Australasian Anaesthesia 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Model for Mandatory Job Safety Analysis Embedded in the Premit-To-Work System >
International Gas Union Research Conference 2011 <A MODEL FOR MANDATORY JOB SAFETY ANALYSIS EMBEDDED IN THE PREMIT-TO-WORK SYSTEM > Main author I. K. Yoon KOREA ABSTRACT Permit to Work (PTW) systems is defined as "a formal documented system used to control the certain types of work that are potentially hazardous". Generally, PTW system should be designed to specify the work to be done safely and the precaution to be taken as well as approval, responsibility, permissions of work. For this reason, PTW is regarded as one of the most important safety management system to control the risk of maintenance that causes 30% of the accident in chemical industries. In the early days, PTW was based on paper based system. But recently has continued to evolve into a computer based system. And these advanced systems has been applied to 80% of oil industry in North Sea and upgraded with providing the hazard information as well as supporting documentation. Usually, the hazard information is provided in the form of hazard checklist or attached risk assessment report such as JSA sheet. But when we consider the various types of work, place and environment, all the potential work related hazard cannot be reviewed in the form of prescribed checklist or certain attachment. To review the potential hazard perfectly, the work permit should be supported by Job Safety Analysis (JSA). But it has rarely been seen that company have a rule to require the mandatory JSA whenever permit to work is accomplished. Despite a relatively simple analysis structure, it is time-consuming and person-consuming methodology to complete all the procedure. -
Contingency Planning and Change Management
CHapteR 11 CONTINGENCY PLANNING AND CHANGE MANAGEMENT Introduction registration agency; for example: changes in Federal and State laws, budget fluctuations, relocation of Change in a voter registration and elections office is election office, staffing changes, agency reorganiza- inevitable, and effective management requires election tion, etc. Unlike contingencies, change management administrators to develop contingency and change focuses on events the office is already aware of and do management plans to respond to situations in a timely not rise unexpectedly. and effective manner. The goal of this chapter is to provide election officials general guidelines on how to identify, assess, and respond to events that may disrupt Identifying and assessing contingencies and election and voter registration services in their local change factors jurisdictions. The chapter addresses both contingency The first step in developing contingency and change planning and change management as they are inextri- management plans is to identify the contingencies cably linked to each other and may at times be devel- and change factors that can impact election and voter oped concurrently with each other. The goal of both registration practices and procedures in your particular these management plans is to prevent or minimize the community. This process is useful for several reasons. impact of change (expected or unexpected) on election First, it will help you define the goal of either your and voter registration processes, while preserving the contingency or change management plans. Second, it integrity of the electoral system. The recommendations will help you to objectively assess situations and their contained in this chapter should be vetted with Federal, potential impact. -

Personal Protective Equipment Hazard Assessment
WORKER HEALTH AND SAFETY Personal Protective Equipment Hazard Assessment Oregon OSHA Personal Protective Equipment Hazard Assessment About this guide “Personal Protective Equipment Hazard Assessment” is an Oregon OSHA Standards and Technical Resources Section publication. Piracy notice Reprinting, excerpting, or plagiarizing this publication is fine with us as long as it’s not for profit! Please inform Oregon OSHA of your intention as a courtesy. Table of contents What is a PPE hazard assessment ............................................... 2 Why should you do a PPE hazard assessment? .................................. 2 What are Oregon OSHA’s requirements for PPE hazard assessments? ........... 3 Oregon OSHA’s hazard assessment rules ....................................... 3 When is PPE necessary? ........................................................ 4 What types of PPE may be necessary? .......................................... 5 Table 1: Types of PPE ........................................................... 5 How to do a PPE hazard assessment ............................................ 8 Do a baseline survey to identify workplace hazards. 8 Evaluate your employees’ exposures to each hazard identified in the baseline survey ...............................................9 Document your hazard assessment ...................................................10 Do regular workplace inspections ....................................................11 What is a PPE hazard assessment A personal protective equipment (PPE) hazard assessment -

View a Copy of This Licence, Visit Tivecommons.Org/Licenses/By/4.0
Katakami et al. Cardiovasc Diabetol (2020) 19:110 https://doi.org/10.1186/s12933-020-01079-4 Cardiovascular Diabetology ORIGINAL INVESTIGATION Open Access Tofoglifozin does not delay progression of carotid atherosclerosis in patients with type 2 diabetes: a prospective, randomized, open-label, parallel-group comparative study Naoto Katakami1,2* , Tomoya Mita3, Hidenori Yoshii4, Toshihiko Shiraiwa5, Tetsuyuki Yasuda6, Yosuke Okada7, Keiichi Torimoto7, Yutaka Umayahara8, Hideaki Kaneto9, Takeshi Osonoi10, Tsunehiko Yamamoto11, Nobuichi Kuribayashi12, Kazuhisa Maeda13, Hiroki Yokoyama14, Keisuke Kosugi15, Kentaro Ohtoshi16, Isao Hayashi17, Satoru Sumitani18, Mamiko Tsugawa19, Kayoko Ryomoto20, Hideki Taki21, Tadashi Nakamura22, Satoshi Kawashima23, Yasunori Sato24, Hirotaka Watada3 and Iichiro Shimomura1 on behalf of the UTOPIA study investigators Abstract Background: This study aimed to investigate the preventive efects of tofoglifozin, a selective sodium-glucose cotransporter 2 (SGLT2) inhibitor, on atherosclerosis progression in type 2 diabetes (T2DM) patients without apparent cardiovascular disease (CVD) by monitoring carotid intima-media thickness (IMT). Methods: This prospective, randomized, open-label, blinded-endpoint, multicenter, parallel-group, comparative study included 340 subjects with T2DM and no history of apparent CVD recruited at 24 clinical units. Subjects were randomly allocated to either the tofoglifozin treatment group (n 169) or conventional treatment group using drugs other than SGLT2 inhibitors (n 171). Primary outcomes were changes= in mean and maximum common carotid IMT measured by echography during= a 104-week treatment period. Results: In a mixed-efects model for repeated measures, the mean IMT of the common carotid artery (mean- IMT-CCA), along with the right and left maximum IMT of the CCA (max-IMT-CCA), signifcantly declined in both the tofoglifozin ( 0.132 mm, SE 0.007; 0.163 mm, SE 0.013; 0.170 mm, SE 0.020, respectively) and the control group ( 0.140 mm,− SE 0.006; 0.190 mm,− SE 0.012; 0.190 mm,− SE 0.020, respectively). -
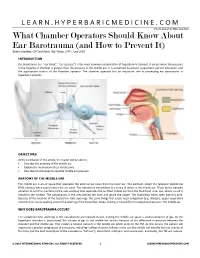
What Chamber Operators Should Know About Ear Barotrauma (And How to Prevent It) Robert Sheffield, CHT and Kevin “Kip” Posey, CHT / June 2018
LEARN.HYPERBARICMEDICINE.COM International ATMO Education What Chamber Operators Should Know About Ear Barotrauma (and How to Prevent It) Robert Sheffield, CHT and Kevin “Kip” Posey, CHT / June 2018 INTRODUCTION Ear barotrauma (i.e. “ear block”, “ear squeeze”) is the most common complication of hyperbaric treatment. It occurs when the pressure in the hyperbaric chamber is greater than the pressure in the middle ear. It is prevented by patient assessment, patient education, and the appropriate actions of the chamber operator. The chamber operator has an important role in preventing ear barotrauma in hyperbaric patients. OBJECTIVES At the conclusion of this article, the reader will be able to: Describe the anatomy of the middle ear Explain the mechanism of ear barotrauma Describe 3 techniques to equalize middle ear pressure ANATOMY OF THE MIDDLE EAR The middle ear is an air space that separates the external ear canal from the inner ear. The eardrum, called the tympanic membrane (TM), vibrates when sound enters the ear canal. The vibration is transmitted to a series of bones in the middle ear. These bones transmit vibration to another membrane (the oval window) that separates the air‐filled middle ear from the fluid‐filled inner ear, where sound is sensed in the cochlea. The nasopharynx is the area behind the nose and above the palate. The Eustachian tubes open into this area. Because of the location of the Eustachian tube openings, the same things that cause nasal congestion (e.g. allergies, upper respiratory infection) can cause swelling around the opening of the Eustachian tubes, making it more difficult to equalize pressure in the middle ear. -

Laryngospasm Caused by Removal of Nasogastric Tube After Tracheal Extubation: Case Report
Yanaka A, et al. J Anesth Clin Care 2021, 8: 061 DOI: 10.24966/ACC-8879/100061 HSOA Journal of Anesthesia & Clinical Care Case Report pCO2: Partial pressure of carbon dioxide pO : Partial pressure of oxygen Laryngospasm Caused by 2 mmHg: Millimeter of mercury Removal of Nasogastric Tube mg/dl: Milligram per deciliter mmol/L: Millimole per litter after Tracheal Extubation: Case Introduction Report Background Laryngospasm (spasmodic closure of the larynx) is an airway Ayumi Yanaka1 and Takuo Hoshi2* complication that may occur when a patient emerges from general 1Department of Anesthesiology and Critical Care Medicine, Ibaraki Prefectur- anesthesia. It is a protective reflex, but may sometimes result in al Central Hospital, Japan pulmonary aspiration, pulmonary edema, arrhythmia and cardiac 2Department of Anesthesiology and Critical Care Medicine, Clinical and Edu- arrest [1]. It does not often cause severe hypoxemia in the patient, and cational Training Center, Tsukuba University Hospital, Japan our review of the literature revealed no previous reports of such cases that cause of the laryngospasm was the removal of nasogastric tube. Here, we describe this significant adverse event in a case and suggest Abstract ways to lessen the possibility of its occurrence. We obtained written informed consent for publication of this case report from the patient. Background: We report a case of laryngospasm during nasogastric tube removal. Laryngospasm is a severe airway complication after Case report surgery and there have been no reports associated with the removal of nasogastric tubes. A 54-year-old woman height, 157 cm; weight, 61 kg underwent abdominal surgery (partial hepatectomy with right partial Case Report: After abdominal surgery, the patient was extubated the tracheal tube, and was removed the nasogastric tube. -

Infectious Waste Contingency Plan
Infectious Waste Contingency Plan Office of Environmental Health and Safety January 2012 Table of Contents I. Introduction……………………………………………………………………………..3 II. Facility Identification…………………………………………………………………..3 III. Emergency Contacts………………………………………………………………...3-4 IV. Scope and Responsibilities……………………………………………………………5 V. Infectious Waste Defined………………………………………….…………………...5 VI. Procedures for Infectious Waste Generators…………………………….………….5-6 VII. Infectious Waste Storage – EHS…………………………………………………......7 VIII. Infectious Waste Disposal – EHS…………………………………………………7-8 IX. Autoclaving – BGES…………………………………………………………………..8 X. Spill Containment and Cleanup Procedures…………………………………………8-10 XI. Training……………………………………………………………………………......10 XII. Records………………………………………………………………………………..11 XIII. Contingency for Disposal…………………………………………………………….11 Appendix A – Definitions……………………………………………………………...12-13 Appendix B – “Sharps” Management……………………………………………………...14 Appendix C – Infectious Waste Inventory Form……………………………………….15-16 Appendix D – Infectious Waste Storage Area Inspection Form………………………..17-18 Appendix E – Spill Log Form…………………………………………………………..19-20 2 I. Introduction In accordance with amendments set forth by the Ohio Environmental Protection Agency (OEPA) to the Ohio Administrative Code (OAC) Chapter 3745, Cleveland State University has declared itself a large quantity generator of infectious waste (generates greater than fifty or more pounds of infectious waste per month) and has developed this Infectious Waste Contingency Plan in order to comply with the -

Critical Care in the Monoplace Hyperbaric Chamber
Critical Care in the Monoplace Hyperbaric Critical Care - Monoplace Chamber • 30 minutes, so only key points • Highly suggest critical care medicine is involved • Pitfalls Lindell K. Weaver, MD Intermountain Medical Center Murray, Utah, and • Ventilator and IV issues LDS Hospital Salt Lake City, Utah Key points Critical Care in the Monoplace Chamber • Weaver LK. Operational Use and Patient Care in the Monoplace Chamber. In: • Staff must be certified and experienced Resp Care Clinics of N Am-Hyperbaric Medicine, Part I. Moon R, McIntyre N, eds. Philadelphia, W.B. Saunders Company, March, 1999: 51-92 in CCM • Weaver LK. The treatment of critically ill patients with hyperbaric oxygen therapy. In: Brent J, Wallace KL, Burkhart KK, Phillips SD, and Donovan JW, • Proximity to CCM services (ed). Critical care toxicology: diagnosis and management of the critically poisoned patient. Philadelphia: Elsevier Mosby; 2005:181-187. • Must have study patient in chamber • Weaver, LK. Critical care of patients needing hyperbaric oxygen. In: Thom SR and Neuman T, (ed). The physiology and medicine of hyperbaric oxygen therapy. quickly Philadelphia: Saunders/Elsevier, 2008:117-129. • Weaver LK. Management of critically ill patients in the monoplace hyperbaric chamber. In: Whelan HT, Kindwall E., Hyperbaric Medicine Practice, 4th ed.. • CCM equipment North Palm Beach, Florida: Best, Inc. 2017; 65-95. • Without certain modifications, treating • Gossett WA, Rockswold GL, Rockswold SB, Adkinson CD, Bergman TA, Quickel RR. The safe treatment, monitoring and management -

Supplementary Material
Supplementary material Table S1. Search strategy performed on the following databases: PubMed, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL). 1. Randomi*ed study OR random allocation OR Randomi*ed controlled trial OR Random* Control* trial OR RCT Epidemiological study 2. sodium glucose cotransporter 2 OR sodium glucose cotransporter 2 inhibitor* OR sglt2 inhibitor* OR empagliflozin OR dapagliflozin OR canagliflozin OR ipragliflozin OR tofogliflozin OR ertugliflozin OR sotagliflozin OR sergliflozin OR remogliflozin 3. 1 AND 2 1 Table S2. Safety outcomes of empagliflozin and linagliptin combination therapy compared with empagliflozin or linagliptin monotherapy in treatment naïve type 2 diabetes patients Safety outcome Comparator 1 Comparator 2 I2 RR [95% CI] Number of events Number of events / / total subjects total subjects i. Empagliflozin + linagliptin vs empagliflozin monotherapy Empagliflozin + Empagliflozin linagliptin monotherapy ≥ 1 AE(s) 202/272 203/270 77% 0.99 [0.81, 1.21] ≥ 1 drug-related 37/272 38/270 0% 0.97 [0.64, 1.47] AE(s) ≥ 1 serious AE(s) 13/272 19/270 0% 0.68 [0.34, 1.35] Hypoglycaemia* 0/272 5/270 0% 0.18 [0.02, 1.56] UTI 32/272 25/270 29% 1.28 [0.70, 2.35] Events suggestive 12/272 13/270 9% 0.92 [0.40, 2.09] of genital infection i. Empagliflozin + linagliptin vs linagliptin monotherapy Empagliflozin + Linagliptin linagliptin monotherapy ≥ 1 AE(s) 202/272 97/135 0% 1.03 [0.91, 1.17] ≥ 1 drug-related 37/272 17/135 0% 1.08 [0.63, 1.84] AE(s) ≥ 1 serious AE(s) 13/272 2/135 0% 3.22 [0.74, 14.07] Hypoglycaemia* 0/272 1/135 NA 0.17 [0.01, 4.07] UTI 32/272 12/135 0% 1.32 [0.70, 2.49] Events suggestive 12/272 4/135 0% 1.45 [0.47, 4.47] of genital infection RR, relative risk; AE, adverse event; UTI, urinary tract infection. -

Summary of Investigation Results Sodium-Glucose Co-Transporter 2 (SGLT2) Inhibitors
Pharmaceuticals and Medical Devices Agency This English version is intended to be a reference material for the convenience of users. In the event of inconsistency between the Japanese original and this English translation, the former shall prevail. Summary of investigation results Sodium-glucose co-transporter 2 (SGLT2) inhibitors September 15, 2015 Non-proprietary name a. Canagliflozin hydrate b. Dapagliflozin propylene glycolate hydrate c. Empagliflozin d. Ipragliflozin L-proline e. Luseogliflozin hydrate f. Tofogliflozin hydrate Brand name (Marketing authorization holder) a. Canaglu Tablets 100 mg (Mitsubishi Tanabe Pharma Corporation) b. Forxiga Tablets 5 mg and 10 mg (AstraZeneca K.K.) c. Jardiance Tablets 10 mg and 25 mg (Nippon Boehringer Ingelheim Co., Ltd.) d. Suglat Tablets 25 mg and 50 mg (Astellas Pharma Inc.) e. Lusefi Tablets 2.5 mg and 5 mg (Taisho Pharmaceutical Co., Ltd.) f. Apleway Tablets 20 mg (Sanofi K.K.) and Deberza Tablets 20 mg (Kowa Company, Ltd.) Indications Type 2 diabetes mellitus Summary of revision 1. Precautions regarding ketoacidosis should be added in the Important Precautions section for the above products from a to f. 2. “Ketoacidosis” should be newly added in the Clinically significant adverse reaction section for the above products from a to f. 3. “Sepsis” should be added to the “Pyelonephritis” subsection in the Important Precautions section for the above products from a to f. Pharmaceuticals and Medical Devices Agency Office of Safety I 3-3-2 Kasumigaseki, Chiyoda-ku, Tokyo 100-0013 Japan E-mail: [email protected] Pharmaceuticals and Medical Devices Agency This English version is intended to be a reference material for the convenience of users. -

Anti-Hypotensive Effects of M6434, an Orally Active a 1-Adrenoceptor Agonist, in Rats
Anti-Hypotensive Effects of M6434, an Orally Active a 1-Adrenoceptor Agonist, in Rats Tatsuroh Dabasaki, Masato Shimojo, Hiroshi Ishikawa and Akio Uemura Fuji Central Research Laboratory, Mochida Pharmaceutical Co., Ltd., 722 Jimba-aza-Uenohara, Gotemba, Shizuoka 412, Japan Received December 19, 1991 Accepted February 17, 1992 ABSTRACT-The anti-hypotensive effects of M6434 were evaluated and compared with those of other orally active sympathomimetics in rats. Oral administration of M6434 (0.5-2.0 mg/kg) and midodrine (1.0 5.0 mg/kg) also produced a dose-related increase in mean arterial pressure in normotensive rats. The pressor effect of M6434 was about 4 times more potent than that of midodrine. Both M6434 and midodrine caused a dose-dependent decrease in heart rate. The pressor effect of M6434 (1.0 mg/kg) did not diminish after its repeated administration for 7 days. The pretreatment with M6434 (0.5 1.0 mg/kg) and midodrine (2.0 5.0 mg/kg) improved the orthostatic index in the experimental model of postural hypotension in rats. The effect of M6434 on postural hypotension was about 5 times more po tent than that of midodrine. Intravenously injected M6434 (3-300pg/kg) produced a dose-dependent increase in the blood pressure of pithed rats. These results suggest that M6434 possesses a potent anti hypotensive activity which is superior to that of midodrine, and M6434 may be useful in the treatment of essential and postural hypotension. Keywords: M6434, a 1-Agonist, Midodrine, Postural hypotension, Orthostatic index M6434, 2-[(5-chloro-2-methoxyphenyl)azo]-1H-imida in clinical therapy. -

Natural Products As Lead Compounds for Sodium Glucose Cotransporter (SGLT) Inhibitors
Reviews Natural Products as Lead Compounds for Sodium Glucose Cotransporter (SGLT) Inhibitors Author ABSTRACT Wolfgang Blaschek Glucose homeostasis is maintained by antagonistic hormones such as insulin and glucagon as well as by regulation of glu- Affiliation cose absorption, gluconeogenesis, biosynthesis and mobiliza- Formerly: Institute of Pharmacy, Department of Pharmaceu- tion of glycogen, glucose consumption in all tissues and glo- tical Biology, Christian-Albrechts-University of Kiel, Kiel, merular filtration, and reabsorption of glucose in the kidneys. Germany Glucose enters or leaves cells mainly with the help of two membrane integrated transporters belonging either to the Key words family of facilitative glucose transporters (GLUTs) or to the Malus domestica, Rosaceae, Phlorizin, flavonoids, family of sodium glucose cotransporters (SGLTs). The intesti- ‑ SGLT inhibitors, gliflozins, diabetes nal glucose absorption by endothelial cells is managed by SGLT1, the transfer from them to the blood by GLUT2. In the received February 9, 2017 kidney SGLT2 and SGLT1 are responsible for reabsorption of revised March 3, 2017 filtered glucose from the primary urine, and GLUT2 and accepted March 6, 2017 GLUT1 enable the transport of glucose from epithelial cells Bibliography back into the blood stream. DOI http://dx.doi.org/10.1055/s-0043-106050 The flavonoid phlorizin was isolated from the bark of apple Published online April 10, 2017 | Planta Med 2017; 83: 985– trees and shown to cause glucosuria. Phlorizin is an inhibitor 993 © Georg Thieme Verlag KG Stuttgart · New York | of SGLT1 and SGLT2. With phlorizin as lead compound, specif- ISSN 0032‑0943 ic inhibitors of SGLT2 were developed in the last decade and some of them have been approved for treatment mainly of Correspondence type 2 diabetes.