House of Representatives State of Delaware 411
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

151St General Assembly Legislative Guide 151St General Assembly Legislative Guide
151st General Assembly Legislative Guide 151st General Assembly Legislative Guide Senate – Table of Contents …………………………….…………………………...…….. i House of Representatives – Table of Contents ..….……………………..…….…...… ii General Assembly Email and Phone Directory ……………………………………..... iv Senate – Legislative Profiles ………………………………………………...………….... 1 House of Representatives – Legislative Profiles …..……………..……………….... 23 Delaware Cannabis Advocacy Network P.O. Box 1625 Dover, DE 19903 (302) 404-4208 [email protected] 151st General Assembly – Delaware State Senate DISTRICT AREA SENATOR PAGE District 1 Wilmington North Sarah McBride (D) 2 District 2 Wilmington East Darius Brown (D) 3 District 3 Wilmington West Elizabeth Lockman (D) 4 District 4 Greenville, Hockessin Laura Sturgeon (D) 5 Heatherbrooke, District 5 Kyle Evans Gay (D) 6 Talleyville District 6 Lewes Ernesto B. Lopez (R) 7 District 7 Elsmere Spiros Mantzavinos (D) 8 District 8 Newark David P. Sokola (D) 9 District 9 Stanton John Walsh (D) 10 District 10 Middletown Stephanie Hansen (D) 11 District 11 Newark Bryan Townsend (D) 12 District 12 New Castle Nicole Poore (D) 13 District 13 Wilmington Manor Marie Pinkney (D) 14 District 14 Smyrna Bruce C. Ennis (D) 15 District 15 Marydel David G. Lawson (D) 16 District 16 Dover South Colin R.J. Bonini (R) 17 District 17 Dover, Central Kent Trey Paradee (D) 18 District 18 Milford David L. Wilson (R) 19 District 19 Georgetown Brian Pettyjohn (R) 20 District 20 Ocean View Gerald W. Hocker (R) 21 District 21 Laurel Bryant L. Richardson (R) 22 151st General Assembly – Delaware House of Representatives DISTRICT AREA REPRESENTATIVE PAGE District 1 Wilmington North Nnamdi Chukquocha (D) 24 District 2 Wilmington East Stephanie T. Bolden (D) 25 District 3 Wilmington South Sherry Dorsey Walker (D) 26 District 4 Wilmington West Gerald L. -
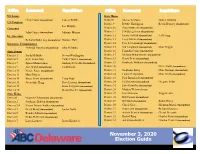
Informational Brochure
US Senate State House Chris Coons (incumbent) Lauren Witzke District8 Sherae’A Moore Daniel Zitofsky US Congress District 9 Debbie Harrington Kevin Hensley (incumbent) Lee Murphy Governor District 10 Sean Matthews (incumbent) John Carney (incumbent) Julianne Murray District 11 Jeff Spiegelman (incumbent) Lt. Governor District 12 Krista Griffith (incumbent) Jeff Cragg Bethany Hall-Long (incumbent) Donyale Hall District 13 Larry Mitchell (incumbent) Insurance Commissioner District 14 Pete Schwartzkopf (incumbent) Trinidad Navarro (incumbent) Julia Pillsbury District 15 Val Longhurst (incumbent) Mike Higgin State Senate District 16 Franklin Cooke (incumbent) District 1 Sarah McBride Steven Washington District 17 Melissa Minor-Brown (incumbent) District 5 Kyle Evans Gay Cathy Cloutier (incumbent) District 18 David Benz (incumbent) District 7 Spiros Mantzavinos Anthony Delcollo (incumbent) District 19 Kimberly Williams (incumbent) District 9 Jack Walsh (incumbent) Todd Ruckle District 20 Steve Smyk (incumbent) District 12 Nicole Poore (incumbent) District 21 Stephanie Barry Mike Ramone (incumbent) District 13 Mary Pinkey District 22 Luann D’Agostino Mike Smith (incumbent) District 14 Bruce Ennis (incumbent) Craig Pugh District 23 Paul Baumbach (incumbent) District 15 Jacqueline Hugg Dave Lawson (incumbent) District 24 Ed Osienski (incumbent) Gregory Wilps District 19 Brian Pettyjohn (incumbent) District 25 John Kowalko (incumbent) District 20 Gerald Hocker (incumbent) District 26 Madina Wilson-Anton State House District 27 Eric Morrison Tripp -

ACTION REQUESTED on Tuesday, May 30, 2017, the Delaware Joint Finance Committee
Rehoboth Beach-Dewey Beach Chamber of Commerce & Visitors Center P. O. Box 216 *501 Rehoboth Avenue, Rehoboth Beach, DE 19971 - 302-227-2233 *800-441-1329 *Hotline 302-227-6446 *Fax 302-227-8351 - [email protected] *www.beach-fun.com TIME SENSITIVE – ACTION REQUESTED On Tuesday, May 30, 2017, the Delaware Joint Finance Committee (JFC) voted to eliminate the current 1% allocated funding to all State Convention & Visitor Bureaus (CVB’s), which is currently a portion of the 8% lodging tax collected by hotels and motels Statewide. This would also terminate the portion of the same 1% which is currently distributed to all Chambers of Commerce in Sussex County. The allocation to Chambers in Sussex is tied to stringent requirements with regard to marketing expenditures and recorded proof of return on investment. On Wednesday, May 31, 2017, the Rehoboth Beach Dewey Beach Chamber of Commerce (RBDBCC) Legislative Representative, Mark Lally, as well as several of our tourism partners and Carol Everhart, met at Legislative Hall in the hope that there would be an opportunity to address the JFC. The operating procedure in place did not allow that opportunity. Below you will find a list of the current JFC members. We are seeking your assistance in personally contacting members of the JFC and/or your legislators by phone or in person to seek their support. We did not provide e-mails, as legislators are more receptive to personal contact. If 7 of the 12 member JFC vote in favor, the 1% could be placed back into the budget. The loss of this allocated revenue would, at a minimum, deplete or severely cut the marketing ability for Sussex Chambers, and in some cases, could put them out of business. -

Delaware Elections Roadmap
DELAWARE ELECTIONS ROADMAP September 28, 2018 REGISTERED VOTERS 2018 v. 2010 COUNTY DEMOCRATS REPUBLICANS OTHERS TOTAL KENT 52,794 36,735 33,129 122,658 NEW CASTLE 213,679 92,335 100,261 406,275 2018 SUSSEX 60,525 64,050 39,397 163,972 STATEWIDE 326,998 193,120 172,787 692,905 KENT 46,243 33,005 25,554 105,763 NEW CASTLE 196,665 101,895 88,232 391,654 2010 SUSSEX 51,936 49,106 26,761 128,723 STATEWIDE 294,844 184,006 140,547 626,140 September 28, 2018 Source: elections.delaware.gov FEDERAL RACES U.S. SENATE U.S. HOUSE Democrat Democrat Thomas R. Carper Lisa Blunt Rochester (Incumbent) (Incumbent) Republican Republican Robert B. Arlett Scott Walker September 28, 2018 STATE RACES TREASURER AUDITOR ATTORNEY GENERAL Republican Democrat Democrat Kenneth A. Simpler Kathleen K. McGuiness Kathy Jennings (Incumbent) Democrat Republican Republican Colleen Davis James Spadola Bernard Pepukayi September 28, 2018 2016 – 2018 GENERAL ASSEMBLY SENATE HOUSE 11 – 10 25 – 16 Democrat Majority Democrat Majority September 28, 2018 KEY VOTES FOR DSCC DSCC Identified 4 Key Bill Votes in the 149th General Assembly (2016-2018) that were priorities for the business community. HB226-Created the Delaware Prosperity Partnership (DPP), to attract new business to Delaware (DSCC Supported) HB190-Modernized Delaware’s Coastal Zone Act (CZA) to allow for redevelopment of 14 underutilized/abandoned properties (DSCC Supported) HB170-Created a tax credit for investment in small tech startups (DSCC Supported) SB170-Increased Delaware’s Minimum Wage (DSCC Opposed) September 28, 2018 2018 ISSUES TO WATCH Impacting Federal and State Races • What, if any, fallout from proposed gun legislation will impact fundraising and voter turnout • How will the Carper U.S. -

A Listing of Delaware Elected Officials Compiled by the League of Women Voters of Delaware, Inc
(Subject to change 4/5/2021) They Represent You 2020-2022 (Revision II) A listing of Delaware elected officials compiled by the League of Women Voters of Delaware, Inc. as a public service (302) 571-8948 United States Party/ Name Address Office Telephone E-mail Address Term Expires President (D) Joseph R. Biden, Jr. The White House (202) 456-6213 Comment line (4 Yrs.) 2024 1600 Pennsylvania Ave. NW (202) 456-1414 www.whitehouse.gov/contact Vice President (D) Kamala Harris Washington, DC 20500 (202) 456-1414 (4 Yrs.) 2024 www.whitehouse.gov/administration/vice-president-harris Senators (D) Thomas R. Carper 513 Hart Senate Office Bldg. (202) 224-2441 DC (6 Yrs.) 2024 Washington, DC 20510 (302) 573-6291 NC Carper.Senate.gov (contact via web page) (302) 674-3308 K (302) 856-7690 S (D) Christopher A. Coons 127 A Russell Senate Office Bldg. (202) 224-5042 DC (6 Yrs.) 2026 Washington, DC 20510 (302) 573-6345 NC Coons.Senate.gov/contact (302) 736-5601 K &S chriscoons.com Representative (D) Lisa Blunt Rochester 1519 Longworth House Office Bldg. (202) 225-4165 DC bluntrochester.house.gov (2 Yrs.) 2022 Washington, DC 20515 (302) 830-2330 NC (contact via web page) (302) 858-4773 SC State Party/Name Address (Area code for DE is 302) Office Telephone E-mail Address Term Expires Governor (D) John C. Carney, Jr. 150 Martin Luther King Jr., Blvd. South 1-800 292-9570 [email protected] (4 Years) 2024 Dover, DE 19901 744-4101 K 577-3210 NC Lt. Governor (D) Bethany A. -
2016-Year-End-Political-Report.Pdf
1 Verizon Political Activity January – December 2016 A Message from Craig Silliman Verizon is affected by a wide variety of government policies -- from telecommunications regulation to taxation to health care and more -- that have an enormous impact on the business climate in which we operate. We owe it to our shareowners, employees and customers to advocate public policies that will enable us to compete fairly and freely in the marketplace. Political contributions are one way we support the democratic electoral process and participate in the policy dialogue. Our employees have established political action committees at the federal level and in 18 states. These political action committees (PACs) allow employees to pool their resources to support candidates for office who generally support the public policies our employees advocate. This report lists all PAC contributions, corporate political contributions, support for ballot initiatives and independent expenditures made by Verizon and its affiliates during 2016. The contribution process is overseen by the Corporate Governance and Policy Committee of our Board of Directors, which receives a comprehensive report and briefing on these activities at least annually. We intend to update this voluntary disclosure twice a year and publish it on our corporate website. We believe this transparency with respect to our political spending is in keeping with our commitment to good corporate governance and a further sign of our responsiveness to the interests of our shareowners. Craig L. Silliman Executive Vice President, Public Policy and General Counsel 2 Verizon Political Activity January – December 2016 Political Contributions Policy: Our Voice in the Democratic Process What are the Verizon Good Government Clubs? setting of monetary contribution limitations and the The Verizon Good Government Clubs (GGCs) exist to help the establishment of periodic reporting requirements. -

County Council Public/Media Packet
Sussex County Council Public/Media Packet MEETING: MAY 21, 2013 **DISCLAIMER** This product is provided by Sussex County government as a courtesy to the general public. Items contained within are for background purposes only, and are presented ‘as is’. Materials included are subject to additions, deletion or other changes prior to the County Council meeting for which the package is prepared. Sussex County Council 2 The Circle | PO Box 589 Georgetown, DE 19947 (302) 855-7743 A G E N D A MAY 21, 2013 10:00 A.M. Call to Order Approval of Agenda Approval of Minutes Reading of Correspondence Norma Prettyman, Friends of the Greenwood Library – Presentation of Construction Contribution Check Todd Lawson, County Administrator 1. Administrator’s Report 2. Fiscal Year 2014 Budget Presentation 3. Discussion and Possible Introduction of Proposed Ordinances: “AN ORDINANCE ESTABLISHING THE ANNUAL OPERATING BUDGET FOR FISCAL YEAR 2014” “AN ORDINANCE ESTABLISHING ANNUAL SERVICE CHARGES, ANNUAL ASSESSMENT RATES FOR COLLECTION AND TRANSMISSION AND/OR TREATMENT, AND CONNECTION CHARGES FOR ALL SUSSEX COUNTY WATER AND SEWER DISTRICTS” Gina Jennings, Finance Director 1. Financial Report for the Nine Months ending March 31, 2013 Sussex County Council Agenda May 21, 2013 Page 2 of 3 Hal Godwin, Deputy County Administrator 1. Legislative Update Bob Jones, Project Engineer 1. Sussex County Airport Concrete Apron Repairs A. Bid Award Grant Requests 1. Delaware Police Chiefs’ Council for seminar costs. 2. The Mid-Atlantic Symphony Orchestra for operating costs. 3. Ocean View Historical Society for the Coastal Towns Museum Project. 4. Rehoboth Art League to sponsor the annual gala which benefits their education, outreach and tuition assistance programs. -

A Listing of Delaware Elected Officials Compiled by the League of Women Voters As a Public Service (302) 571-8948
(Subject to change 6/17/2021) They Represent You 2020-2022 (Revision III) A listing of Delaware elected officials compiled by the League of Women Voters of Delaware, Inc. as a public service (302) 571-8948 United States Party/ Name Address Office Telephone E-mail Address Term Expires President (D) Joseph R. Biden, Jr. The White House (202) 456-6213 Comment line (4 Yrs.) 2024 1600 Pennsylvania Ave. NW (202) 456-1414 www.whitehouse.gov/contact Vice President (D) Kamala Harris Washington, DC 20500 (202) 456-1414 (4 Yrs.) 2024 www.whitehouse.gov/administration/vice-president-harris Senators (D) Thomas R. Carper 513 Hart Senate Office Bldg. (202) 224-2441 DC (6 Yrs.) 2024 Washington, DC 20510 (302) 573-6291 NC Carper.Senate.gov (contact via web page) (302) 674-3308 K (302) 856-7690 S (D) Christopher A. Coons 127 A Russell Senate Office Bldg. (202) 224-5042 DC (6 Yrs.) 2026 Washington, DC 20510 (302) 573-6345 NC Coons.Senate.gov/contact (302) 736-5601 K &S chriscoons.com Representative (D) Lisa Blunt Rochester 1519 Longworth House Office Bldg. (202) 225-4165 DC bluntrochester.house.gov (2 Yrs.) 2022 Washington, DC 20515 (302) 830-2330 NC (contact via web page) (302) 858-4773 SC State Party/Name Address (Area code for DE is 302) Office Telephone E-mail Address Term Expires Governor (D) John C. Carney, Jr. 150 Martin Luther King Jr., Blvd. South 1-800 292-9570 [email protected] (4 Years) 2024 Dover, DE 19901 744-4101 K 577-3210 NC Lt. Governor (D) Bethany A. -

Bill Seeks to Increase Number of Primary Care Practitioners in Delaware
NEWS: Bill Seeks to Increase Number of Primary Care Practitioners in Delaware Increasing the number of primary care physicians and nurse practitioners serving Delawareans is the goal of a bipartisan bill released from committee this week. Sponsored by State Reps. David Bentz (D-Newark-Christina) and Bryan Shupe (R- Milford South), the measure would create a program that could award education loan repayment grants to new primary care providers of up to $50,000 per year for a maximum of 4 years. Organizations eligible to apply for grants on behalf of their new primary care providers would need to be located in areas of need and accept Medicare and Medicaid participants. Rep. Shupe said the program would be funded through a public-private partnership. The state would dedicate up to $1 million to the initiative, with Delaware health insurers contributing a matching amount. According to 2018 data cited by Rep. Shupe, there are approximately 228 primary care physicians downstate, compared to 587 in New Castle County. Expressed in terms of population, Kent and Sussex counties have a combined 42% of the state's residents, but only 28% of its doctors. A 2016 federal government study projected a growing gap State Rep. Bryan Shupe between demand for primary care physicians in Delaware and availability, which is part of a national trend. The nation's aging population is cited as one of the major factors driving demand. The U.S. population is expected to grow by 10% over the next 12 years, but the number of Americans age 65 and over will jump by 48% during the same period. -

Legislators by School District/Charter
2020-2021 Legislators by School District Appoquinimink District Christina District (suburban) Laurel S 10 Stephanie Hansen S -4 Laura Sturgeon* Chair Senate Educ. S 21 Bryant Richardson S- 12 Nicole Poore S -7 SpirosComm. Mantzavinos H- 39 Daniel B. Short S 14 Bruce Ennis S -8 David Sokola* Sen. Educ. Comm. H- 40 Timothy D. Dukes H- 8 Sherae'a "Rae" Moore* House Educ. Comm. S -9 John Walsh H- 41 Richard Collins* House Educ. Comm. H- 9 Kevin Hensley* House Educ. Comm. S - 10 Stephanie Hansen - Milford District H- 11 Jeffrey N. Spiegelman S -11 Bryan Townsend* Sen. Educ. Comm. S 16 Colin Bonini* Sen. Educ. Comm. H- 27 Eric Morrison* House Educ. Comm. S -12 Nicole Poore S- 18 David Wilson - Brandywine District S -13 Marie Pinkney S- 19 Brian Pettyjohn S 1 Sarah McBride H 5 Kendra Johnson H- 30 W. Shannon Morris S- 2 Darius Brown H- 15 Valerie Longhurst H- 33 Charles Postles Jr.* House Educ. Comm. S- 4 Laura Sturgeon* Chair Senate Educ. H- 18 David Bentz H- 35 Jesse Vanderwende S- 5 KyleComm. Evans Gay H- 21 Michael Ramone* House Educ. Comm. H- 36 Bryan Shupe* House Educ. Comm. H- 1 Nnamdi Chukwuocha* House Educ ViceChair H- 22 Michael Smith* House Educ. Comm. - Red Clay District H- 2 Stephanie Bolden* House Educ. Comm. H- 23 Paul S. Baumbach S 1 Sarah McBride H- 4 Gerald L. Brady H- 24 Edward S. Osienski* House Educ. S- 2 Darius Brown H- 6 Debra J. Heffernan* House Educ. Comm. H- 25 JohnComm. A. Kowalko, Jr.* House Educ. -

A Message from Craig Silliman
1 Verizon Political Contributions January – December 2013 A Message from Craig Silliman Verizon is affected by a wide variety of government policies -- from telecommunications regulation to taxation to health care and more -- that have an enormous impact on the business climate in which we operate. We owe it to our shareowners, employees and customers to advocate public policies that will enable us to compete fairly and freely in the marketplace. Political contributions are one way we support the democratic electoral process and participate in the policy dialogue. Our employees have established political action committees at the federal level and in 20 states. These political action committees (PACs) allow employees to pool their resources to support candidates for office who generally support the public policies our employees advocate. This report lists all PAC contributions, corporate political contributions, support for ballot initiatives and independent expenditures made by Verizon during 2013. The contribution process is overseen by the Corporate Governance and Policy Committee of our Board of Directors, which receives a comprehensive report and briefing on these activities at least annually. We intend to update this voluntary disclosure twice a year and publish it on our corporate website. We believe this transparency with respect to our political spending is in keeping with our commitment to good corporate governance and a further sign of our responsiveness to the interests of our shareowners. Craig L. Silliman Senior Vice President, Public Policy 2 Verizon Political Contributions January – December 2013 Political Contributions Policy: Our Voice in the Political Process What are the Verizon Good Government Clubs? individual state election laws. -

Election Guide Was Created President-Elect RON MACARTHUR PHOTO Day
A special publication by 2 DATEOCTOBER 28 - NOVEMBER 8, 2016 ELECTION #GUIDE 2016 Cape Gazette DELAWARE PUBLIC ARCHIVES PHOTO A RARE DOCUMENT shows coun- ty election returns from 1811. Until 1812, all voting took place in the coun- ty seat Georgetown. Return Day trivia • John M. Clayton of Dags- boro, a U.S. senator and U.S. secretary of state in President Zachery Taylor’s administra- MANY HAPPY tion, put Return Day in per- spective in the mid-1800s. He said “that the man who had been to a political meeting in RETURNS Dagsboro, seen Return Day in Georgetown and visited Paris had witnessed the three most interesting sights in the world” • While there are no records of a president participating in the parade, in 2008 then Vice President-Elect Joe Biden rode in a carriage with his wife, Jill, on the rain soaked streets of Georgetown. That year’s event CLOCKWISE, FROM TOP: Town crier Kirk Lawson reads re- was like no other in history, turns from the 2014 election; Sussex County party leaders, in a complete with metal-detector photo from 1988, Republican J. Everett Moore, Libertarian Bob security checks, Secret Service Sigler and Democrat Ken McDowell prepare to bury the hatch- and sharpshooters et; a historical marker on The Circle explains the unique histo- ry of the one-of-a-kind event in the country; and each Return Day, officials of each political party gather to bury the hatchet • In 1965, the Delaware Gen- in Lewes Beach sand. eral Assembly declared Return PHOTOS: DELAWARE PUBLIC ARCHIVES AND RON MACARTHUR Day as a legal half-day holiday in Sussex County • W.