Emma Jane Armstrong Harcourt
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

By Anne-Sophie Adelys
by Anne-Sophie Adelys © Anne-Sophie Adelys - 2013 - www.adelys.co.nz © Anne-Sophie Adelys - 2013 - www.adelys.co.nz 3 © Anne-Sophie Adelys - 2013 - www.adelys.co.nz © Anne-Sophie Adelys - 2013 - www.adelys.co.nz My name is Anne-Sophie Adelys. I’m French and have been living in New Zealand since 2001. I’m an artist. A painter. Each week I check “The Big idea” website for any open call for artists. On Saturday the 29th of June 2013, I answered an artist call titled: “Artist for a fringe campaign on Porn” posted by the organisation: The Porn Project. This diary documents the process of my work around this project. I’m not a writer and English is not even my first language. Far from a paper, this diary only serves one purpose: documenting my process while working on ‘The Porn Project’. Note: I have asked my friend Becky to proof-read the diary to make sure my ‘FrenchGlish’ is not too distracting for English readers. But her response was “your FrenchGlish is damn cute”. So I assume she has left it as is… © Anne-Sophie Adelys - 2013 - www.adelys.co.nz 4 4 © Anne-Sophie Adelys - 2013 - www.adelys.co.nz The artist call as per The Big Idea post (http://www.thebigidea.co.nz) Artists for a fringe campaign on porn 28 June 2013 Organisation/person name: The Porn Project Work type: Casual Work classification: OTHER Job description: The Porn Project A Fringe Art Campaign Tāmaki Makaurau/Auckland, Aotearoa/New Zealand August, 2013 In 2012, Pornography in the Public Eye was launched by people at the University of Auckland to explore issues in relation to pornography through research, art and community-based action. -
Too Late for Change in the Decision Ross Said Student Input $ and a Vote in $ Needed to Come Earlier in Friday’S Tuition $ Increase Decision
Serving UNC students and the University community since 1893 Volume 119, Issue 144 dailytarheel.com Thursday, February 2, 2012 Too LaTe for change in the decision Ross said student input $ and a vote in $ needed to come earlier in Friday’s tuition $ increase decision. $$ the tuition process. But Ross said TUITION students have had By Jessica Seaman an opportunity to Staff Writer provide their insight on tuition. “There will be some people on Student protesters, who have both sides that aren’t happy,” Ross opposed tuition increases since said. October, will likely have little He encouraged students to par- influence when the UNC-system ticipate in the tuition discussion Board of Governors votes on by communicating at the campus tuition proposals on Feb. 10. level and by sending emails to At a meeting Wednesday night, members of the board. students pushed UNC-system “I don’t know if it will have a President Thomas Ross for more difference if they vote,” he said. representation at board meetings, “But the board is trying hard to so they can be more active in the make sure students have a voice.” tuition debate. He said students also have a But Ross said it would be diffi- representative on the board to cult to know if students will influ- whom they can relay their con- ence the board’s decision when cerns. they vote in eight days. Atul Bhula, the president Wednesday’s meeting was orga- of the Association of Student nized after student groups emailed Governments, is the sole non-vot- Ross asking to work with him on ing student member of the board. -

The Boggy Shoe the Magazine of Bh7 Hash House Harriers
THE BOGGY SHOE THE MAGAZINE OF BH7 HASH HOUSE HARRIERS 1087 MAR/APR 1999 RUNS ? 1084 1085 1086 1083 1086 1082 1081 1080 01-March-99 1080 Sussex Ox Milton Street Elaine 01273 493676 08-March-99 1081 Golden Cross Portland Road, Hove Ivan (100th) & Steve 01273 707182 15-March-99 1082 Shepherd & Dog Fulking David Hearle n/k? 22-March-99 1083 Star Steyning Greyhounds Chris etc. 01273 554148 29-March-99 1084 Wheatsheaf Cuckfield Bouncer (250th)Gabi 01273 779520 05-April-99 1085 Fountain Ashurst Auntie Jo Jex 01903 765163 12-April-99 1086 Royal Oak Poynings Rosemary (retirement) 01273 506571 19-April-99 1087 Flight Path Lowfield Heath Simon & Les 01444 232194 26-April-99 1088 Blacksmiths Arms Offham Mudlarks Nigel & Pete 01273 271441 All runs are on Mondays meet at 19.30 for 19.40 start Sschhpi-ell! Well another winter is nearly over and time to put the the old wossnames fading. This information is also available on the hashlights away. Good to see a few more town runs this internet and a hard copy will be given to anyone attending the next time. Gradually hares are getting used to setting shorter Interhash in Tasmania. Registrations go up 1st July so get in quick to runs in the dark and keeping checks short in built-up areas. avoid a hefty increase. Should mean a few short fast runs come BST! I have masses of material for the trash which is ready to be put in but Good luck to any idiots out there doing the London I may have to step down for a while come the summer. -

Millian Liberalism and Extreme Pornography
Millian Liberalism and Extreme Pornography Nick Cowen King’s College London Abstract: How sexuality should be regulated in a liberal political community is an important, controversial theoretical and empirical question—as shown by the recent criminalization of possession of some adult pornography in the United Kingdom. Supporters of criminalization argue that Mill, often considered a staunch opponent of censorship, would support prohibition due to his feminist commitments. I argue that this account underestimates the strengths of the Millian account of private conduct and free expression, and the consistency of Millian anticensorship with feminist values. A Millian contextual defense of liberty, however, suggests several other policy approaches to addressing the harms of pornography. hatplacedoespornographyhaveinaliberal sexual penetration; acts that appear to threaten a person’s society?1 Williams (1979), in his role as life; acts that inflict serious harm on the breasts, geni- W chair of the British Home Office Committee talia, or anus; and acts of necrophilia and bestiality. While on Obscenity and Film Censorship, famously bound many images falling under this definition offend and dis- Mill’s harm principle to a defense of pornography, and turb people, liberal opponents are concerned that the Millian thought has been central to this debate ever prohibition includes fictional representations, in particu- since. Some feminist critics of pornography offer a new lar, depictions of common sexual fantasy scenarios (Joyal, pro-censorship Millian account, supported by Mill’s Cossette, and Lapierre 2015), as well as a range of sex acts commitments to women’s emancipation and aversion to that may appear subjectively dangerous or degrading, but humanity’s animalistic sexual appetites (McGlynn and are safe and frequently enjoyed when practiced between Rackley 2009; McGlynn and Ward 2014). -
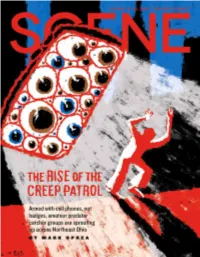
Scene 081220 PROOF1.Pdf
clevescene.com MEDICAL MARIJUANA CARDS BE FREE FROM • For Medical Marijuana Cards DRUG & Treatment Plans • Cards available same day! ADDICTION COMPASSIONATE BOARD CERTIFIED MD MIDDLEBURG HEIGHTS Suboxone Clinic WELLNESS CENTER 440-580-4998 2 | clevescene.com | August 12-18, 2020 | clevescene.com | August 12-18, 2020 3 CONTENTSO AUGUST 12-18, 2020 • VOL. 52 N 6 Upfront ............................................ 5 Music ............................................. 25 Feature ............................................ 8 Savage Love ................................. 26 Eat .................................................. 21 REWIND: i977 Dedicated to Free Times founder Richard H. Siegel (1935-1993) Euclid Media Group and Scene founder Richard Kabat Chief Executive Officer Andrew Zelman Chief Operating Officers Chris Keating, Michael Wagner Publisher Andrew Zelman VP Digital Services Stacy Volhein Forty-three years ago, Editor Vince Grzegorek Digital Operations Coordinator Jaime Monzon The Raspberries’ Eric Editorial www.euclidmediagroup.com Music Editor Jeff Niesel Carmen merited a two- Senior Writer Sam Allard National Advertising Staff Writer Brett Zelman Voice Media Group part interview feature in Dining Editor Douglas Trattner 1-800-278-9866, vmgadvertising.com Visual Arts Writer Shawn Mishak these humble pages. Stage Editor Christine Howey Cleveland Scene Copy Editor Elaine Cicora 737 Bolivar Rd., #4100 Advertising Cleveland, OH 44115 Senior Multimedia Account Executive www.clevescene.com John Crobar, Shayne Rose Phone 216-241-7550 -

A Brief Amicus Curiae
In the Case of Lyle v. Warner Bros. Television Productions, et. al.: A Brief Amicus Curiae Prof. Russell K. Robinson* INTRODUCTION I wrote this amicus brief in connection with the California Su- preme Court's review of Lyle v. Warner Bros. Television.1 Thirteen other law professors from several elite law schools joined the brief. As a writer's assistant for the hit television sitcom Friends,Amaani Lyle was charged with recording the conversations in the writers' room and producing a transcript, which would sometimes lead to jokes and plots for the sitcom. In this position, Lyle alleges, she was routinely subjected to crude sexual conduct and expression in violation of Cali- fornia's Fair Housing and Employment Act, which bans various forms of discrimination, including verbal sexual harassment.2 The Respon- dents, including Friends writers who were Lyle's supervisors, argue that their crude sexual conduct was an indispensable means of developing gags, dialogue and story lines for Friends, which depicts the lives of sexually active adults. This case attracted my attention because it involves several diffi- cult and interesting legal issues that have rarely been addressed by * Acting Professor, UCLA School of Law. The author would like to thank Kimberl6 Crenshaw, Adam B. Wolf and Noah Zatz for critical encouragement and advice in writing this brief. I am also very grateful to the following professors who decided to join the brief: Cynthia G. Bowman, Devon Carbado, Kimberl Crenshaw, Laura Gomez, Cheryl Harris, Kenneth L. Karst, Charles J. Ogletree, Deborah L. Rhode, Dorothy E. Roberts, Leti Volpp, Adam Winkler, Kimberly A. -

Everything In
University of Texas at El Paso ScholarWorks@UTEP Open Access Theses & Dissertations 2020-01-01 Everything In Greg Chavez University of Texas at El Paso Follow this and additional works at: https://scholarworks.utep.edu/open_etd Part of the Creative Writing Commons Recommended Citation Chavez, Greg, "Everything In" (2020). Open Access Theses & Dissertations. 3149. https://scholarworks.utep.edu/open_etd/3149 This is brought to you for free and open access by ScholarWorks@UTEP. It has been accepted for inclusion in Open Access Theses & Dissertations by an authorized administrator of ScholarWorks@UTEP. For more information, please contact [email protected]. EVERYTHING IN GREG CHAVEZ Master’s Program in Creative Writing APPROVED: Sylvia Aguilar-Zéleny, MH, MFA, Chair Jeffrey Sirkin, Ph.D. Annika Mann, Ph.D. Stephen L. Crites, Jr., Ph.D. Dean of the Graduate School Copyright © by Greg Chavez 2020 EVERYTHING IN by GREG CHAVEZ, B.A. THESIS Presented to the Faculty of the Graduate School of The University of Texas at El Paso in Partial Fulfillment of the Requirements for the Degree of MASTER OF FINE ARTS Department of Creative Writing THE UNIVERSITY OF TEXAS AT EL PASO December 2020 Acknowledgements I wish to express my sincerest gratitude for the entire creative writing community at UTEP. Your invaluable feedback and encouragement along the way has helped guide my writing into and out of spaces it had feared to tread. Special thanks to all my UTEP professors who challenged me to see writing and literature from perspectives never imagined. To my thesis committee, Professor Sylvia Aguilar-Zéleny, Dr. Jeffrey Sirkin, and Dr. -

Feminism & Psychology
Feminism & Psychology http://fap.sagepub.com/ Vegan Sexuality: Challenging Heteronormative Masculinity through Meat-free Sex Annie Potts and Jovian Parry Feminism & Psychology 2010 20: 53 DOI: 10.1177/0959353509351181 The online version of this article can be found at: http://fap.sagepub.com/content/20/1/53 Published by: http://www.sagepublications.com Additional services and information for Feminism & Psychology can be found at: Email Alerts: http://fap.sagepub.com/cgi/alerts Subscriptions: http://fap.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav Citations: http://fap.sagepub.com/content/20/1/53.refs.html >> Version of Record - Feb 15, 2010 What is This? Downloaded from fap.sagepub.com at UNIV CALIFORNIA IRVINE on January 4, 2012 Annie POTTS and Jovian PARRY Vegan Sexuality: Challenging Heteronormative Masculinity through Meat-free Sex The terms ‘vegansexuality’ and ‘vegansexuals’ entered popular discourse following sub- stantial media interest in a New Zealand-based academic study on ethical consumption that noted that some vegans engaged in sexual relationships and intimate partnerships only with other vegans. At this time it was suggested that a spectrum existed in rela- tion to cruelty-free consumption and sexual relationships: at one end of this spectrum, a form of sexual preference influenced by veganism entailed an increased likelihood of sexual attraction towards those who shared similar beliefs regarding the exploitation of non-human animals; at the other end of the spectrum such a propensity might manifest as a strong sexual aversion to the bodies of those who consume meat and other animal products. -

Developmental Characteristics of Interspecific Hybrid Embryos
DEVELOPMENTAL CHARACTERISTICS OF INTERSPECIFIC HYBRID EMBRYOS A Thesis Presented to The Faculty of Graduate Studies of The University of Guelph bv DAWN A. KELK In partial fulfilLment of requkements for the degree of Doctor of Philosophy Jdy, 1997 Bibbaièque nationale du Canada Acquisitions and Acquisitions et Bibliographie Services senrices bibliographiques 395 Wellington Street 395. rue Wemgtcm ût&waON KlAW Otlawa ON KIA ON4 Canada canada The author bas granted a non- L'auteur a accordé une licence non exclusive licence allowing the exclusive pamettant à la National L&rary of Canada to Bibliothèque nationale du Canada de reproduce, loan, disîriiuîe or sell reproduire, prêter, distribuer ou copies of this thesis in microfonn, vendre des copies de cette thèse sous paper or electronic formats. ia forme de microfiche/fï?m, de reproduction sur papier ou sur fonnat électronique. The author retains ownership of the L'auteur conserve la propriété du copyright in this thesis. Neitha the droit d'auteur qui protège cette thèse. thesis nor substantial extracts hmit Ni la thèse ni des extraits substantiels may be printed or otherwise de cebci ne doivent être imwés reproduced without the author's ou autrement reproduits sans son permission. autorisation, DEVnOPMENTAL CHARACTERISTICS OF INTERSPECIFIC HYBRID EMBRYOS Dawn A. Kelk Advisor: University of Guelph, 1997 Dr. W. A. King Establishment of an embryo capable of development to term involves precisely regdated nudear and cytoplasmic events. Interspeefic hybrids provide unique emb ryo models with morpho logical, b iochemical and temporal markers of development which enable investigation of these interactions. This study explores the feasibility of producing and utilizing interspecific hybrid embryos of cattle, sheep and goats as models to examine the respective roles of the maternd and patemal contributions to the embryo and the interactions of the nucleus and cytoplasm. -

Prose in Poor Taste
PRO SE IN PO O R TA STE Editors Ben John Smith ~ Arthur Graham Copyright © 2017 by Horror Sleaze Trash ISB N -13: 978-1975745523 IS B N -1 0 : 19 7 5 7 4 5 5 2 3 /is book is a work of 3ction. Names, characters, business organizations, places, events, and incidents either are the product of the authors’ im agination or are used 3ctitiously. /e use of nam es of actual persons (living or dead), places, and characters is incidental to the purposes of the plot, and is not intended to change the entirely 3c tio n a l c h a ra c te r o f th e w o rk . No part of this work may be reproduced, stored in a retrieval system , o r tran sm itted b y an y m ean s w ith o u t the w ritten perm ission of the authors or publisher, with the exception of short excerpts used in articles and critical review s. Foreword HST isn’t run w ith any real sense of consistency or urgency. O r professionalism for that fucking m atter. It’s run from the oddity-crow ded spare room in a house in W estmeadow s, M elbourne. It’s ran w ith a scream ing one year old running dow n the hallw ay banging on a pot lid with a wooden spoon. It’s ran in conjunction w ith a full-tim e job as a sandblaster w ith a m ortgage. It’s patched together w ith saliva and claret. -

Evolutionary Ecology of Mammalian Placental Invasiveness
EVOLUTIONARY ECOLOGY OF MAMMALIAN PLACENTAL INVASIVENESS Michael G. Elliot M.A., University of Oxford, 1998 THESIS SUBMITTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE In the Department of Biological Sciences O Michael G. Elliot 2007 SIMON FRASER UNIVERSITY Fa11 2007 All rights reserved. This work may not be reproduced in whole or in part, by photocopy OF other means, without permission of the author. APPROVAL Name: Michael G. Elliot Degree: Master of Science Title of Thesis: Evolutionary ecology of mammalian placental invasiveness Examining Committee: Chair: Dr. R. Ydenberg, Professor Dr. B. Crespi, Professor, Senior Supervisor Department of Biological Sciences, S.F.U. Dr. A. Mooers, Associate Professor Department of Biological Sciences, S.F.U. Dr. T. Williams, Professor Department of Biological Sciences, S.F.U. Dr. J. Reynolds, Professor Department of Biological Sciences, S.F.U. Public Examiner 4 December Date Approved Declaration of Partial Copyright Licence The author, whose copyright is declared on the title page of this work, has granted to Simon Fraser University the right to lend this thesis, project or extended essay to users of the Simon Fraser University ~ibrary,and to make partial or single copies only for such users or in response to a request from the library of any other university, or other educational institution, on its own behalf or for one of its users. The author has further granted permission to Simon Fraser University to keep or make a digital copy for use in its circulating collection (currently available to the public at the 'Institutional Repositoryn link of the SFU Library website <www.lib.sfu.ca> at: <http://ir.lib.sfu.ca/handle/l892/112>) and, without changing the content, to translate the thesislproject or extended essays, if technically possible, to any medium or format for the purpose of preservation of the digital work. -

Allogeneic Component to Overcome Rejection in Interspecific Pregnancy Mikael Häggström1
WikiJournal of Medicine, 2014, 1(1) doi: 10.15347/wjm/2014.004 Figure Article Allogeneic component to overcome rejection in interspecific pregnancy Mikael Häggström1 Introduction Interspecific pregnancy is a pregnancy involving an embryo or fetus belonging to another species than the carrier. The embryo or fetus is called xenoge- neic (the prefix xeno- denotes something from another species), and would be equivalent to a xenograft rather than an allograft, putting a higher demand on gestational immune tolerance in order to avoid an immune reaction toward the fetus. Methods to over- come rejection of the xenogeneic embryo or fetus in- clude the following two: Intercurrently inserting an allogeneic (allo- denotes some- thing from the same species) embryo into the uterus in ad- dition to the xenogeneic one. For example, embryos of the species Spanish Ibex are aborted when inserted alone into the womb of a goat, but when introduced together with a goat embryo, they may develop to term.[1] Covering the outer layer of a xenogeneic embryo with al- logeneic cells. Such envelopment can be created by first isolating the inner cells mass of blastocysts of the species to be reproduced by immunosurgery, wherein the blasto- cyst is exposed to antibodies toward that species. Be- cause only the outer layer, that is, the trophoblastic cells, are exposed to the antibodies, only these cells will be de- stroyed by subsequent exposure to complement. The re- maining inner cell mass can be injected into a blastocele of the recipient species to acquire its tropho- blastic cells.[2] As an example of this method, embryos of Ryuku Mouse(Mus caroli) will survive to term inside the uterus of a house mouse (Mus musculus) only if enveloped in Mus musculus trophoblast cells.[3] Both of these methods involve a xenogeneic pregnancy in addition to an allogeneic component, that is, either a separate allogeneic embryo or an allogeneic tropho- blast.