Vital Signs Cover
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Environmental Causes and the Law Contents March/April 2013
March/April 2013 Westward – How? Civil Disobedience Help Yourself! Relating law to life in Canada Environmental Causes and the Law Contents March/April 2013 24 The Difference a Year Makes: Changes to Canadian Federal Environmental Assessment Law in 2012 Brenda Heelan Powell The omnibus budget bill of 2012 contained many measures that profoundly changed Canada’s environmental protection laws, and not for the better. 30 Nickel Shower: An Environmental Class Action Peter Bowal and Sean Keown Canadians treasure their environment, and for many, preventing The case of Smith v. Inco Ltd. is the first its degradation becomes a cause. The law can be used in some Canadian environmental class action lawsuit to interesting and unique ways to help the cause. proceed through a trial and appeal. Cover image: © Grady Mitchell Special Report: Helping Yourself Feature: Environmental Causes and the Law 35 How To Avoid Your Day in Court Carole Aippersbach 9 The Constitutional Right to a Healthy Think of the law as a spectrum with the Environment courthouse at the very end. There are lots of David R. Boyd ways that you can avoid going there! Environmental rights enjoy constitutional protection in over 100 countries. Canada is not 40 Helping Yourself: Where Do You Start? one of them, but it should be. Adriana Bugyiova There are many of sources for legal information, 14 The Oil Sands: Westward How? ranging from walk-in offices to websites to help John Edmond you access the law. There are many obstacles: technical; legal; constitutional; and political that stand in the 43 Doin' It Your Own Way… way of transporting Alberta’s bitumen out of the Unsuccessful Succession province. -

Reflections Upon My Daughter's Wedding Dealing with the Patient on Narcotics in the Brave New World AHS Narcotic Ordering
COMMUNICATING WITH PHYSICIANS IN ALBERTA September 2017 ZONE MEDICAL STAFF ASSOCIATIONS OF ALBERTA VITAL SIGNS OPIOIDS Reflections Upon My Daughter’s Wedding Dealing With The Patient on Narcotics in the Brave New World AHS Narcotic Ordering Initiative The Opioid Crisis: Community Collaboration for the Planning of Supervised Consumption Services AHS plans Supervised Consumption Services at the Sheldon Chumir The Opioid Crisis and What You Can Do About It Telephone Consultation for Opioid Dependence Therapy Medical Marijuana: Who, Why and How? Rapid Dissemination of Best Practices to Primary Care Providers Via Project ECHO NEW LOOK NEW SERVICES AT MARKET MALL Expanded services for faster, local access. Automated Breast Ultrasound Bone Scan with SPECT/CT Image-Guided Pain Therapy Fast, efficient technology for 3D Mayfair’s state-of-the-art GE Mayfair’s experienced team uses imaging of the whole breast to Discovery 670 nuclear medicine Ultrasound and X-ray guidance provide a clearer picture of dense camera provides exceptional, high- to best localize and treat pain. breast tissue. resolution, hybrid images to help localize specific areas of concern. 40 Ave NW N Mayfair Diagnostics Market Mall 333, 4935 - 40 Avenue NW Calgary, T3A 2N1 Shaganappi Tr. NW 49 St. NW SERVICES: ALL APPOINTMENTS: Bone Mineral Densitometry, 403.777.3000 Market Mall Breast Imaging, Image-Guided radiology.ca Pain Therapy, Nuclear Medicine Imaging, Ultrasound, X-ray 32 Ave. NW MEDICAL IMAGING REIMAGINED A CALGARY & AREA MEDICAL STAFF SOCIETY PUBLICATION September 2017 CAMSS EXECUTIVE President: Dr. Sharron L. Spicer – Contents: [email protected] President-Elect: Dr. Linda Mrkonjic – Reflections Upon My Daughter’s Wedding ................................................2 [email protected] Secretary-Treasurer: Dr. -

Financial Assistance and Awards – Introduction Financial Assistance and Awards
60 Financial Assistance and Awards – Introduction Financial Assistance and Awards Financial Assistance General Information and • The senate policy committee on scholarships, awards and bursaries ensures that all scholarships, 3200 Maggie Benston Student Services Centre, Regulations awards and bursaries administered by the University 604.294.8600 Registrar Information Service (Touch The following regulations apply generally to all or listed in its Calendar, are in the best interests of Tone service only), 604.291.4356 general enquiries, financial assistance administered by the University. the University as an academic institution. The terms 604.291.4722 Fax, www.reg.sfu.ca/fa/ • All scholarships, awards and bursaries are given on of reference for scholarships, awards and bursaries the recommendation of the senate undergraduate should not include restrictive criteria unrelated to Introduction awards adjudication committee. Committee academic merit or financial need such as race, decisions, when announced, are final. creed, colour, sex, or national origin, when the Students are eligible for a variety of financial • The University does not guarantee the payment of committee determines these criteria are improper or assistance programs including entrance or continuing any scholarships, awards or bursaries listed in the irrelevant. scholarships, bursaries, awards, and loans. Calendar other than those provided directly from • The senate undergraduate awards adjudication Scholarships recognize outstanding academic funds of the University. If invested funds do not committee has the right to give special achievements; bursaries are awarded on the basis of provide the necessary income for an endowed consideration to course load requirements on financial need; awards generally acknowledge scholarship, award or bursary payment of the award scholarships, awards or bursaries for persons with outstanding achievements or contributions to the may be reduced or the award withheld. -

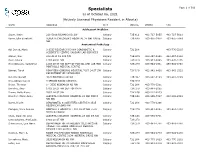
Specialists Page 1 of 508 As of October 03, 2021 (Actively Licensed Physicians Resident in Alberta)
Specialists Page 1 of 508 as of October 03, 2021 (Actively Licensed Physicians Resident in Alberta) NAME ADDRESS CITY POSTAL PHONE FAX Adolescent Medicine Soper, Katie 220-5010 RICHARD RD SW Calgary T3E 6L1 403-727-5055 403-727-5011 Vyver, Ellie Elizabeth ALBERTA CHILDREN'S HOSPITAL 28 OKI DRIVE Calgary T3B 6A8 403-955-2978 403-955-7649 NW Anatomical Pathology Abi Daoud, Marie 9-3535 RESEARCH RD NW DIAGNOSTIC & Calgary T2L 2K8 403-770-3295 SCIENTIFIC CENTRE CALGARY LAB SERVICES Alanen, Ken 242-4411 16 AVE NW Calgary T3B 0M3 403-457-1900 403-457-1904 Auer, Iwona 1403 29 ST NW Calgary T2N 2T9 403-944-8225 403-270-4135 Benediktsson, Hallgrimur 1403 29 ST NW DEPT OF PATHOL AND LAB MED Calgary T2N 2T9 403-944-1981 493-944-4748 FOOTHILLS MEDICAL CENTRE Bismar, Tarek ROKYVIEW GENERAL HOSPITAL 7007 14 ST SW Calgary T2V 1P9 403-943-8430 403-943-3333 DEPARTMENT OF PATHOLOGY Bol, Eric Gerald 4070 BOWNESS RD NW Calgary T3B 3R7 403-297-8123 403-297-3429 Box, Adrian Harold 3 SPRING RIDGE ESTATES Calgary T3Z 3M8 Brenn, Thomas 9 - 3535 RESEARCH RD NW Calgary T2L 2K8 403-770-3201 Bromley, Amy 1403 29 ST NW DEPT OF PATH Calgary T2N 2T9 403-944-5055 Brown, Holly Alexis 7007 14 ST SW Calgary T2V 1P9 403-212-8223 Brundler, Marie-Anne ALBERTA CHILDREN HOSPITAL 28 OKI DRIVE Calgary T3B 6A8 403-955-7387 403-955-2321 NW NW Bures, Nicole DIAGNOSTIC & SCIENTIFIC CENTRE 9 3535 Calgary T2L 2K8 403-770-3206 RESEARCH ROAD NW Caragea, Mara Andrea FOOTHILLS HOSPITAL 1403 29 ST NW 7576 Calgary T2N 2T9 403-944-6685 403-944-4748 MCCAIG TOWER Chan, Elaine So Ling ALBERTA CHILDREN HOSPITAL 28 OKI DR NW Calgary T3B 6A8 403-955-7761 Cota Schwarz, Ana Lucia 1403 29 ST NW Calgary T2N 2T9 DiFrancesco, Lisa Marie DEPARTMENT OF PATHOLOGY (CLS) MCCAIG Calgary T2N 2T9 403-944-4756 403-944-4748 TOWER 7TH FLOOR FOOTHILLS MEDICAL CENTRE 1403 29TH ST NW Duggan, Maire A. -

Alberta's Rights Revolution
Dominique Clément Alberta's rights revolution Studies of human rights that focus on international politics or institutions fail to convey the complex influence of human rights on law, politics and society in a local context. This article documents the impact of the rights revolution in Alberta. The rights revolution emerged in the province beginning in the 1970s following the election of the Progressive Conservative Party in 1971. Many of the issues that typified Alberta's rights revolution were unique to this region: censorship, eugenics and discrimi nation against Hutterites, Aboriginals, Blacks and French Canadians. However, as the controversy surrounding discrimination on the basis of sexual orientation demonstrates, Alberta's rights revolution remains an unfulfilled promise. Keywords: Alberta, human rights, civil liberties, history, social movements, politics Since 1998 the Supreme Court of Canada has required the government of Alberta to enforce its provincial human rights legislation as if it included sexual orientation as a prohibited ground of discrimination. And yet it was not until 2010 - when the government introduced a new Human Rights Act - that the term sexual orientation was formally written into the legislation. The Human Rights Act included another notable addition: teachers are now prohibited from discussing sexual orientation, sexuality or religion to children of parents who demanded an exemption. No other jurisdiction in Canada has ever created the possibility that teaching could be a human rights violation in this way. The Edmonton Journal described the amendment as ‘unnecessary, divisive and potentially damaging ... the bill only serves to reinforce stereotypes of Albertans in other parts of the country that are at odds with the tolerant, multicultural, open-minded reality in this most urban of places’ (Editorial 2009). -

Teacher Workload 3 on Summer Conference Initial Report Released the Provincial Framework Agreement (PFA) Between Teachers and the Alberta Government Is in Effect
ATA News revamp: 48-year-old publication gets a nip and tuck—Editorial, page 2. ATANEWS WELCOME August 27, 2013 Volume 48, Number 1 News Publication of The Alberta Teachers’ Association BACK Students ready to hit the books Librarian Pauline Zapisocky at St. Catherine School, in Edmonton, signed out textbooks to Grade 9 students on the first day of school on August 12. St. Catherine School is one of three schools in the Edmonton Catholic Schools district that offer the year- round schooling calendar. Students returned to school in mid-August but will enjoy a two-week fall break in October and a two-week spring break in March. About 100 schools in Canada follow the year-round schooling calendar. The calendar provides more continuous learning for students, particularly in reading and math, than the traditional calendar. YUET CHAN Your views . Teacher workload 3 On summer conference Initial report released The provincial framework agreement (PFA) between teachers and the Alberta government is in effect. Key components of the PFA were designed to relieve work- load concerns that inhibit teachers’ core work with students. A preliminary review of Alberta Education–initiated tasks was conducted and a report sent to the Alberta Teachers’ Associa- tion on June 28. See WORKLOAD on page 4 Teachers Albertans don’t support Workload issues are very real, 5 privatizing public education Q&A, page 2 In the recent Alberta budget, millions of dollars were devoted to funding private ATA Gold Medals in Education, education, even though there appears page 4 to be very little public support for this. -

2009 Annual Report
Board Board of Directors of Directors 2008-2009 2009-2010 2008-2009 Annual Report Donald G. Cormack, C.A. Beverley Foy, C.A. CHAIR Partner, Collins Barrow Calgary LLP Partner, Director Since 2008 PricewaterhouseCoopers LLP Director Since 2001 Ross Kobayashi Community Volunteer Alison T. Love, VICE CHAIR Director Since 2005 The Calgary Foundation distributed $22 million to approach to investing that minimizes risk. This approach Vice President & Corporate achieves a long term return that enables a distribution Secretary, Enbridge Inc. 655 charitable organizations in the 2008–2009 of 5% to community, while maintaining the value of the Director Since 2003 endowment over the long term. fiscal year. The Calgary Foundation believes that philanthropy has The Calgary Foundation’s Annual Report recognizes the an important role to play in building a strong and vibrant generosity of donors who have chosen to partner with the community – now, more than ever. To inspire new and Din Ladak Foundation to achieve their philanthropic goals and who different conversations appropriate in this challenging CEO, Immigrant Services Calgary are committed to supporting those in need, especially economic time, the Foundation will host, this fall, a forum Director Since 2003 during challenging financial times. The Report also Ali A. Bhojani ‘Shaping Relationships to Sustain a Healthy Nonprofit highlights the outstanding charitable organizations that Investment Banking Sector’ that will convene members from all sectors - Director Since 2009 rise above the challenges and continue to do more. public, private and charitable, to seek transformational We are fortunate to live in an affluent and generous city. solutions through innovation, collaboration, engagement In the recently published 2007 Canada Survey of Giving/ and leadership. -
Specialists Page 1 of 509 As of October 06, 2021 (Actively Licensed Physicians Resident in Alberta)
Specialists Page 1 of 509 as of October 06, 2021 (Actively Licensed Physicians Resident in Alberta) NAME ADDRESS CITY POSTAL PHONE FAX Adolescent Medicine Soper, Katie 220-5010 RICHARD RD SW Calgary T3E 6L1 403-727-5055 403-727-5011 Vyver, Ellie Elizabeth ALBERTA CHILDREN'S HOSPITAL 28 OKI DRIVE Calgary T3B 6A8 403-955-2978 403-955-7649 NW Anatomical Pathology Abi Daoud, Marie 9-3535 RESEARCH RD NW DIAGNOSTIC & Calgary T2L 2K8 403-770-3295 SCIENTIFIC CENTRE CALGARY LAB SERVICES Alanen, Ken 242-4411 16 AVE NW Calgary T3B 0M3 403-457-1900 403-457-1904 Auer, Iwona 1403 29 ST NW Calgary T2N 2T9 403-944-8225 403-270-4135 Benediktsson, Hallgrimur 1403 29 ST NW DEPT OF PATHOL AND LAB MED Calgary T2N 2T9 403-944-1981 493-944-4748 FOOTHILLS MEDICAL CENTRE Bismar, Tarek ROKYVIEW GENERAL HOSPITAL 7007 14 ST SW Calgary T2V 1P9 403-943-8430 403-943-3333 DEPARTMENT OF PATHOLOGY Bol, Eric Gerald 4070 BOWNESS RD NW Calgary T3B 3R7 403-297-8123 403-297-3429 Box, Adrian Harold 3 SPRING RIDGE ESTATES Calgary T3Z 3M8 Brenn, Thomas 9 - 3535 RESEARCH RD NW Calgary T2L 2K8 403-770-3201 Bromley, Amy 1403 29 ST NW DEPT OF PATH Calgary T2N 2T9 403-944-5055 Brown, Holly Alexis 7007 14 ST SW Calgary T2V 1P9 403-212-8223 Brundler, Marie-Anne ALBERTA CHILDREN HOSPITAL 28 OKI DRIVE Calgary T3B 6A8 403-955-7387 403-955-2321 NW NW Bures, Nicole DIAGNOSTIC & SCIENTIFIC CENTRE 9 3535 Calgary T2L 2K8 403-770-3206 RESEARCH ROAD NW Caragea, Mara Andrea FOOTHILLS HOSPITAL 1403 29 ST NW 7576 Calgary T2N 2T9 403-944-6685 403-944-4748 MCCAIG TOWER Chan, Elaine So Ling ALBERTA CHILDREN HOSPITAL 28 OKI DR NW Calgary T3B 6A8 403-955-7761 Cota Schwarz, Ana Lucia 1403 29 ST NW Calgary T2N 2T9 DiFrancesco, Lisa Marie DEPARTMENT OF PATHOLOGY (CLS) MCCAIG Calgary T2N 2T9 403-944-4756 403-944-4748 TOWER 7TH FLOOR FOOTHILLS MEDICAL CENTRE 1403 29TH ST NW Duggan, Maire A. -

Faculty of Rehabilitation Medicine
www.ualberta.ca UNIVERSITY OF ALBERTA 335 Faculty of Rehabilitation Medicine 170 The Faculty of Rehabilitation Medicine 335 170 The Faculty of Rehabilitation 171 The Professors 335 171.1 Teaching and Scholarship 335 Medicine 171.2 Members of the Faculty 335 172 General Information 338 Mission Statement 172.1 Undergraduate Programs 338 Through excellent teaching, research and service to the 172.2 Programs for Master’s Degrees 338 community, the Faculty of Rehabilitation Medicine is committed to 172.3 Membership in Professional Associations 338 enhancing quality of life, promoting participation and autonomy, 172.4 Budget 338 and improving function for citizens in Alberta and beyond. 173 Faculty Regulations 338 173.1 Professional Ethics/Code of Student Behaviour 338 173.2 Academic Standing and Graduation 338 173.3 Credit by Special Assessment 339 171 The Professors 173.4 Practicum Intervention Policy 339 173.5 Fieldwork/Clinical Practice Requirements 339 173.6 Appeals and Grievances 340 171.1 Teaching and Scholarship 174 Programs of Study 340 In recognition of excellence in teaching, Professor Mark 174.1 Degree of BSc in Occupational Therapy 340 Hall was selected as the 2012 recipient of the Faculty Teaching 174.2 Graduate Programs in Rehabilitation Medicine 340 Award. Other teaching award recipients for 2012 are Kim Dao for 175 Courses 340 the Faculty Sessional Teaching Award, and Jorge Fuentes for the Graduate Student Teaching Award. 171.2 Members of the Faculty Officers of the Faculty Dean and Professor V Smith, PhD M Langevin, PhD M -
Annual Report
Annual Report 2012-2013 Fiscal Year Ending March 31, 2013 Table of Contents Annual Report 2012-2013 2012-2013: Highlights ........................................................................................................................ 3 Programming Research ................................................................................................................................ 3 Publications .................................................................................................... 4 o Review of Constitutional Studies ........................................................ 4 o Constitutional Forum………………………………………………………………………5 Public Legal Education .......................................................................................................... 5 Website .......................................................................................................... 6 Summer Student Program………………………………………………………………………….6 Speakers and Events ...................................................................................... 8 o Speakers ............................................................................................. 8 o Events…………………………………………………………………………………………… 8 Documentary Projects ................................................................................... 11 Media Resource and Expert Commentary ..................................................... 12 Collaborations ................................................................................................ 12 Other ..................................................................................................................................... -

Orange Chinook: Politics in the New Alberta
University of Calgary PRISM: University of Calgary's Digital Repository University of Calgary Press University of Calgary Press Open Access Books 2019-01 Orange Chinook: Politics in the New Alberta University of Calgary Press Bratt, D., Brownsey, K., Sutherland, R., & Taras, D. (2019). Orange Chinook: Politics in the New Alberta. Calgary, AB: University of Calgary Press. http://hdl.handle.net/1880/109864 book https://creativecommons.org/licenses/by-nc-nd/4.0 Attribution Non-Commercial No Derivatives 4.0 International Downloaded from PRISM: https://prism.ucalgary.ca ORANGE CHINOOK: Politics in the New Alberta Edited by Duane Bratt, Keith Brownsey, Richard Sutherland, and David Taras ISBN 978-1-77385-026-9 THIS BOOK IS AN OPEN ACCESS E-BOOK. It is an electronic version of a book that can be purchased in physical form through any bookseller or on-line retailer, or from our distributors. Please support this open access publication by requesting that your university purchase a print copy of this book, or by purchasing a copy yourself. If you have any questions, please contact us at [email protected] Cover Art: The artwork on the cover of this book is not open access and falls under traditional copyright provisions; it cannot be reproduced in any way without written permission of the artists and their agents. The cover can be displayed as a complete cover image for the purposes of publicizing this work, but the artwork cannot be extracted from the context of the cover of this specific work without breaching the artist’s copyright. COPYRIGHT NOTICE: This open-access work is published under a Creative Commons licence. -

Charter Schools in Alberta: Change Or Continuity in Progressive Conservative Education Policy?
The Alberta Journal of Educational Research Vol. XLV, No. 1, Spring 1999,52-66 Michael Wagner University of Alberta Charter Schools in Alberta: Change or Continuity in Progressive Conservative Education Policy? The Progressive Conservative government of Premier Ralph Klein undertook an ambitious program of educational restructuring. Among other changes the government provided for the establishment of charter schools in the province. This was the first time that charter schools were to be allowed in Canada and led a number of observers to allege that this was a step toward the privatization of public education in Alberta. In other words, a radical change was taking place. However, a careful look at the education policy of Alberta's PC government reveals that it has consistently been favorable to private and quasi-private alternatives to public education. Many different policy decisions since the 1970s demonstrate this to be the case. Rather than being a radical change, then, the introduction of charter schools is simply an extension of the PC government's longstanding policy of promoting "educational choice. " Le gouvernement progressiste conservateur de Ralph Klan en Alberta a entrepris un ambi• tieux programme de restructuration du système éducatif. Parmi les modifications instaurées, on compte celle permettant l'établissement d'écoles à charte dans la province. C'était la première fois que l'on acceptait des écoles à charte au Canada et la décision a poussé certains observateurs à prétendre que cela constituait un pas vers la privatisation de l'éducation publique en Alberta; autrement dit, qu'il s'agissait d'un changement radical. Par contre, une étude approfondie de la politique du gouvernement PC de l'Alberta relatif à l'éducation révèle que, face à l'éducation publique, celui-ci s'est constamment montré favorable aux alternatives privées ou semi-privées.