22 February 2019: No 2 in Memory: Dr Mags Portman
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sunday, November 7, 2021
SUNDAY, NOVEMBER 7, 2021 PRE-CONFERENCE SESSIONS TBA 9:00 AM – 10:30 AM TBA TBA 10:30 AM - Noon TBA Noon - 1:00 PM Lunch OPENING REMARKS 1:00 PM - 1:15 PM Welcome to Adherence 2021 1:15 PM - 1:20 PM Break KEYNOTE ADDRESS Making Up for Lost Time: Critical Steps to Regain Momentum in HIV Prevention and Treatment 1:20 PM - 1:50 PM Meg Doherty, World Health Organization, Geneva, Switzerland* 1:50 PM - 1:55 PM Break HIV TREATMENT ADHERENCE Moderator : Jessica Haberer, Massachussetts General Hospital* and Jean Bisimwa Nachega, University of Pittsbur State-of-the-Art: A Review of Long-Acting Antivirals for HIV Treatment from an Adherence Perspective Susan Swindells, Nebraska AIDS Education Training Center, Omaha, NE, USA* Paradigm Shift: Asssessing Acceptability and Creating Demand for Long-Acting and Extended Release Formulations for HIV Treatment 1:55 PM - 3:10 PM Delivette Castor, Columbia University, New York, NY, USA* Antiretroviral Drug Resistance: Managing the Clinical Challenges of Long-Lasting Drug Concentrations Charlie Flexner, Johns Hopkins University, Baltimore, MD, USA* Discussion (15 minutes) 3:10 PM - 3:40 PM Break IMPLEMENTATION SCIENCE Moderator : Elvin Geng, Washington University of St. Louis* and Juliet Iwelunmor, Saint Louis University* Reaching Youth through Crowd Sourcing Juliet Iwelunmor, Saint Louis University, St. Louis, MO, USA COVID-19 and HIV Services: Disruptive Thinking for Disruptive Times 3:40 PM - 4:55 PM Matt Golden, University of Washington, Seattle, WA, USA Renewing Commitment to Equity in the HIV Response Lisa Bowleg, George Washington University, Washington, DC, USA Discussion (15 minutes) 4:55 PM - 5:00 PM Break THREE TOP-RATED ABSTRACTS 5:00 PM - 6:00 PM 6:00 PM Adjourn MONDAY, NOVEMBER 8, 2021 GARY S. -

FTC London Conference 2019 Report
SEPTEMBER 9-11, 2019 CONFERENCE REPORT SPONSORED BY: IN PARTNERSHIP WITH: GLOBAL NETWORK OF PEOPLE LIVING WITH HIV LONDON FAST-TRACK CITIES 2019 CONFERENCE REPORT Contents INTRODUCTION . 2 Conference Framework . 4 Conference Report Structure . 4 LEADERSHIP IN ACTION . 5 A Tale of Three Fast-Track Cities . 5 London . 5 Nairobi City County . 7 New York City . 9 Projecting and Monitoring 90-90-90 . 13 Modeling Impact and Effectiveness . 15 Unite as Leaders . 16 PLACING PEOPLE AT THE CENTER . 17 Addressing Stigma . 18 Promoting U=U . 18 Addressing Stigma in Key Populations . 19 Risk, Vulnerability, and Transmission . 21 Violence against Adolescent Girls and Young Women . 21 Mental Health and Substance Use . 23 Aging with HIV . 24 Migration . 25 Injection Drug Use . 25 Prioritizing Quality of Life . 26 Community-Led Responses . 28 INNOVATIONS IN HIV TESTING, ART, AND PREP . 31 Innovations in HIV Testing . 31 HIV Self-Testing . 31 HIVcheck .jp Project . 31 Click-and-Collect . 32 Provider-Initiated HIV Testing . 33 Innovations in ART and ART Delivery . 33 RAPID . 34 Crescent Care Start Initiative . 35 1917 Clinic Fast-Track . 35 Rapid Start . 36 H-Team . 37 Innovations in HIV PrEP . 38 Technology and ART . 38 ADDRESSING COMORBIDITIES . 39 Tuberculosis . 39 Viral Hepatitis . 40 Other STIs beyond HIV . 41 CONCLUSION . 42 Acknowledgements . 45 i FAST-TRACK CITIES 2019 | SEPTEMBER 9-11, 2019 | BARBICAN CENTRE, LONDON LONDON FAST-TRACK CITIES 2019 CONFERENCE REPORT DEVELOPMENT OF THE FAST-TRACK CITIES 2019 CONFERENCE REPORT WAS SPONSORED BY: INTRODUCTION INTRODUCTION Since the Joint United Nations Programme on HIV/AIDS (UNAIDS) convened high-level stakeholders in December 2013 to plot a roadmap towards expanding access to HIV testing and treatment with the aim of blunting the course of the HIV epidemic, there has been a growing sense of commitment and optimism by governments, non-governmental organizations, funders, and community leaders that ending AIDS as a public health threat by 2030 may be feasible . -

Aidsimpact 2009 Programme
1 Tuesday # Title Type Times Room Chairs SIDACTION, Tsodilo Vincent Douris, 1 An international measure of Quality of Life specific to PW HIV Satellite 10.00-13:00 B4 Veronica Noseda Tsodilo 2 Ethics of Clinical Research Satellite 10:00-13:00 Sidaction B1+2 Tsodilo 3 HIV considerations in Botswana Satellite 13:00-14:00 Sheila Tlou B1+2 Rosemary Building capacity for HIV/AIDS prevention trials in Africa: Strategies for Serondela 4 Satellite 10:00-12:00 Musonda, meeting a multi-dimensional challenge 3+4 Robert Geneau HSRC, Serondela 46 HIV in South Africa: A Turning Tide Among Teenagers? Satellite 12:00-14:00 Olive Shisana, 3+4 Linda Richter Tsodilo Simon Rosser, 47 Are gay communities dying Satellite 13:00-14:00 B4 William West Sheila Tlou, 5 Opening Ceremony Plenary 14:00-15:00Tsodilo C Batho C. Molomo 5.1OPENING CEREMONY - 14:00-14:05--National Anthem led by NACA Choi 14:05-14:10--Welcome remarks by Prof. Sheila Tlou, Co-Chair, Local Organising Committee 14:10-14:15--Remarks by Prof. Lorraine Sherr, AIDS Impact 14:15-14:20--Remarks Ms. Regina Lesole , Activist, Ms. Stigma-Free 2006 14:20-14:30--Song by NACA choir 5.2Mark Stirling Keynote address - Global HIV Challenges 2 Lorraine Sherr, 6 HIV state of the Art Plenary 15:30-18:00Tsodilo C Pepe Catalan 6.1Olive Shisana HIV in the disabled population: are we doing our part? 6.2Chloe Orkin Anti-retroviral therapy in 2009: what have we learned? 6.3Gita Ramjee HIV Prevention Overview 6.4Bruno Spire Quality of Life and HIV- ANRS Plenary 6.5John De Wit Gay Men 6.6Elly Katabira International AIDS -
Boston March 4-7, 2018 Program and Conference Information
Program and Conference Information Conference on Retroviruses and Opportunistic Infections Boston March 4-7, 2018 General Information CONTENTS Information General CROI FOUNDATION ...........................................................2 IAS–USA.......................................................................2 CROI 2018 PROGRAM COMMITTEE.........................................3 Scientific Program Committee .........................................3 Community Liaison Subcommittee .....................................5 EXTERNAL REVIEWERS . 6 SCHOLARSHIP AWARDEES ..................................................8 New Investigator Awardees.................................................8 International Investigator Awardees .......................................12 Community Educator Awardees............................................12 CONTINUING MEDICAL EDUCATION ......................................13 GENERAL INFORMATION . .15 Overview .................................................................15 Conference Support .......................................................15 Americans With Disabilities Act ............................................15 Emergency Services . .15 Embargo Policies and Social Media ....................................16 Welcome Reception .......................................................16 Meals.....................................................................16 Overflow Accommodations for Oral Sessions................................17 Mobile App ...............................................................17 -
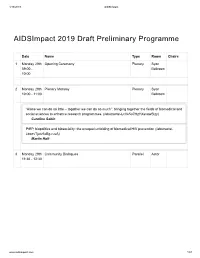
Aidsimpact 2019 Draft Preliminary Programme
4/16/2019 AIDSImpact AIDSImpact 2019 Draft Preliminary Programme Date Name Type Room Chairs 1 Monday 29th Opening Ceremony Plenary Syon 09:00 - Ballroom 10:00 2 Monday 29th Plenary Monday Plenary Syon 10:00 - 11:00 Ballroom “Alone we can do so little – together we can do so much”: bringing together the fields of biomedical and social sciences to enhance research programmes. (/abstracts/-LcVe5o7HzYXsvawSlzy) Caroline Sabin PrEP, biopolitics and biosociality: the unequal unfolding of biomedical HIV prevention (/abstracts/- LbaevTjutv6xBg-ruvA) Martin Holt 3 Monday 29th Community Dialogues Parallel Astor 11:30 - 12:30 www.aidsimpact.com 1/57 4/16/2019 AIDSImpact Date Name Type Room Chairs South African adolescent girls’ and young women’s narratives of communication with and support from parents and teachers: implications for sexual and reproductive health decisions (/abstracts/- LZtCv6dXuEhYZ5V5V8n) Zoe Duby, Kim Jonas, Kealeboga Maruping, Ashleigh LoVette, Caroline Kuo, Catherine Mathews The embodied relationality of blood-borne viruses: How families matter in the context of a stigmatised viral infection (/abstracts/-LZqqpIxbkjOKRBI0o8y) Asha Persson, Christy Newman, Myra Hamilton, Joanne Bryant, kylie valentine, Kerryn Drysdale, Rebecca Gray A support for autonomy for people living with HIV in West Guina: health and associative professionals’ discourses and visions on a complex phenomenon. (/abstracts/-LZfTrHBB_l_aYW52RT1) Anne-Sophie Petit, Nikos Kalampalikis, Marie Préau Adherence and retention in a community-based trial testing PrEP -
Croi 2021 Program Committee
General Information CONTENTS WELCOME . 2 General Information General Information OVERVIEW . 2 CONTINUING MEDICAL EDUCATION . 3 CONFERENCE SUPPORT . 4 VIRTUAL PLATFORM . 5 ON-DEMAND CONTENT AND WEBCASTS . 5 CONFERENCE SCHEDULE AT A GLANCE . 6 PRECONFERENCE SESSIONS . 9 LIVE PLENARY, ORAL, AND INTERACTIVE SESSIONS, AND ON-DEMAND SYMPOSIA BY DAY . 11 SCIENCE SPOTLIGHTS™ . 47 SCIENCE SPOTLIGHT™ SESSIONS BY CATEGORY . 109 CROI FOUNDATION . 112 IAS–USA . 112 CROI 2021 PROGRAM COMMITTEE . 113 Scientific Program Committee . 113 Community Liaison Subcommittee . 113 Former Members . 113 EXTERNAL REVIEWERS . .114 SCHOLARSHIP AWARDEES . 114 AFFILIATED OR PROXIMATE ACTIVITIES . 114 EMBARGO POLICIES AND SOCIAL MEDIA . 115 CONFERENCE ETIQUETTE . 115 ABSTRACT PROCESS Scientific Categories . 116 Abstract Content . 117 Presenter Responsibilities . 117 Abstract Review Process . 117 Statistics for Abstracts . 117 Abstracts Related to SARS-CoV-2 and Special Study Populations . 117. INDEX OF SPECIAL STUDY POPULATIONS . 118 INDEX OF PRESENTING AUTHORS . .122 . Version 9 .0 | Last Update on March 8, 2021 Printed in the United States of America . © Copyright 2021 CROI Foundation/IAS–USA . All rights reserved . ISBN #978-1-7320053-4-1 vCROI 2021 1 General Information WELCOME TO vCROI 2021 Welcome to vCROI 2021! The COVID-19 pandemic has changed the world for all of us in so many ways . Over the past year, we have had to put some of our HIV research on hold, learned to do our research in different ways using different tools, to communicate with each other in virtual formats, and to apply the many lessons in HIV research, care, and community advocacy to addressing the COVID-19 pandemic . Scientists and community stakeholders who have long been engaged in the endeavor to end the epidemic of HIV have pivoted to support and inform the unprecedented progress made in battle against SARS-CoV-2 . -

Report from the 10Th International AIDS Society Conference on HIV
HIV Nursing 2019; 19(3): 74–77 Conference Report Report from the 10th International AIDS Society Conference on HIV Science 21–24 July 2019 Mexico City, Mexico Shaun Watson Clinical Nurse Specialist (HIV Community) , Chelsea and Westminster NHS Trust, London Introduction surveillance sites in Botswana and an increased cover- age from 45% to 75% of all births, concluding that This year ’ s International AIDS Society (IAS) conference there is now a 0.3% prevalence of NTDs amongst ‘IAS19’ was held in Mexico City, a place that despite women taking dolutegravir at conception [2–4] . It was the danger warnings, was colourful, vibrant, friendly interesting to note that NTDs were noted in nine out and culturally fascinating. It ’ s great to be here but this of 23 315 women without HIV, a 0.04% prevalence. is no jolly holiday as sessions start at 07:00 and end at What does this mean? Zash et al . concluded the session 20:30, for most of us it ’ s a 45-minute taxi ride in as the with some clinical and policy recommendations based conference centre is at the edge of a very car-heavy city. on their fi ndings stating that there is a small potential IAS19 delivered a lot of new data with the long-awaited risk of NTDs compared with the larger potential benefi ts news on the potential link between dolutegravir and of dolutegravir use, there is a lack of data for most neural tube birth defects, new antiretroviral therapy other modern ARVs (except efavirenz, which interest- (ART), especially the simplifi cation of treatment regi- ingly was the initial focus of the Tsepamo). -

Long-Active Cabotegravir + Rilpivirine for HIV Maintenance: FLAIR Week 48 Results
Long-Active Cabotegravir + Rilpivirine for HIV Maintenance: FLAIR WeeK 48 Results Chloe Orkin,1 KeiKawus Arasteh,2 Miguel Górgolas Hernández-Mora,3 Vadim PoKrovsKy,4 Edgar T. Overton,5 Pierre-Marie Girard,6 Shinichi OKa,7 Ronald D’Amico,8 David Dorey,9 Sandy Griffith,8 David A. Margolis,8 Peter Williams,10 Wim Parys,10 William R. Spreen8 1Queen Mary University, London, UK; 2EPIMED GmbH, Berlin, Germany; 3Fundación Jiménez Díaz, Madrid, Spain; 4Central Institute of Epidemiology, Moscow, Russia; 5University of Alabama at Birmingham, Birmingham, AL, USA; 6Hôpital Saint Antoine, Paris, France; 7National Center for Global Health and Medicine, Tokyo, Japan; 8ViiV Healthcare, Research Triangle Park, NC, USA; 9GlaxoSmithKline, Mississauga, Ontario, Canada; 10Janssen Research and Development, Beerse, Belgium 25th Annual Conference of the British HIV Association; April 2-5, 2019; Bournemouth, UK Disclosures • I have received grants to my institution from Gilead, Janssen, ViiV Healthcare, and Merck Sharpe & Dohme • I have received travel scholarships, honoraria for advisory boards, and speaker fees from Gilead, Janssen, ViiV Healthcare, and Merck Sharpe & Dohme Ork in et al. BHIVA 2019; Bournemouth, UK. Slides O10. 25th Annual Conference of the British HIV Association; April 2-5, 2019; Bournemouth, UK FLAIR BacKground • Approved therapies for HIV now include once-daily oral regimens containing 2 or 3 antiretrovirals • Despite the success of daily oral therapy, considerable interest exists in LA treatment options • Cabotegravir (CAB) is an HIV-1 integrase strand transfer inhibitor – Oral 30 mg tablet: t½ ≈ 40 hours – Long-acting IM injection, 200 mg/mL: t½ ≈ 40 days • Rilpivirine (RPV) is an HIV-1 non-nucleoside reverse transcriptase inhibitor – Oral 25 mg tablet: t½ ≈ 50 hours – Long-acting IM injection, 300 mg/mL: t½ ≈ 90 days • LATTE-2: CAB LA + RPV LA given every 4 or 8 weeks maintained HIV-1 RNA <50 c/mL for >3 years1 • Two pivotal phase 3 studies (ATLAS2 and fLAIR) have reached their primary endpoints at 48 weeks IM, intramuscular; LA, long-acting. -

Sunday, November 7, 2021
SUNDAY, NOVEMBER 7, 2021 PRE-CONFERENCE SESSIONS TBA 9:00 AM – 10:30 AM TBA TBA 10:30 AM - Noon TBA Noon - 1:00 PM Lunch OPENING REMARKS 1:00 PM - 1:15 PM Welcome to Adherence 2021 1:15 PM - 1:20 PM Break KEYNOTE ADDRESS Making Up for Lost Time: Critical Steps to Regain Momentum in HIV Prevention and Treatment 1:20 PM - 1:50 PM Meg Doherty, World Health Organization, Geneva, Switzerland* 1:50 PM - 1:55 PM Break HIV TREATMENT ADHERENCE State-of-the-Art: A Review of Long-Acting Antivirals for HIV Treatment from an Adherence Perspective Susan Swindells, Nebraska AIDS Education Training Center, Omaha, NE, USA* Paradigm Shift: Asssessing Acceptability and Creating Demand for Long-Acting and Extended Release Formulations for HIV Treatment 1:55 PM - 3:10 PM Delivette Castor, Columbia University, New York, NY, USA* Antiretroviral Drug Resistance: Managing the Clinical Challenges of Long-Lasting Drug Concentrations Charlie Flexner, Johns Hopkins University, Baltimore, MD, USA* Discussion (15 minutes) 3:10 PM - 3:40 PM Break IMPLEMENTATION SCIENCE Reaching Youth through Crowd Sourcing Juliet Iwelunmor, Saint Louis University, St. Louis, MO, USA COVID-19 and HIV Services: Disruptive Thinking for Disruptive Times 3:40 PM - 4:55 PM Matt Golden, University of Washington, Seattle, WA, USA Renewing Commitment to Equity in the HIV Response Lisa Bowleg, George Washington University, Washington, DC, USA Discussion (15 minutes) 4:55 PM - 5:00 PM Break THREE TOP-RATED ABSTRACTS 5:00 PM - 6:00 PM 6:00 PM Adjourn MONDAY, NOVEMBER 8, 2021 GARY S. REITER AND -

HIV & Hepatitis Nordic Conference 2019
HIV & Hepatitis Nordic Conference 2019 HIV & Hepatitis Nordic Conference 2019 The HIV & Hepatitis Nordic Conference have twice as high risk for cardiovascular ties. Effective treatment of modifiable was held in Stockholm in September 25 disease compared with the background risk factors – such as smoking, high cho- - 27. Almost 300 participants had come population. A study we did on peripheral lesterol and high blood pressure – can to the Swedish capital to attend. artery disease showed that PLWH have a significantly reduce an individual's risk 75 % increased risk for this disease, Prof for cardiovascular disease. Dam Poulsen continued. – The median age of PLWH has increa- – 300 is an ideal number – because it Pulmonary disease in PLWH have a sed. It is estimated that in 2030, 40 % of allows for discussions, and enables new high prevalence of airflow limitation PLWH will be 60 years old or more. This networks to be formed, Prof Magnus of 10 - 15 %, and this is associated with underlines the importance of prevention. Gisslén stated when he greeted them all death. A comparison of 598 PLWH and We should always try to get our patients welcome to the Opening session. 2,598 controls on renal impairment show to quit smoking, she said. It was for the sixth time this annual a prevalence of 3.7 % for PLWH versus Efforts to avoid late presentation may Meeting took place, focusing on the 1.7 %. also decrease co-morbidities. Collabo- Nordic region. The lecturers consisted – The overall prevalence of renal im- ration with GPs is needed in managing of – as always – an exciting mix between pairment in PLWH is 6.4 %, with some the ageing and co-morbid population of international and Scandinavian key-note geographical variation. -

Hepatitis C Good Practice Roadshow
Hepatitis C Good Practice Roadshow Tuesday 24 November 2015 Brighton Welcome and introduction and setting the scene Charles Gore, Chief Executive, The Hepatitis C Trust Tuesday 24 November 2015 Brighton Local epidemiology Paul Crook, Consultant Epidemiologist, Public Health England Tuesday 24 November 2015 Brighton Hepatitis C epidemiology in the South East Dr Paul Crook Consultant Epidemiologist Field Epidemiology Services South East & London National Infection Service, Public Health England Rate of new hepatitis C reports Rate of laboratory confirmed diagnoses of hepatitis C per 100,000 residents, by Region, 2014 Source: Laboratory reports PHE 50.0 2014 rate 2014 number 4,500 45.0 4,000 40.0 3,500 35.0 3,000 30.0 2,500 25.0 2,000 Number Rate/100,000 20.0 1,500 15.0 10.0 1,000 5.0 500 45.2 28.4 20.9 17.7 15.3 13.3 12.0 11.6 11.4 0.0 0 London Yorkshire North West South West South East East East of North East West and Midlands England Midlands Humber PHE Centre 5 Hepatitis C epidemiology in the South East Risk factors for hepatitis C People who have ever injected drugs People who received a blood transfusion before 1991 or blood products before 1986 People born or brought up in a country with an intermediate or high prevalence (2% or greater) of chronic hepatitis C. Babies born to mothers infected with hepatitis C Prisoners, including young offenders Looked-after children and young people, including those living in care homes People living in hostels for the homeless or sleeping on the streets HIV-positive men who have sex with men Close contacts of someone known to be chronically infected with hepatitis C 6 Hepatitis C epidemiology in the South East Men who have sex with men (MSM) with hepatitis C 75% - history of non-injecting recreational drug use 33% - injecting drug use 86% - sex under influence of drugs High proportions – unprotected sex Source: Public Health England. -

Hiv Medicine
HIV MEDICINE Published on behalf of the British HIV Association and the European AIDS Clinical Society Editors Brian Gazzard, UK claims for missing or damaged copies within six months of publication, within Jens Lundgren, Denmark our reasonable discretion and subject to availability. Back issues: Single issues from current and recent volumes are available at the Associate Editors current single issue price from [email protected]. Earlier issues may be obtained from Periodicals Service Company, 351 Fairview Avenue – Ste 300, José Gatell, Spain Hudson, NY 12534, USA. Margaret Johnson, UK Tel: +1 518 822-9300, Fax: +1 518 822-9305, Jürgen Rockstroh, Germany Email: [email protected] Georg Behrens, Germany HINARI: Access to this journal is available free online within institutions in the Caroline Sabin, UK developing world through the HINARI initiative with the WHO. For information, visit www.who.int/hinari/en/ Roger Paredes, Spain Wiley is a founding member of the UN-backed HINARI, AGORA, and OARE initiatives. They are now collectively known as Research4Life, making online Editorial Board scientific content available free or at nominal cost to researchers in developing Jane Anderson, UK Jeff Lazarus, Denmark countries. Please visit Wiley’s Content Access – Corporate Citizenship site: http:// Francisco Antunes, Portugal Adriano Lazzarin, Italy www.wiley.com/WileyCDA/Section/id-390082.html Jose Arribas, Spain Hermione Lyall, UK Jason Baker, USA Paddy Mallon, Dublin Georg Behrens, Germany Esteban Martinez, Spain Publisher and Business Correspondence Sanjay Bhagani, UK Catia Marzolini, Switzerland HIV Medicine is published by John Wiley & Sons Ltd: 9600 Jordi Blanch, Spain Gail Matthews, Australia Garsington Road, Oxford OX4 2DQ, UK.