Pathophysiological Mechanisms in Antiphospholipid Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Remote Ischemic Preconditioning (RIPC) Modifies Plasma Proteome in Humans
Remote Ischemic Preconditioning (RIPC) Modifies Plasma Proteome in Humans Michele Hepponstall1,2,3,4, Vera Ignjatovic1,3, Steve Binos4, Paul Monagle1,3, Bryn Jones1,2, Michael H. H. Cheung1,2,3, Yves d’Udekem1,2, Igor E. Konstantinov1,2,3* 1 Haematology Research, Murdoch Childrens Research Institute; Melbourne, Victoria, Australia, 2 Cardiac Surgery Unit and Cardiology, Royal Children’s Hospital; Melbourne, Victoria, Australia, 3 Department of Paediatrics, The University of Melbourne; Melbourne, Victoria, Australia, 4 Bioscience Research Division, Department of Primary Industries, Melbourne, Victoria, Australia Abstract Remote Ischemic Preconditioning (RIPC) induced by brief episodes of ischemia of the limb protects against multi-organ damage by ischemia-reperfusion (IR). Although it has been demonstrated that RIPC affects gene expression, the proteomic response to RIPC has not been determined. This study aimed to examine RIPC induced changes in the plasma proteome. Five healthy adult volunteers had 4 cycles of 5 min ischemia alternating with 5 min reperfusion of the forearm. Blood samples were taken from the ipsilateral arm prior to first ischaemia, immediately after each episode of ischemia as well as, at 15 min and 24 h after the last episode of ischemia. Plasma samples from five individuals were analysed using two complementary techniques. Individual samples were analysed using 2Dimensional Difference in gel electrophoresis (2D DIGE) and mass spectrometry (MS). Pooled samples for each of the time-points underwent trypsin digestion and peptides generated were analysed in triplicate using Liquid Chromatography and MS (LC-MS). Six proteins changed in response to RIPC using 2D DIGE analysis, while 48 proteins were found to be differentially regulated using LC-MS. -
Pancancer Progression Human Vjune2017
Gene Symbol Accession Alias/Prev Symbol Official Full Name AAMP NM_001087.3 - angio-associated, migratory cell protein ABI3BP NM_015429.3 NESHBP|TARSH ABI family, member 3 (NESH) binding protein ACHE NM_000665.3 ACEE|ARACHE|N-ACHE|YT acetylcholinesterase ACTG2 NM_001615.3 ACT|ACTA3|ACTE|ACTL3|ACTSG actin, gamma 2, smooth muscle, enteric ACVR1 NM_001105.2 ACTRI|ACVR1A|ACVRLK2|ALK2|FOP|SKR1|TSRI activin A receptor, type I ACVR1C NM_145259.2 ACVRLK7|ALK7 activin A receptor, type IC ACVRL1 NM_000020.1 ACVRLK1|ALK-1|ALK1|HHT|HHT2|ORW2|SKR3|TSR-I activin A receptor type II-like 1 ADAM15 NM_207195.1 MDC15 ADAM metallopeptidase domain 15 ADAM17 NM_003183.4 ADAM18|CD156B|CSVP|NISBD|TACE ADAM metallopeptidase domain 17 ADAM28 NM_014265.4 ADAM 28|ADAM23|MDC-L|MDC-Lm|MDC-Ls|MDCL|eMDC II|eMDCII ADAM metallopeptidase domain 28 ADAM8 NM_001109.4 CD156|MS2 ADAM metallopeptidase domain 8 ADAM9 NM_001005845.1 CORD9|MCMP|MDC9|Mltng ADAM metallopeptidase domain 9 ADAMTS1 NM_006988.3 C3-C5|METH1 ADAM metallopeptidase with thrombospondin type 1 motif, 1 ADAMTS12 NM_030955.2 PRO4389 ADAM metallopeptidase with thrombospondin type 1 motif, 12 ADAMTS8 NM_007037.4 ADAM-TS8|METH2 ADAM metallopeptidase with thrombospondin type 1 motif, 8 ADAP1 NM_006869.2 CENTA1|GCS1L|p42IP4 ArfGAP with dual PH domains 1 ADD1 NM_001119.4 ADDA adducin 1 (alpha) ADM2 NM_001253845.1 AM2|dJ579N16.4 adrenomedullin 2 ADRA2B NM_000682.4 ADRA2L1|ADRA2RL1|ADRARL1|ALPHA2BAR|alpha-2BAR adrenoceptor alpha 2B AEBP1 NM_001129.3 ACLP AE binding protein 1 AGGF1 NM_018046.3 GPATC7|GPATCH7|HSU84971|HUS84971|VG5Q -
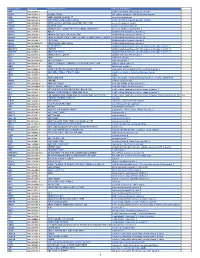
Supporting Information for Proteomics DOI 10.1002/Prca.200780101
Supporting Information for Proteomics DOI 10.1002/prca.200780101 Paul Cutler, Emma L. Akuffo, Wanda M. Bodnar, Deborah M. Briggs, John B. Davis, Christine M. Debouck, Steven M. Fox, Rachel A. Gibson, Darren A. Gormley, Joanna D. Holbrook, A. Jacqueline Hunter, Emma E. Kinsey, Rabinder Prinjha, Jill C. Richardson, Allen D. Roses, Marjorie A. Smith, Nikos Tsokanas, David R. Will, Wen Wu, John W. Yates and Israel S. Gloger Proteomic identification and early validation of complement 1 inhibitor and pigment epithelium-derived factor: Two novel biomarkers of Alzheimer’s disease in human plasma ª 2007 WILEY-VCH Verlag GmbH & Co. KGaA, Weinheim www.clinical.proteomics-journal.com Supplementary Table 1: Complete list of proteins identified from spots derived from 2D gel analysis of human plasma. Each protein was observed to be in a spot showing altered expression between Alzheimer’s disease and matched control by statistical methods as described in the Methods section. Each protein is identified by the gene description and the HUGO gene symbol. The number of “changing” spots in which this protein was observed is also given. HUGO Human Gene Number of Gene Description Symbol Spots alpha-1-B glycoprotein; A1BG 5 alpha-2-macroglobulin A2M 7 afamin; AFM 1 angiotensinogen (serpin peptidase inhibitor, clade A, member 8) AGT 4 alpha-2-HS-glycoprotein AHSG 3 albumin ALB 90 alpha-1-microglobulin/bikunin precursor; AMBP 1 annexin A1 ANXA1 1 amyloid P component, serum APCS 3 apolipoprotein A-I APOA1 14 apolipoprotein A-IV APOA4 2 apolipoprotein E APOE 2 apolipoprotein -

Apolipoprotein H, an Acute Phase Protein, a Performing Tool for Ultra-Sensitive Detection and Isolation of Microorganisms from Different Origins
2 Apolipoprotein H, an Acute Phase Protein, a Performing Tool for Ultra-Sensitive Detection and Isolation of Microorganisms from Different Origins Ilias Stefas1, Gregor Dubois2, Sylvia Tigrett1, Estelle Lucarz1 and Francisco Veas2 1ApoH-Technologies Faculty of Pharmacy, University Montpellier 1, Av Charles Flahault, Montpellier 2Comparative Molecular Immuno-Physiopathology Lab. UMR-MD3 Faculty of Pharmacy, University Montpellier 1, Av Charles Flahault, Montpellier France 1. Introduction Apolipoprotein H (ApoH), also known as beta2-glycoprotein I (ß2-GPI), is a plasma glycoprotein of 50 kDa. ApoH is present in human plasma at a concentration of between 150 and 300 mg/ml (Bouma et al., 1999). In blood, ApoH circulate in free conformations or bound to lipoproteins: chylomicrons, very low-density lipoprotein (VLDL), low density lipoprotein (LDL) and high-density lipoprotein (HDL). In addition, ApoH has a high affinity for triglyceride-rich lipoproteins. The amount of ApoH associated with plasma lipoproteins in healthy individuals varies according to the authors from 4 to 13% (Gambino et al., 1999a) up to about 40% (Polz & Kostner, 1979). ApoH is able to activate lipoprotein lipases (Lee et al., 1983). ApoH was isolated from the fraction of plasma lipoproteins, and described for the first time in 1961 by H. Schultze E (Schultze, 1961). In a lesser extent, ApoH is also associated to ß2-globulin fraction. ApoH is expressed in human liver, in intestinal cells and tissues (Averna et al., 1997). In rats, other sites of synthesis in low concentrations were identified as the kidney, small intestine, brain, cardiomyocytes of the heart, and at even lower in the spleen, stomach and prostate (Ragusa et al., 2006). -

Review Article Mouse Homologues of Human Hereditary Disease
I Med Genet 1994;31:1-19 I Review article J Med Genet: first published as 10.1136/jmg.31.1.1 on 1 January 1994. Downloaded from Mouse homologues of human hereditary disease A G Searle, J H Edwards, J G Hall Abstract involve homologous loci. In this respect our Details are given of 214 loci known to be genetic knowledge of the laboratory mouse associated with human hereditary dis- outstrips that for all other non-human mam- ease, which have been mapped on both mals. The 829 loci recently assigned to both human and mouse chromosomes. Forty human and mouse chromosomes3 has now two of these have pathological variants in risen to 900, well above comparable figures for both species; in general the mouse vari- other laboratory or farm animals. In a previous ants are similar in their effects to the publication,4 102 loci were listed which were corresponding human ones, but excep- associated with specific human disease, had tions include the Dmd/DMD and Hprt/ mouse homologues, and had been located in HPRT mutations which cause little, if both species. The number has now more than any, harm in mice. Possible reasons for doubled (table 1A). Of particular interest are phenotypic differences are discussed. In those which have pathological variants in both most pathological variants the gene pro- the mouse and humans: these are listed in table duct seems to be absent or greatly 2. Many other pathological mutations have reduced in both species. The extensive been detected and located in the mouse; about data on conserved segments between half these appear to lie in conserved chromo- human and mouse chromosomes are somal segments. -

Assessing Changes in Biomarkers of Effect in Smokers Who Switch to a Closed System Electronic Cigarette
Assessing Changes In Biomarkers Of Effect In Smokers Who Switch To A Closed System Electronic Cigarette Liz Mason | Kunming, China | 26th October 2018 CONTENT 1. Background Biomarkers of exposure and effect Study Aim 2. 5-day Study Study design Results 3. Two-year study Study design Results 4. Summary Study Conclusions Background 5-day Study Two year study Conclusions 2 | VAPOUR PRODUCTS HAVE BEEN SHOWN TO REDUCE BIOMARKERS OF EXPOSURE Previous studies have demonstrated that when a smoker switches to a vapour product, they are exposed to significantly lower levels of carcinogens and toxicants in the aerosol... Reduced formation of toxicants in blu™ e-cigarette …and significant reductions in biomarkers of exposure… aerosol vs. conventional cigarette smoke “Chemical Composition of myblu™ Pod-System E-Cigarette Aerosols: A Quantitative Comparison with Conventional Cigarette Smoke”, Poster presentation, 1st Scientific Summit Tobacco Harm Reduction (http://www.fontemscience.com/wp-content/uploads/2018/06/2018-04-18-aerosol-chemistry-thr-summit-2018-poster_final.pdf); Tayyarah R and Long GA. “Comparison of select analytes in aerosol from e-cigarettes with smoke from conventional cigarettes and with ambient air.” Regulatory toxicology and pharmacology 70 3 (2014). O’Connell et al (2016): Reductions in biomarkers of exposure (BoE) to harmful or potentially harmful constituents (HPHCs) following partial or complete substitution of cigarettes with electronic cigarettes in adult smokers, Toxicology Mechanisms and Methods, DOI: 10.1080/15376516.2016.1196282. http://www.fontemscience.com/wp-content/uploads/2017/05/fontem2research-1.pdf Background 5-day Study Two year study Conclusions 3 | VAPOUR PRODUCTS HAVE BEEN SHOWN TO REDUCE BIOMARKERS OF EXPOSURE What is the biological impact when a smoker switches to a vapour product? Clinical markers: • can be defined as a measurable biochemical, physiologic, behavioural, or other alteration in an organism. -

A Novel Mechanism of Thrombosis in Antiphospholipid Antibody Syndrome
Vlachoyiannopoulos PG, Routsias JG. Ένας νέος μηχανισμός για την θρόμβωση στο σύνδρομο αντιφωσφολιπιδίων. J Autoimmun. 2010, 35(3):248-55. Antiphospholipid antibody syndrome (APS) is an autoimmune thrombophilia mediated by autoantibodies directed against phospholipid‐binding plasma proteins, mainly β2 Glycoprotein I (β2GPI)‐ a plasma apolipoprotein and prothrombin (PT). A subgroup of these antibodies termed "Lupus Anticoagulant" (LA) elongate in vitro the clotting times, this elongation not corrected by adding normal plasma in the detection system. The exact mechanism by which these autoantibodies induce thrombosis is not well understood. Resistance to natural anticoagulants such as protein C, impaired fibrinolysis, activation of endothelial cells to a pro‐coagulant phenotype and activation of platelets, are among the mechanisms partially supported by experimental evidence. Artificially dimerized β2GPI binds tightly to platelet membrane activating them. We search for mechanisms of natural dimerization of β2GPI by proteins of the platelet membranes and found that platelet factor 4 (PF4) assembled in homotetramers binds two molecules of β2GPI and this complex is recognized by anti‐β2GPI antibodies, the whole complexes being thrombogenic in terms of activating platelets as confirmed by p38MAP kinase phosphorylation and thromboxane B2 production. Of note PF4/heparin complexes are also immunogenic triggering the production of anti‐PF4/heparin antibodies which activate also platelets (the so‐called "heparin‐induced thrombocytopenia and thrombosis syndrome", HITT). The anti‐β2GPI antibodies activate platelets by their F(ab)2, while the anti‐PF4/heparin by their Fc fragments. Thus PF4 is a common denominator in the pathogenesis of APS and HITT which share also clinical characteristics such as thrombocytopenia and thrombosis. -

Strand Breaks for P53 Exon 6 and 8 Among Different Time Course of Folate Depletion Or Repletion in the Rectosigmoid Mucosa
SUPPLEMENTAL FIGURE COLON p53 EXONIC STRAND BREAKS DURING FOLATE DEPLETION-REPLETION INTERVENTION Supplemental Figure Legend Strand breaks for p53 exon 6 and 8 among different time course of folate depletion or repletion in the rectosigmoid mucosa. The input of DNA was controlled by GAPDH. The data is shown as ΔCt after normalized to GAPDH. The higher ΔCt the more strand breaks. The P value is shown in the figure. SUPPLEMENT S1 Genes that were significantly UPREGULATED after folate intervention (by unadjusted paired t-test), list is sorted by P value Gene Symbol Nucleotide P VALUE Description OLFM4 NM_006418 0.0000 Homo sapiens differentially expressed in hematopoietic lineages (GW112) mRNA. FMR1NB NM_152578 0.0000 Homo sapiens hypothetical protein FLJ25736 (FLJ25736) mRNA. IFI6 NM_002038 0.0001 Homo sapiens interferon alpha-inducible protein (clone IFI-6-16) (G1P3) transcript variant 1 mRNA. Homo sapiens UDP-N-acetyl-alpha-D-galactosamine:polypeptide N-acetylgalactosaminyltransferase 15 GALNTL5 NM_145292 0.0001 (GALNT15) mRNA. STIM2 NM_020860 0.0001 Homo sapiens stromal interaction molecule 2 (STIM2) mRNA. ZNF645 NM_152577 0.0002 Homo sapiens hypothetical protein FLJ25735 (FLJ25735) mRNA. ATP12A NM_001676 0.0002 Homo sapiens ATPase H+/K+ transporting nongastric alpha polypeptide (ATP12A) mRNA. U1SNRNPBP NM_007020 0.0003 Homo sapiens U1-snRNP binding protein homolog (U1SNRNPBP) transcript variant 1 mRNA. RNF125 NM_017831 0.0004 Homo sapiens ring finger protein 125 (RNF125) mRNA. FMNL1 NM_005892 0.0004 Homo sapiens formin-like (FMNL) mRNA. ISG15 NM_005101 0.0005 Homo sapiens interferon alpha-inducible protein (clone IFI-15K) (G1P2) mRNA. SLC6A14 NM_007231 0.0005 Homo sapiens solute carrier family 6 (neurotransmitter transporter) member 14 (SLC6A14) mRNA. -

Serum Acute Phase Reactants Hallmark Healthy Individuals at Risk For
Borlak et al. Genome Medicine 2013, 5:86 http://genomemedicine.com/content/5/9/86 RESEARCH Open Access Serum acute phase reactants hallmark healthy individuals at risk for acetaminophen-induced liver injury Jürgen Borlak1*, Bijon Chatterji1, Kishor B Londhe1 and Paul B Watkins2 Abstract Background: Acetaminophen (APAP) is a commonly used analgesic. However, its use is associated with drug-induced liver injury (DILI). It is a prominent cause of acute liver failure, with APAP hepatotoxicity far exceeding other causes of acute liver failure in the United States. In order to improve its safe use this study aimed to identify individuals at risk for DILI prior to drug treatment by searching for non-genetic serum markers in healthy subjects susceptible to APAP-induced liver injury (AILI). Methods: Healthy volunteers (n = 36) received either placebo or acetaminophen at the maximum daily dose of 4 g for 7 days. Blood samples were taken prior to and after APAP treatment. Serum proteomic profiling was done by 2D SDS-PAGE and matrix-assisted laser desorption/ionization-time of flight-mass spectrometry. Additionally, the proteins C-reactive protein, haptoglobin and hemopexin were studied by quantitative immunoassays. Results: One-third of study subjects presented more than four-fold increased alanine transaminase activity to evidence liver injury, while serum proteomics informed on 20 proteins as significantly regulated. These function primarily in acute phase and immune response. Pre-treatment associations included C-reactive protein, haptoglobin isoforms and retinol binding protein being up to six-fold higher in AILI susceptible individuals, whereas alpha1-antitrypsin, serum amyloid A, kininogen and transtyretin were regulated by nearly five-fold in AILI responders. -

Candidate Genes and Proteomic Biomarkers of Serum and Urine in Medication-Overuse Headache
International Journal of Molecular Sciences Review Candidate Genes and Proteomic Biomarkers of Serum and Urine in Medication-Overuse Headache Natalia A. Shnayder 1,2,* , Victoria B. Sharavii 3,* , Marina M. Petrova 2, Polina V. Moskaleva 2 , Elena A. Pozhilenkova 2, Darya S. Kaskaeva 2, Olga. V. Tutynina 2, Tatiana E. Popova 4, Natalia P. Garganeeva 5 and Regina F. Nasyrova 1 1 The Center of Personalized Psychiatry and Neurology, V. M. Bekhterev National Medical Research Center for Neurology and Psychiatry, 192019 Saint-Petersburg, Russia; [email protected] 2 The Center of Collective Usage “Molecular and Cell Technologies”, V. F. Voino-Yasenetsky Krasnoyarsk State Medical University, 660022 Krasnoyarsk, Russia; [email protected] (M.M.P.); [email protected] (P.V.M.); [email protected] (E.A.P.); [email protected] (D.S.K.); [email protected] (O.V.T.) 3 The International School Medicine of the Future, I. M. Sechenov First Moscow State Medical University (Sechenov University), 119991 Moscow, Russia 4 The Yakutsk Scientific Center for Complex Medicine Problems, The Department of Epidemiology of Non-Infectious Diseases, 677018 Yakutsk, Russia; [email protected] 5 The Department of General Medical Practice and Polyclinic Therapy, The Siberian State Medical University, 634050 Tomsk, Russia; [email protected] * Correspondence: [email protected] (N.A.S.); [email protected] (V.B.S.); Tel.: +7-(812)-620-02-20 (N.A.S.); +7-994-002-9712 (V.B.S.) Citation: Shnayder, N.A.; Sharavii, Abstract: Chronic headache is a topical problem of neurology, psychiatry and general practice. The V.B.; Petrova, M.M.; Moskaleva, P.V.; medication-overuse headache (MOH) is one of the leading pathologies in the structure of chronic Pozhilenkova, E.A.; Kaskaeva, D.S.; headache. -

The Application of Multiple Reaction Monitoring and Multi-Analyte
Yassine et al. Lipids in Health and Disease 2014, 13:8 http://www.lipidworld.com/content/13/1/8 RESEARCH Open Access The application of multiple reaction monitoring and multi-analyte profiling to HDL proteins Hussein N Yassine1*, Angela M Jackson2, Chad R Borges3, Dean Billheimer4, Hyunwook Koh1, Derek Smith3, Peter Reaven5, Serrine S Lau6 and Christoph H Borchers2,7 Abstract Background: HDL carries a rich protein cargo and examining HDL protein composition promises to improve our understanding of its functions. Conventional mass spectrometry methods can be lengthy and difficult to extend to large populations. In addition, without prior enrichment of the sample, the ability of these methods to detect low abundance proteins is limited. Our objective was to develop a high-throughput approach to examine HDL protein composition applicable to diabetes and cardiovascular disease (CVD). Methods: We optimized two multiplexed assays to examine HDL proteins using a quantitative immunoassay (Multi-Analyte Profiling- MAP) and mass spectrometric-based quantitative proteomics (Multiple Reaction Monitoring-MRM). We screened HDL proteins using human xMAP (90 protein panel) and MRM (56 protein panel). We extended the application of these two methods to HDL isolated from a group of participants with diabetes and prior cardiovascular events and a group of non-diabetic controls. Results: We were able to quantitate 69 HDL proteins using MAP and 32 proteins using MRM. For several common proteins, the use of MRM and MAP was highly correlated (p < 0.01). Using MAP, several low abundance proteins implicated in atherosclerosis and inflammation were found on HDL. On the other hand, MRM allowed the examination of several HDL proteins not available by MAP. -

Technology for Proteomics Translation to Clinical Research
TechnologyTechnology ForFor ProteomicsProteomics Translation to Clinical ResearchResearch StudiesStudies Lance A. Liotta MD PhD George Mason University A. Novel one step preservative for tissue phosphoproteins B. Protein Microarrays: 200 signal pathway phosphoproteins -Translation to clinical research trials -The universal tissue preservative: obviate frozen storage C. Smart nanoparticles for one step in-solution molecular size sieving, affinity capture, biomarker preservation and amplification of effective sensitivity. The Center for Applied Proteomics and M ole cular Medicine Proteomics Tools for Clinical Medicine There is a need to measure the state of activity of the actual drug targets (the proteins) in a patient’s individual cancer. Patient A Patient B Proteomics is the missing link for designing individualized therapies Concurrent phosphorylation of kinases and kinase substrates indicates functional linkage “Proteins carry the epigenetic marks and information” Emma Whitelaw, DISCOVER Nov. 2006 Genetic or epigenetic defects are selected during cancer progression because they cooperate to orchestrate alterations in protein networks generating a survival advantage for the target cell. Post-translational modifications, such as phosphorylation, reflect the activity state of cellular signaling networks. Patterns of phosphorylation indicate docking events and infer protein-protein interactions. Pre‐analytical Variables: The tissue is alive! •The tissue is alive and reactive post excision • During the post excision delay time, tissue signal