A PDF File of “All Tied up and No Place To
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fictional Narratives and the Social Cognition of Mating
challenges Article Tie-Up Cycles in Long-Term Mating. Part II: Fictional Narratives and the Social Cognition of Mating Lorenza Lucchi Basili 1,† and Pier Luigi Sacco 2,3,4,*,† 1 Independent Researcher, 20 Chestnut Street, Cambridge, MA 02139, USA; [email protected] 2 metaLAB (at) Harvard, 42 Kirkland Street, Cambridge, MA 02138, USA 3 Boylston Hall, Harvard University, Cambridge, MA 02138, USA 4 Department of Humanities and Geography, IULM University, via Carlo Bo, 1, 20143 Milan, Italy * Correspondence: [email protected] or [email protected]; Tel.: +39-02-89141-2604 † These authors contribute equally to this work. Academic Editor: Palmiro Poltronieri Received: 23 October 2016; Accepted: 9 February 2017; Published: 20 February 2017 Abstract: In the first part of this paper, we have introduced a novel theoretical approach to mating dynamics, known as Tie-Up Theory (TU). In this second part, in the context of the bio-cultural approach to literature, that assigns to fictional narratives an important valence of social cognition, we apply the conceptual tools presented in the first part to the analysis of mating-related interaction dynamics in some blockbuster Hollywood movies from WWII to today. The interaction dynamics envisioned by our theory accurately reflect, to a significant level of detail, the narrative development of the movies under exam from the viewpoint of the mating dynamics of the couple of main characters, accounting for the specific reasons that lead them to react to certain situations via certain behaviors, and for the reasons why such behaviors lead to certain outcomes. Our analysis seems thus to bring some further legitimacy to the bio-cultural foundation of the narrative structure of the movies that we analyze, and moreover to the idea that it is possible to ‘inquire’ characters about their choices according to the narratological-experimental lines suggested by some proponents of the bio-cultural approach. -

Tied up in Knots New Report Exposes the Truth Behind Britain’S Musculoskeletal Health
All tied up in knots New report exposes the truth behind Britain’s musculoskeletal health 2 Contents Page Foreword: What works for an age old problem? 2 Section 1: Fairer sex face an unfair burden 4 Section 2: Time takes a toll 6 Section 3: Body of evidence 8 Section 4: As stiff as a board 10 Section 5: Simply the best approach 13 About Simplyhealth 16 Did you know: Stats and facts from ShARP 18 Foreword: What works for an age old problem? Every year in the UK 20% of the population present with A poll of 1,000 people who suffer aches and pains a new onset or recurrence of a musculoskeletal problem.1 commissioned by the Simplyhealth Advisory Research Panel In fact, musculoskeletal disorders (MSDs) are the most (ShARP), found that more than a third (35%) take to their common work related problem in Europe2, the most beds in the hope it will ease their pain. Exercise, such as common cause of physical disability3 and the biggest reason yoga7 and workouts guided by a physiotherapist,8 is proven to for long term treatment.4 Musculoskeletal disorders can improve spinal aches and pains, but only 6% of sufferers use affect the body’s muscles, ligaments, tendons, nerves and it to relieve their symptoms and almost half (42%) say pain joints, and most commonly result in back pain, knee pain, prevents them from exercising as much as they would like. neck and shoulder pain, hip and limb pain. Team GB kayaker, sports scientist and physiotherapist, Paul A recent study5 into how we manage our musculoskeletal Hobrough from ShARP notes: “There is a real danger that health reveals that two out of five Britons believe that by people can become trapped in a vicious cycle with lack of resting, their musculoskeletal condition will improve, what exercise leading to increased stiffness, pain and muscle they don’t realise is that it could in fact be making it worse. -

Paradigms of Restraint
02__MURPHY.DOC 5/27/2008 1:44:55 PM PARADIGMS OF RESTRAINT ERIN MURPHY† ABSTRACT Incapacitation of dangerous individuals has conventionally entailed the exercise of physical control over an actual body: the state confines the person in jail. But advances in technology have changed that convention. A variety of new technologies—such as GPS tracking bracelets, biometric scanners, online offender indexes, and DNA databases—give the government power to control dangerous persons without relying on any exertion of physical control. The government can track the location of a person in real time, receive remote notification that an individual has ingested alcohol, or electronically zone someone into a home or out of a public park. It can prove conclusively that a particular person wore a hat or took a sip from a discarded soda can, or identify a single face in a ten thousand–person crowd. In this day and age, restraint of the dangerous can be as much about keeping people out of a place as it used to be about locking them up in one. But whereas physical incapacitation of dangerous persons has always invoked some measure of constitutional scrutiny, virtually no legal constraints circumscribe the use of its technological counterpart. Across legal doctrines, courts erroneously treat physical deprivations Copyright © 2008 by Erin Murphy. † Assistant Professor, University of California, Berkeley (Boalt Hall). I owe a debt of gratitude to Carol Steiker, who invited me to participate in the Conference on Criminal Procedure Stories at Harvard Law School at which a preliminary version of this work was given, and to Dan Richman, whose superb piece on United States v. -

As We Forgive Those
City University of New York (CUNY) CUNY Academic Works Dissertations and Theses City College of New York 2013 As We Forgive Those Therese O'Neil CUNY City College How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/cc_etds_theses/401 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] As We Forgive Those By Tracy O’Neill Mentor: Salar Abdoh April 30, 2013 Submitted in partial fulfillment of the requirements for the degree of Master of Fine Arts at the City College of the City University of New York. 1 CUT HIM Most all the stories Ted tells are quoting movies, and some of the movies are even movies we’ve seen together, but I don’t let on that I know. Problems are intrepid to all of us. Like last month, we’re at the Silver Dollar Stack pancake house, when bang! We’ve reared right back into this guy’s minivan. Guy gets out real steamed, saying he’s going to call 911 and get the police over. My mind is spinning like bicycle pedals on a downhill. I’ve got a D‐Dub from driving home from a high school party nine months back, and here we are in the parking lot not having learned our lesson, Ted drinking rum in his orange juice. I can see the whole scenario in cop eyes. “Dump it,” I told Ted. -
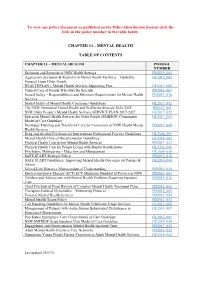
Chapter 13 – Mental Health Table of Contents
To view any policy document as published on the Policy Distribution System click the link on the policy number in the table below. CHAPTER 13 – MENTAL HEALTH TABLE OF CONTENTS CHAPTER 13 – MENTAL HEALTH PD/IB/GL NUMBER Seclusion and Restraint in NSW Health Settings PD2020_004 Aggression, Seclusion & Restraint in Mental Health Facilities – Guideline GL2012_005 Focused Upon Older People HEALTHPLAN – Mental Health Services Supporting Plan GL2012_006 Clinical Care of People Who May Be Suicidal PD2016_007 Sexual Safety – Responsibilities and Minimum Requirements for Mental Health PD2013_038 Services Sexual Safety of Mental Health Consumers Guidelines GL2013_012 The NSW Aboriginal Mental Health and Wellbeing Strategy 2020-2025 IB2021_002 NSW Older People’s Mental Health Services SERVICE PLAN 2017-2027 GL2017_022 Specialist Mental Health Services for Older People (SMHSOP) Community GL2017_003 Model of Care Guideline Discharge Planning and Transfer of Care for Consumers of NSW Health Mental PD2019_045 Health Services Drug and Alcohol Psychosocial Interventions Professional Practice Guidelines GL2008_009 Mental Health Clinical Documentation Guidelines GL2014_002 Physical Health Care within Mental Health Services PD2017_033 Physical Health Care for People Living with Mental Health Issues GL2021_006 Psychiatric Malingering – Detection and Management GL2009_016 SAFE START Strategic Policy PD2010_016 SAFE START Guidelines: Improving Mental Health Outcomes for Parents & GL2010_004 Infants School-Link Initiative Memorandum of Understanding PD2010_020 -
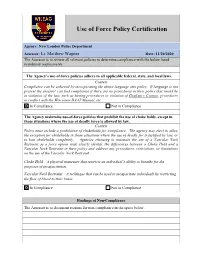
Use of Force Policy Certification
Use of Force Policy Certification Agency: New London Police Department Assessor: Lt. Matthew Wagner Date: 11/20/2020 The Assessor is to review all relevant policies to determine compliance with the below listed mandatory requirements. The Agency’s use-of-force policies adhere to all applicable federal, state, and local laws. Context Compliance can be achieved by incorporating the above language into policy. If language is not present the assessor can find compliance if there are no procedures in their policy that would be in violation of the law, such as having procedures in violation of Graham v Connor, procedures in conflict with the Wisconsin DAAT Manual, etc. In Compliance Not in Compliance The Agency maintains use-of-force policies that prohibit the use of choke holds, except in those situations where the use of deadly force is allowed by law. Context Policy must include a prohibition of chokeholds for compliance. The agency may elect to allow the exception for chokeholds in those situations where the use of deadly for is justified by law, or to ban chokeholds completely. Agencies choosing to maintain the use of a Vascular Neck Restraint as a force option must clearly identify the differences between a Choke Hold and a Vascular Neck Restraint in their policy and address any procedures, restrictions, or limitations on the use of the Vascular Neck Restraint. Choke Hold – A physical maneuver that restricts an individual’s ability to breathe for the purposes of incapacitation. Vascular Neck Restraint – A technique that can be used to incapacitate individuals by restricting the flow of blood to their brain. -

Labette Health
LABETTE HEALTH POLICY AND PROCEDURE SUBJECT: RESTRAINT REFERENCE:A/N/SWING BED/ER APPROVED BY: Restraint Committee PAGE 1 OF 10 EFFECTIVE: SEPT/97 REVISED: FEB/JULY99 MAR/01, JAN/02, OCT/03, DEC/03 AUG/05/MAY/07/JULY/08, APR/09, OCT/09, APRIL/12 TITLE: RESTRAINT DEFINITIONS: A restraint is any manual method, physical or mechanical device, material, or equipment that immobilizes or reduces the ability of a patient to move his or her arms, legs, body, or head freely; or a drug or medication when it is used as a restriction to manage the patient’s behavior or restrict the patient’s freedom of movement and is not a standard treatment or dosage for the patient’s condition. Patients Who May Require Restraint 1. Non-violent or non-self destructive patients (Medical): patients who require restraints to prevent removal of tubes, lines, dressings, or to support medical healing or well-being. 2. Violent or self-destructive patients (Behavior): patients who display severely aggressive or destructive behavior that jeopardizes the immediate physical safety of the patient, staff, or others. This category includes patients for which a Dr. Strong might be called. POLICY: 1. It is the intent of Labette Health to be Restraint free. 2. All patients have the right to be free from restraints or seclusion of any form, imposed as a means of coercion, discipline, convenience, or retaliation by staff. 3. Labette Health does not use seclusion as a form of restraint. 4. Restraints shall be used only where alternative methods are not sufficient to protect patients or others from injury. -
Restraint Prevalence Tools
Restraint Prevalence Tools NURSING BEST PRACTICE GUIDELINES EVALUATION USER GUIDE November 2006 Disclaimer The opinions expressed in this publication are those of the authors. Publication does not imply any endorsement of these views by either of the participating partners of the Nursing Best Practice Research Unit, which include members of the University of Ottawa faculty and members of the Registered Nurses’ Association of Ontario (RNAO). 158 Pearl Street / 158, rue Pearl School of Nursing / Toronto ON M5H 1L3 CANADA École des sciences infirmières 451 Smyth 416 599-1925 Ottawa ON K1H 8M5 CANADA 416 599-1926 613 562-5800 (8407) 613 562-5658 http://www.nbpru.ca/ Nursing Best Practice Guidelines Evaluation User Guide Copyright © 2006 by the NBPRU Printed in Ottawa, Ontario, Canada All rights reserved. Reproduction, in whole or in part, of this document without the acknowledgement of the authors and copyright holder is prohibited. The recommended citation is: Davies B, Danseco E, Ploeg J, Heslin, K, Stansfield M, Santos J & Edwards, N. (2006). Nursing Best Practice Guideline Evaluation User Guide: Restraint Prevalence Tools. Nursing Best Practice Research Unit, University of Ottawa, Canada. pp. 1-20. Nursing Best Practice Guidelines Evaluation User Guide Acknowledgements This user guide was based on an evaluation project awarded to Barbara Davies and Nancy Edwards with the Registered Nurses’ Association of Ontario (RNAO) and funded by the Government of Ontario. The authors are grateful for the support of the Nursing Secretariat of the Ministry of Health and Long-Term Care (MOHLTC), in particular the Chief Nursing Officer, Sue Matthews. The authors would also like to acknowledge the contributions of Tazim Virani and RNAO staff, clinical sites that pilot-tested the evaluation tool, members of the evaluation team and project staff. -
Best Practices in the Use of Restraints with Pregnant Women and Girls Under Correctional Custody
BEST PRACTICES IN THE USE OF RESTRAINTS WITH PREGNANT WOMEN AND GIRLS UNDER CORRECTIONAL CUSTODY Purpose of the Best Practices Statement The National Task Force on the Use of Restraints with Pregnant Women under Correctional Custody, initially convened by the U.S. Department of Justice in 2011, created this best practices statement to articulate a set of principles to guide agencies and jurisdictions in the development of local policy and practice. These best practices are relevant across a variety of settings including criminal justice, juvenile justice, psychiatric and forensic hospitals, law enforcement transport, and others. This document refers and applies to both women (age 18 years and older) and girls (younger than age 18) who are pregnant, laboring and delivering, or in the post-partum period. This statement is not a proscribed policy. Rather, it should serve as a starting point for individual organizations to use in developing effective internal policies, procedures, and practices that maximize safety and minimize risk for pregnant women and girls, their fetuses/newborns, and correctional and medical staff. Bureau of Justice Assistance U.S. Department of Justice ACKNOWLEDGMENT. The development of this document was sponsored by the Bureau of Justice Assistance, Office of Justice Programs (OJP), U.S. Department of Justice (DOJ). It was prepared by the National Association of State Mental Health Program Directors (NASMHPD) under Contract No. HHSS2832007000201 awarded by SAMHSA, and by the National Resource Center on Justice-Involved Women under Grant No. 2010-DJ-BX-K080 awarded by DOJ. It was written by Kristen King, MPS, from Advocates for Human Potential, Inc., with editorial oversight by Madeline Carter and Rachelle Ramirez from the Center for Effective Public Policy, contributions from Richard P. -

Directive 5.11 PRISONER TRANSPORT
Athens-Clarke County Police Department Directive 5.11 PRISONER TRANSPORT Effective Date: May 28, 2020 Cancels: B1/13/07, B1/13/03, A3/03/09 Updated Date: Section(s): SME Review Date: Updated Date: Section(s): May 28, 2022 Updated Date: Section(s): CONTENTS 5.11.1 POLICY AND PURPOSE 5.11.2 DEFINITIONS 5.11.3 RULES/RESPONSIBILITIES 5.11.4 TRANSPORTING NON-ARRESTEES 5.11.5 POSITIONAL ASPHYXIA 5.11.6 PROCEDURES 5.11.7 TRAINING 5.11.1 POLICY AND PURPOSE The purpose of this Directive is to establish procedures and guidelines whereby prisoners, persons living with a mental illness, or persons in the custody of the police will be transported. It is the policy of the Athens-Clarke County Police Department that all prisoners, persons living with a mental illness, or persons in the custody of the police will be transported in a manner that provides maximum security and safety of the prisoner, the public, and the transporting officer. 5.11.2 DEFINITIONS Flex-Cuff – a plastic strip that can be fastened as a restraint around a person’s wrists or ankles. Handcuffs – restraint devices designed to secure a person’s wrists close together. 5.11 PRISONER TRANSPORT PAGE 2 Ripp Hobble – a one-inch wide webbed belting designed to be used in various situations to secure the legs and ankles of an individual. Leg-Iron/Shackle – a kind of physical restraint used on the feet or ankles. Positional Asphyxia – a condition which may be caused or exacerbated by stress owing to the position of the body, with the stress influencing or inhibiting respiration. -

Mechanical Restraint in Psychiatric Healthcare Facilities
Mechanical restraint in psychiatric healthcare facilities A helpful tool, or torture or other cruel, inhuman or degrading treatment or punishment in disguise? Julia Rudhe Faculty of Law at Stockholm University Thesis 30 ECTS Subject: Public International Law Spring semester 2021 Supervisor: Per Ahlin Abstract The use of mechanical restraint is a common practice in psychiatric care, often defended by medical necessity but seldom questioned from a human rights per- spective. The purpose of this thesis has been to investigate under which circum- stances mechanical restraint by bed through belt fixation could amount to torture and other cruel, inhuman or degrading treatment or punishment. Persons with psychosocial disabilities are in a particularly vulnerable situation and as the Inter- national Convention on the Rights of Persons with Disabilities (CRPD) is the most comprehensive rights framework for this group, it has been discussed whether the CRPD sets out additional safeguards in relation to restraint. A legal doctrinal approach is the basic methodology used in order to outline the current international and European legal framework on torture and other ill- treatment and disability rights. A survivor-controlled research methodology has been applied and to amplify other voices of persons with firsthand experience of being mechanically restrained, interviews have been conducted with persons from Sweden and Spain. Healthcare professionals have also been interviewed. A feminist perspective on the law is applied. Different international conventions and bodies of the United Nations have diverse interpretations on what acts or omissions that amount to torture and other cruel, inhuman or degrading treatment or punishment, although there is an aim and will to streamline the conventions. -

Dedicated to the Needs of the Music/Rec Albums
DEDICATED TO THE NEEDS OF THE MUSIC/REC STRY SEPTEMBER 10, (977 $1.75 SINGLES ALBUMS RITA COOLIDGE, "WE'RE ALL ALONE" (prod. by ALAN O'DAY, "STARTED OUT DANCING, LINDA RONSTADT, "SIMPLE DREAMS." David Anderle) (writer: Boz Scaggs) ENDED UP MAKING LOVE" (prod. by From the album artwork to the record (Boz Scaggs, ASCAP) (3:38). This Steve Barri) (writer: O'Day) (WB, contained within, this is Ronstadt's superb Scaggs ballad was never a ASCAP) (3:21). "Undercover Angel" finest achievement to date. She is in single for the writer, but should be brought O'Day to number one with classic form with Roy Orbison's "Blue Coolidge's second straight pop hit. his first record, and this disco -ori- Bayou," Buddy Holly's "It's So Eeasy" She sings it with feeling and re- ented 'ollow-up has the same play- and the Stones' "Tumbling Dice" while straint. With her album in the top 20, ful eroticism and hook -filled struc- the ballads reflect an introspective side top 40 should react quickly. A&M ture. Look for a speedy chart return. with a sparse arrangement underpin- 1965. Pacific 002 (Atlantic). ning her voice. Asylum 6E-104 (7.98). JIMMY BUFFETT, "CHANGES IN LATITUDES, ART GARFUNKEL, "CRYING IN MY SLEEP" DARYL HALL AND JOHN OATES, CHANGES IN ATTITUDES" (prod. by (prod. by Art Garfunkel & Barry "BEAUTY ON A BACKSTREET." The Norbert Putnam) (writer: Jimmy Buf- Beckett) (writer: Jimmy Webb) (Can- group continues to ride the peak of fett) (Coral Reefer / Outer Banks, opy, ASCAP) (4:00). The first offering their success with this strong follow-up BMI) (3:15).