how much cancer is worth the benefits of a given toxic substance. Most discussions of toxics regulation, however, focus on the "science" of risk assessment and the politics of risk management, thus missing the heart of EPA's harm allocation effort: the initial decision of how much harm is to be allowed-how many people are to die. Now, as reform of the regulatory process is debated in Washington, it is worth rethinking what regulation is, and how we control and justify the allocation of toxic harms. -

Prolonged Elimination of Negative Feedback Control Mechanisms Along the Insulin Signalling Pathway Impairs Cell Function in Vivo
Page 1 of 39 Diabetes 1 Prolonged Elimination of Negative Feedback Control Mechanisms Along the Insulin Signalling Pathway Impairs Cell Function In Vivo Roi Isaac, Yaron Vinik, Sigalit Boura-Halfon, Lydia Farack, Sarina Streim, Eytan Elhanany, Zvi Kam, and Yehiel Zick Department of Molecular Cell Biology, Weizmann Institute of Science, Rehovot 76100, Israel Running Title: Effects of IRS2 on -cell functionin vivo Corresponding Author: Yehiel Zick, Department of Molecular Cell Biology, Weizmann Institute of Science Rehovot,76100 Israel; Tel: +972-89-342380; Fax: +972-89-344125; e-mail: [email protected] Words : 3,999 Figures: 8 Diabetes Publish Ahead of Print, published online April 19, 2017 Page 2 of 39 Diabetes Abstract 2 Cellular stress and pro-inflammatory cytokines induce phosphorylation of insulin receptor substrate (IRS) proteins at Ser sites that inhibit insulin and IGF-1 signalling. We therefore examined the effects of mutation of five ‘inhibitory’Ser phosphorylation sitesonIRS2 function in transgenic mice that overexpress, selectively in pancreatic cells, either wild-type (WT) or a mutated IRS2 protein (IRS25A).Islets size, number, and mRNA levels of catalase and superoxide dismutase, were increased, while those of nitric oxide synthase were decreased in 7-10 weeks old IRS25A-β micecompared to IRS2WT-β mice. However, glucose homeostasis and insulin secretion in IRS25A-β mice were impaired, when compared to IRS2WT-β mice or to non-transgenic animals. This was associated withreduced mRNA levels of Glut2 and islet cell transcription factors such as Nkx6.1 and MafA.Similarly, components mediating the unfolded protein response (UPR) were decreased in islets of IRS25A-β micein accordance with their decreased insulin secretion.The beneficial effects of IRS25Aon cell proliferation and cell transcription factorswere evident only in 5-8 days old mice.These findings suggest that elimination of ‘inhibitory’ Ser phosphorylation sites of IRS2exertsshort-term beneficial effectsin vivo, howevertheir sustained elimination leads to impaired cell function.