Scheduling Evaluation Report Application to Amend the Poisons
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Robert Cathey Research Source
THE ROBERT CATHEY RESEARCH SOURCE http://www.navi.net/~rsc A bibliography of essays and monographs by Dr. Krebs, John Beard and other's involved the metabolic resolution of cancer will be found at: http://www.navi.net/~rsc/krebsall.htm. rsc. (Updated 31 July 1997...see end of file for graphic links; for an essay on suggested mechanisms of action of nitrilosides; Also, certain terms are defined in the text for clarity and are included in brackets.rsc) THE NITRILOSIDES IN PLANTS AND ANIMALS Nutritional and Therapeutic Implications Ernst T. Krebs, Jr. John Beard Memorial Foundation (Privately published: 1964) Since the principal objective of this presentation is a study of the clinical use of the Laetriles (nitrilosides) because these substances yield nascent HCN [hydrocyanic acid] when they undergo enzymatic hydrolysis in vivo, it will be helpful if one begins with a general study of the nitrilosides in plants and animals. A nitriloside is a naturally occurring or synthetic compound which upon hydrolysis by a beta- glucosidase yields a molecule of a non-sugar, or aglycone, a molecule of free hydrogen cyanide, and one or more molecules of a sugar or its acid. There are approximately 14 naturally occurring nitrilosides distributed in over 1200 species of plants. Nitrilosides are found in all plant phyla from Thallophyta to Spermatophyta. The nitrilosides specifically considered in this paper are 1-mandelonitrile-beta-diglucoside (amygdalin) and its hydrolytic products; 1-para-hydroxymandelonitrile-beta-glucoside (dhurrin); methylethyl-ketone-cyanohydrin-beta-glucoside (lotaustralin); and acetone-cyanohydrin-beta- glucoside (linamarin). All of these compounds are hydrolysed to free HCN, one or more sugars and a non-sugar or aglycone. -

Content of the Cyanogenic Glucoside Amygdalin in Almond Seeds Related
Content of the cyanogenic glucoside amygdalin in almond seeds related to the bitterness genotype Contenido del glucósido cianogénico amigdalina en semillas de almendra con relación al genotipo con sabor amargo Guillermo Arrázola1, Raquel Sánchez P.2, Federico Dicenta2, and Nuria Grané3 ABSTRACT RESUMEN Almond kernels can be sweet, slightly bitter or bitter. Bitterness Las semillas de almendras pueden ser dulces, ligeramente ama- in almond (Prunus dulcis Mill.) and other Prunus species is rgas y amargas. El amargor en almendro (Prunus dulcis Mill.) related to the content of the cyanogenic diglucoside amygdalin. y en otras especies de Prunus se relaciona con el contenido de When an almond containing amygdalin is chopped, glucose, la amígdalina diglucósido cianogénico. Cuando una almendra benzaldehyde (bitter flavor) and hydrogen cyanide (which que contiene amigdalina se tritura, produce glucosa, benzal- is toxic) are released. This two-year-study with 29 different dehído (sabor amargo) y ácido cianihídrico (que es tóxico). El almond cultivars for bitterness was carried out in order to estudio es realizado durante dos años, con 29 variedades de al- relate the concentration of amygdalin in the kernel with the mendra diferentes para la amargura o amargor, se ha realizado phenotype (sweet, slightly bitter or bitter) and the genotype con el fin de relacionar la concentración de la amígdalina en el (homozygous: sweet or bitter or heterozygous: sweet or slightly núcleo con el fenotipo (dulce, ligeramente amargo y amargo) bitter) with an easy analytical test. Results showed that there y el genotipo (homocigota: dulce o amargo o heterocigótico: was a clear difference in the amount of amygdalin between bit- dulce o amarga un poco) por un ensayo de análisis fácil. -
Material Safety Data Sheet Mandelonitrile, Tech. MSDS
Material Safety Data Sheet Mandelonitrile, tech. MSDS# 70343 Section 1 - Chemical Product and Company Identification MSDS Name: Mandelonitrile, tech. Catalog AC152090000, AC152091000, AC152095000 Numbers: Acetonitrile, hydroxypehnyl-; Amygdalonitrile; Benzaldehyde cyanohydrin; Glycolonitirile, phenyl-; Synonyms: Mandelic acid nitrile; Nitril kyseliny mandlove (Czech) Acros Organics BVBA Company Identification: Janssen Pharmaceuticalaan 3a 2440 Geel, Belgium Acros Organics Company Identification: (USA) One Reagent Lane Fair Lawn, NJ 07410 For information in the US, call: 800-ACROS-01 For information in Europe, call: +32 14 57 52 11 Emergency Number, Europe: +32 14 57 52 99 Emergency Number US: 201-796-7100 CHEMTREC Phone Number, US: 800-424-9300 CHEMTREC Phone Number, Europe: 703-527-3887 Section 2 - Composition, Information on Ingredients ---------------------------------------- CAS#: 532-28-5 Chemical Name: Mandelonitrile, tech. %: ca. 100 EINECS#: 208-532-7 ---------------------------------------- Hazard Symbols: T Risk Phrases: 23/24/25 Section 3 - Hazards Identification EMERGENCY OVERVIEW Warning! Moisture sensitive. The toxicological properties of this material have not been fully investigated. Causes severe eye irritation. Harmful if swallowed, inhaled, or absorbed through the skin. Target Organs: No data found. Potential Health Effects Eye: Causes severe eye irritation. Skin: Causes skin irritation. Metabolism may release cyanide, which may result in headache, dizziness, weakness, collapse, unconsciousness Ingestion: and possible -

Research Journal of Pharmaceutical, Biological and Chemical Sciences
ISSN: 0975-8585 Research Journal of Pharmaceutical, Biological and Chemical Sciences Laetrile Or Amygdalin (Vitamin B-17) – Nutrient Or A Drug: A Review Of Running Controversies. MR Suchitra, and S Parthasarathy*. 1Department Of Biochemistry, SASTRA University, Tamil Nadu, India. 2Mahatma Gandhi Medical College And Research Institute, Sri Balaji Vidyapeeth University, Puducherry – South India ABSTRACT Amygdalin/Vitamin B17/Laetrile is a cyanogenic diglucoside, an active ingredient of several fruit pits and rawnuts was thought to possess anti-cancer properties. Amygdalin is contained in a few stone fruit kernels, such as apricot bitter almond, peach and plum and in the seeds of the apple. Even though there are a few animal and human studies which demonstrate the benefits of amygdalin in cancer, these are not well established in randomized clinical trials. When considering the other diseases like hypertension, pain, and bronchial asthma the role of Laetrile needs to be explored by using this drug as a supplement to regular therapeutic strategies. But as such the intake of apricot kernels and apple seeds should not be discouraged for fear of amygdalin toxicity in view of their other nutritional benefits. Keywords: laetrile, amygdalin, vitamin B17, *Corresponding author January – February 2019 RJPBCS 10(1) Page No. 437 ISSN: 0975-8585 INTRODUCTION AND CHEMISTRY Vitamin B17/Amygdalin/Laetrile is one of the most controversial vitamins in the last three decades. Chemically, it is a cyanogenic di-glucoside, but with a condensed formula of C20-H27-NO-11, and a MW (molecular weight) of 457. It has a chemical name of DMandelonetrile-betaglucoside-6 beta-D-glucoside. -

Studies on Betalain Phytochemistry by Means of Ion-Pair Countercurrent Chromatography
STUDIES ON BETALAIN PHYTOCHEMISTRY BY MEANS OF ION-PAIR COUNTERCURRENT CHROMATOGRAPHY Von der Fakultät für Lebenswissenschaften der Technischen Universität Carolo-Wilhelmina zu Braunschweig zur Erlangung des Grades einer Doktorin der Naturwissenschaften (Dr. rer. nat.) genehmigte D i s s e r t a t i o n von Thu Tran Thi Minh aus Vietnam 1. Referent: Prof. Dr. Peter Winterhalter 2. Referent: apl. Prof. Dr. Ulrich Engelhardt eingereicht am: 28.02.2018 mündliche Prüfung (Disputation) am: 28.05.2018 Druckjahr 2018 Vorveröffentlichungen der Dissertation Teilergebnisse aus dieser Arbeit wurden mit Genehmigung der Fakultät für Lebenswissenschaften, vertreten durch den Mentor der Arbeit, in folgenden Beiträgen vorab veröffentlicht: Tagungsbeiträge T. Tran, G. Jerz, T.E. Moussa-Ayoub, S.K.EI-Samahy, S. Rohn und P. Winterhalter: Metabolite screening and fractionation of betalains and flavonoids from Opuntia stricta var. dillenii by means of High Performance Countercurrent chromatography (HPCCC) and sequential off-line injection to ESI-MS/MS. (Poster) 44. Deutscher Lebensmittelchemikertag, Karlsruhe (2015). Thu Minh Thi Tran, Tamer E. Moussa-Ayoub, Salah K. El-Samahy, Sascha Rohn, Peter Winterhalter und Gerold Jerz: Metabolite profile of betalains and flavonoids from Opuntia stricta var. dilleni by HPCCC and offline ESI-MS/MS. (Poster) 9. Countercurrent Chromatography Conference, Chicago (2016). Thu Tran Thi Minh, Binh Nguyen, Peter Winterhalter und Gerold Jerz: Recovery of the betacyanin celosianin II and flavonoid glycosides from Atriplex hortensis var. rubra by HPCCC and off-line ESI-MS/MS monitoring. (Poster) 9. Countercurrent Chromatography Conference, Chicago (2016). ACKNOWLEDGEMENT This PhD would not be done without the supports of my mentor, my supervisor and my family. -
Unconventional Cancer Treatments
Unconventional Cancer Treatments September 1990 OTA-H-405 NTIS order #PB91-104893 Recommended Citation: U.S. Congress, Office of Technology Assessment, Unconventional Cancer Treatments, OTA-H-405 (Washington, DC: U.S. Government Printing Office, September 1990). For sale by the Superintendent of Documents U.S. Government Printing OffIce, Washington, DC 20402-9325 (order form can be found in the back of this report) Foreword A diagnosis of cancer can transform abruptly the lives of patients and those around them, as individuals attempt to cope with the changed circumstances of their lives and the strong emotions evoked by the disease. While mainstream medicine can improve the prospects for long-term survival for about half of the approximately one million Americans diagnosed with cancer each year, the rest will die of their disease within a few years. There remains a degree of uncertainty and desperation associated with “facing the odds” in cancer treatment. To thousands of patients, mainstream medicine’s role in cancer treatment is not sufficient. Instead, they seek to supplement or supplant conventional cancer treatments with a variety of treatments that exist outside, at varying distances from, the bounds of mainstream medical research and practice. The range is broad—from supportive psychological approaches used as adjuncts to standard treatments, to a variety of practices that reject the norms of mainstream medical practice. To many patients, the attractiveness of such unconventional cancer treatments may stem in part from the acknowledged inadequacies of current medically-accepted treatments, and from the too frequent inattention of mainstream medical research and practice to the wider dimensions of a cancer patient’s concerns. -

"Ellagic Acid, an Anticarcinogen in Fruits, Especially in Strawberries: a Review"
FEATURE Ellagic Acid, an Anticarcinogen in Fruits, Especially in Strawberries: A Review John L. Maasl and Gene J. Galletta2 Fruit Laboratory, U.S. Department of Agriculture, Agricultural Research Service, Beltsville, MD 20705 Gary D. Stoner3 Department of Pathology, Medical College of Ohio, Toledo, OH 43699 The various roles of ellagic acid as an an- digestibility of natural forms of ellagic acid, Mode of inhibition ticarcinogenic plant phenol, including its in- and the distribution and organ accumulation The inhibition of cancer by ellagic acid hibitory effects on chemically induced cancer, or excretion in animal systems is in progress appears to occur through the following its effect on the body, occurrence in plants at several institutions. Recent interest in el- mechanisms: and biosynthesis, allelopathic properties, ac- lagic acid in plant systems has been largely a. Inhibition of the metabolic activation tivity in regulation of plant hormones, for- for fruit-juice processing and wine industry of carcinogens. For example, ellagic acid in- mation of metal complexes, function as an applications. However, new studies also hibits the conversion of polycyclic aromatic antioxidant, insect growth and feeding in- suggest that ellagic acid participates in plant hydrocarbons [e.g., benzo (a) pyrene, 7,12- hibitor, and inheritance are reviewed and hormone regulatory systems, allelopathic and dimethylbenz (a) anthracene, and 3-methyl- discussed in relation to current and future autopathic effects, insect deterrent princi- cholanthrene], nitroso compounds (e.g., N- research. ples, and insect growth inhibition, all of which nitrosobenzylmethylamine and N -methyl- N- Ellagic acid (C14H6O8) is a naturally oc- indicate the urgent need for further research nitrosourea), and aflatoxin B1 into forms that curring phenolic constituent of many species to understand the roles of ellagic acid in the induce genetic damage (Dixit et al., 1985; from a diversity of flowering plant families. -

Betanin, the Main Pigment of Red Beet
Betanin, the main pigment of red beet - molecular origin of its exceptionally high free radical scavenging activity Anna Gliszczyńska-Świglo, Henryk Szymusiak, Paulina Malinowska To cite this version: Anna Gliszczyńska-Świglo, Henryk Szymusiak, Paulina Malinowska. Betanin, the main pigment of red beet - molecular origin of its exceptionally high free radical scavenging activity. Food Additives and Contaminants, 2006, 23 (11), pp.1079-1087. 10.1080/02652030600986032. hal-00577387 HAL Id: hal-00577387 https://hal.archives-ouvertes.fr/hal-00577387 Submitted on 17 Mar 2011 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Food Additives and Contaminants For Peer Review Only Betanin, the main pigment of red beet - molecular origin of its exceptionally high free radical scavenging activity Journal: Food Additives and Contaminants Manuscript ID: TFAC-2005-377.R1 Manuscript Type: Original Research Paper Date Submitted by the 20-Aug-2006 Author: Complete List of Authors: Gliszczyńska-Świgło, Anna; The Poznañ University of Economics, Faculty of Commodity Science -
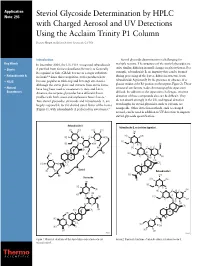
Steviol Glycoside Determination by HPLC with Charged Aerosol and UV Detections Using the Acclaim Trinity P1 Column
Application Note: 293 Steviol Glycoside Determination by HPLC with Charged Aerosol and UV Detections Using the Acclaim Trinity P1 Column Deanna Hurum and Jeffrey Rohrer; Sunnyvale, CA USA Introduction Steviol glycoside determination is challenging for Key Words In December 2008, the U.S. FDA recognized rebaudioside multiple reasons. The structures of the steviol glycosides are quite similar, differing in small changes in glycosylation. For • Stevia A purified from Stevia rebaudiana (Bertoni) as Generally Recognized as Safe (GRAS) for use as a sugar substitute example, rebaudioside B, an impurity that can be formed • Rebaudioside A in foods.1,2 Since this recognition, stevia products have during processing of the leaves, differs in structure from rebaudioside A primarily by the presence or absence of a • HILIC become popular as table-top and beverage sweeteners. Although the stevia plant and extracts from stevia leaves glucose residue at the R1 position on the terpene (Figure 2). These • Natural have long been used as sweeteners in Asia and Latin structural similarities make chromatographic separation Sweeteners America, the terpene glycosides have different flavor difficult. In addition to the separation challenges, sensitive profiles with both sweet and unpleasant bitter flavors.3 detection of these compounds also can be difficult. They Two steviol glycosides, stevioside and rebaudioside A, are do not absorb strongly in the UV, and typical detection largely responsible for the desired sweet flavor of the leaves wavelengths for steviol glycosides, such as 210 nm, are (Figure 1), with rebaudioside A preferred for sweeteners.4 nonspecific. Other detection methods, such as charged aerosol, can be used in addition to UV detection to improve steviol glycoside quantification. -
Application A1108 Rebaudioside M As a New Steviol Glycoside Intense
Supporting document 1 Risk and technical assessment report – Application A1108 Rebaudioside M as a New Steviol Glycoside Intense Sweetener Executive summary Rebaudioside M is similar in chemical structure and sweetness intensity to other currently permitted steviol glycosides. The production of rebaudioside M preparations, analytical methods, specifications and stability are similar to other steviol glycosides. Rebaudioside M occurs naturally in the leaves of the stevia plant at much lower concentrations than several other steviol glycosides so specific concentration and purification steps are required to produce preparations containing high concentrations of rebaudioside M. As for other steviol glycosides, rebaudioside M is hydrolysed completely to steviol by gut microflora. The existing acceptable daily intake (ADI) for steviol glycosides of 0– 4 mg/kg bodyweight, which is expressed on the basis of steviol, is therefore applicable to rebaudioside M. Rebaudioside M-containing preparations are intended for use in the same food categories and at the same use-levels already permitted for other steviol glycoside products. FSANZ has previously conducted a dietary exposure assessment using the current permissions for steviol glycosides and therefore no dietary exposure assessment was necessary for this Application. It is concluded that the use of rebaudioside M as a food additive in accordance with the current permissions for steviol glycosides raises no public health and safety concerns. 1 Table of Contents EXECUTIVE SUMMARY ........................................................................................................................ -

Apricot Kernel Oil (AKO)
RISK PROFILE Apricot kernel oil (AKO) C A S N o . 72869- 69- 3 Date of reporting 31.05.201 3 Content of document 1. Identification of substance ……………………………………………………… p. 1 2. Uses and origin ……………………………………………………… p. 7 3. Regulation ………………………………………………………………………… p. 10 4. Relevant toxicity studies ……………………………………………………… p. 10 5. Exposure estimates and critical NOAEL/NOEL …………………………………… p. 16 6. Other sources of exposure than cosmetic products …………………………. p. 19 7. Assessment ………………………………………………………………………… p. 23 8. Conclusion ………………………………………………………………………… p. 24 9. References ………………………………………………………………………… p. 25 10. Annexes ………………………………………………………………………… p. 29 1. Identification of substance Chemical name (IUPAC): Apricot kernel oil INCI PRUNUS ARMENIACA KERNEL OIL Synonyms Apricot oil CAS No. 72869-69-3 EINECS No. 272-046-1 / - Molecular formula Chemical structure Molecular weight Contents (if relevant) AKO is the fixed oil expressed from the kernels of the Apricot, Prunus armeniaca L., Rosaceae AKO meant for cosmetic purposes is usually produced by cold pressing of the kernel (seed) of wild (bitter) apricots (Asma BM et al 2007, Dwivedi DH et al 2008). A typical composition of such a seed is as follows (Azou Z et al 2009): (w/w) Risk profile Apricot kernel oil Page 1 of 36 Version date: 31MAY2013 Fat (triglycerides): 50.3 % Protein 27.8 % Sugar 11.3 % Fiber 3.1 % Moisture 5.5 % Ash 2.2 % Annex 1 shows a more detailed chemical composition of the seed according to the Phytochemical database of the American Department of Agriculture1. A combination of cold pressing and solvent extraction (petroleum ether, hexane, chloroform-methanol or methanol) yield an AKO that consists of the lipids 92 – 98 %. Besides, that oil consists of smaller amounts of phytosterols like beta-sitosterol. -

GRAS Notice 821 for Glucosylated Steviol Glycosides
GRAS Notice (GRN) No. 821 https://www.fda.gov/food/generally-recognized-safe-gras/gras-notice-inventory {Ri~(C~ij\;#~[Q) NOV I 9 2018 16 November 20 l 8 OFFICE OF FOOD ADDITIVE SAFETY Dr. Paulette Gaynor Office of Food Additive Safety (HFS-200) Center for Food Safety and Applied Nutrition (CFSAN) Food and Drug Administration 500 l Campus Drive College Park, MD 20740 USA Dear Dr. Gaynor: Re: GRAS Notice for High-Purity Glucosylated Steviol Glycosides In accordance with 21 CFR § 170 Subpart E consisting of§ 170.203 through 170.285, Haigen-BGG Natural Ingredients (HBNI) Limited [l 1038, 11/F, Tower A, Gateway Square No. 18, Xiaguangli, North Road East Third Ring, Chaoyang District, Beijing, China], as the notifier, is submitting one hard copy and one electronic copy (on CD), of all data and information supporting the company's conclusion that high-purity glucosylated steviol glycosides, as manufactured by HBNI, is GRAS under the specified conditions of use as a food ingredient on the basis of scientific procedures, and therefore are not subject to the premarket approval requirements of the Federal Food, Drug and Cosmetic Act. Information setting forth the basis for HBNI's GRAS conclusion, as well as a consensus opinion of an independent panel of experts, also are enclosed for review by the agency. l certify that the enclosed electronic files were scanned for viruses prior to submission and are thus certified as being virus-free using Symantec Endpoint Protection 12.1.5. Should you have any questions or concerns regarding this GRAS notice, please do not hesitate to contact me at any point during the review process so that we may provide a response in a timely manner.