Breech Presentation and Delivery in Singleton Term Pregnancies in Finland
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
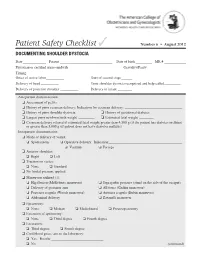
Documenting Shoulder Dystocia
Patient Safety Checklist ✓ Number 6 • August 2012 DOCUMENTING SHOULDER DYSTOCIA Date _____________ Patient _____________________________ Date of birth _________ MR # ____________ Physician or certified nurse–midwife _____________________________ Gravidity/Parity______________________ Timing: Onset of active labor __________ Start of second stage ______ Delivery of head __________ Time shoulder dystocia recognized and help called _________ Delivery of posterior shoulder __________ Delivery of infant ________ Antepartum documentation: ❏ Assessment of pelvis ❏ History of prior cesarean delivery: Indication for cesarean delivery: ________________________________ ❏ History of prior shoulder dystocia ❏ History of gestational diabetes ❏ Largest prior newborn birth weight _________ ❏ Estimated fetal weight ________ ❏ Cesarean delivery offered if estimated fetal weight greater than 4,500 g (if the patient has diabetes mellitus) or greater than 5,000 g (if patient does not have diabetes mellitus) Intrapartum documentation: ❏ Mode of delivery of vertex: ❏ Spontaneous ❏ Operative delivery: Indication: _________________________________________ ❏ Vacuum ❏ Forceps ❏ Anterior shoulder: ❏ Right ❏ Left ❏ Traction on vertex: ❏ None ❏ Standard ❏ No fundal pressure applied ❏ Maneuvers utilized (1): ❏ Hip flexion (McRoberts maneuver) ❏ Suprapubic pressure (stand on the side of the occiput) ❏ Delivery of posterior arm ❏ All fours (Gaskin maneuver) ❏ Posterior scapula (Woods maneuver) ❏ Anterior scapula (Rubin maneuver) ❏ Abdominal delivery ❏ Zavanelli maneuver -

Management of Prolonged Decelerations ▲
OBG_1106_Dildy.finalREV 10/24/06 10:05 AM Page 30 OBGMANAGEMENT Gary A. Dildy III, MD OBSTETRIC EMERGENCIES Clinical Professor, Department of Obstetrics and Gynecology, Management of Louisiana State University Health Sciences Center New Orleans prolonged decelerations Director of Site Analysis HCA Perinatal Quality Assurance Some are benign, some are pathologic but reversible, Nashville, Tenn and others are the most feared complications in obstetrics Staff Perinatologist Maternal-Fetal Medicine St. Mark’s Hospital prolonged deceleration may signal ed prolonged decelerations is based on bed- Salt Lake City, Utah danger—or reflect a perfectly nor- side clinical judgment, which inevitably will A mal fetal response to maternal sometimes be imperfect given the unpre- pelvic examination.® BecauseDowden of the Healthwide dictability Media of these decelerations.” range of possibilities, this fetal heart rate pattern justifies close attention. For exam- “Fetal bradycardia” and “prolonged ple,Copyright repetitive Forprolonged personal decelerations use may onlydeceleration” are distinct entities indicate cord compression from oligohy- In general parlance, we often use the terms dramnios. Even more troubling, a pro- “fetal bradycardia” and “prolonged decel- longed deceleration may occur for the first eration” loosely. In practice, we must dif- IN THIS ARTICLE time during the evolution of a profound ferentiate these entities because underlying catastrophe, such as amniotic fluid pathophysiologic mechanisms and clinical 3 FHR patterns: embolism or uterine rupture during vagi- management may differ substantially. What would nal birth after cesarean delivery (VBAC). The problem: Since the introduction In some circumstances, a prolonged decel- of electronic fetal monitoring (EFM) in you do? eration may be the terminus of a progres- the 1960s, numerous descriptions of FHR ❙ Complete heart sion of nonreassuring fetal heart rate patterns have been published, each slight- block (FHR) changes, and becomes the immedi- ly different from the others. -

00005721-201907000-00003.Pdf
2.0 ANCC Contact Hours Angela Y. Stanley, DNP, APRN-BC, PHCNS-BC, NEA-BC, RNC-OB, C-EFM, Catherine O. Durham, DNP, FNP-BC, James J. Sterrett, PharmD, BCPS, CDE, and Jerrol B. Wallace, DNP, MSN, CRNA SAFETY OF Over-the-Counter MEDICATIONS IN PREGNANCY Abstract Approximately 90% of pregnant women use medications while they are pregnant including both over-the-counter (OTC) and prescription medications. Some medica- tions can pose a threat to the pregnant woman and fetus with 10% of all birth defects directly linked to medications taken during pregnancy. Many medications have docu- mented safety for use during pregnancy, but research is limited due to ethical concerns of exposing the fetus to potential risks. Much of the information gleaned about safety in pregnancy is collected from registries, case studies and reports, animal studies, and outcomes management of pregnant women. Common OTC categories of readily accessible medications include antipyretics, analgesics, nonsteroidal anti- infl ammatory drugs, nasal topicals, antihistamines, decongestants, expectorants, antacids, antidiar- rheal, and topical dermatological medications. We review the safety categories for medications related to pregnancy and provide an overview of OTC medications a pregnant woman may consider for management of common conditions. Key words: Pharmacology; Pregnancy; Safety; Self-medication. Shutterstock 196 volume 44 | number 4 July/August 2019 Copyright © 2019 Wolters Kluwer Health, Inc. All rights reserved. he increased prevalence of pregnant women identifi ed risks in animal-reproduction studies or completed taking medications, including over-the-counter animal studies show no harm. The assignment of Category (OTC) medications presents a challenge to C has two indications; (1) limited or no research has been nurses providing care to women of childbear- conducted about use in pregnancy, and (2) animal studies ing age. -

A Guide to Obstetrical Coding Production of This Document Is Made Possible by Financial Contributions from Health Canada and Provincial and Territorial Governments
ICD-10-CA | CCI A Guide to Obstetrical Coding Production of this document is made possible by financial contributions from Health Canada and provincial and territorial governments. The views expressed herein do not necessarily represent the views of Health Canada or any provincial or territorial government. Unless otherwise indicated, this product uses data provided by Canada’s provinces and territories. All rights reserved. The contents of this publication may be reproduced unaltered, in whole or in part and by any means, solely for non-commercial purposes, provided that the Canadian Institute for Health Information is properly and fully acknowledged as the copyright owner. Any reproduction or use of this publication or its contents for any commercial purpose requires the prior written authorization of the Canadian Institute for Health Information. Reproduction or use that suggests endorsement by, or affiliation with, the Canadian Institute for Health Information is prohibited. For permission or information, please contact CIHI: Canadian Institute for Health Information 495 Richmond Road, Suite 600 Ottawa, Ontario K2A 4H6 Phone: 613-241-7860 Fax: 613-241-8120 www.cihi.ca [email protected] © 2018 Canadian Institute for Health Information Cette publication est aussi disponible en français sous le titre Guide de codification des données en obstétrique. Table of contents About CIHI ................................................................................................................................. 6 Chapter 1: Introduction .............................................................................................................. -

Turning Your Breech Baby to a Head-Down Position (External Cephalic Version)
Turning your breech baby to a head-down position (External Cephalic Version) This leaflet explains more about External Cephalic Version (ECV), including the benefits and risks. It will also describe any alternatives and what you can expect when you come to hospital. If you have any further questions, please speak to a doctor or midwife caring for you. What is a breech position? A breech position means that your baby is lying with its feet or bottom in your pelvis rather than in a head first position. This is common throughout most of pregnancy, but we expect that most babies will turn to lie head first by the end of pregnancy. If your baby is breech at 36 weeks of pregnancy it is unlikely that it will turn into a head down position on its own. Three in every 100 babies will still be in a breech position by 36 weeks. A breech baby may be lying in one of the following positions: Extended or frank Flexed breech – the Footling breech – the breech – the baby is baby is bottom first, with baby’s foot or feet are bottom first, with the thighs the thighs against the below the bottom. against the chest and feet chest and the knees bent. up by the ears. Most breech babies are in this position. Pictures reproduced with permission from ‘A breech baby at the end of pregnancy’ published by The Royal College of Obstetricians and Gynaecologists, 2008. 1 of 5 What causes breech? Breech is more common in women who are expecting twins, or in women who have a differently-shaped womb (uterus). -

Dermatology and Pregnancy* Dermatologia E Gestação*
RevistaN2V80.qxd 06.05.05 11:56 Page 179 179 Artigo de Revisão Dermatologia e gestação* Dermatology and pregnancy* Gilvan Ferreira Alves1 Lucas Souza Carmo Nogueira2 Tatiana Cristina Nogueira Varella3 Resumo: Neste estudo conduz-se uma revisão bibliográfica da literatura sobre dermatologia e gravidez abrangendo o período de 1962 a 2003. O banco de dados do Medline foi consul- tado com referência ao mesmo período. Não se incluiu a colestase intra-hepática da gravidez por não ser ela uma dermatose primária; contudo deve ser feito o diagnóstico diferencial entre suas manifestações na pele e as dermatoses específicas da gravidez. Este apanhado engloba as características clínicas e o prognóstico das alterações fisiológicas da pele durante a gravidez, as dermatoses influenciadas pela gravidez e as dermatoses específi- cas da gravidez. Ao final apresenta-se uma discussão sobre drogas e gravidez Palavras-chave: Dermatologia; Gravidez; Patologia. Abstract: This study is a literature review on dermatology and pregnancy from 1962 to 2003, based on Medline database search. Intrahepatic cholestasis of pregnancy was not included because it is not a primary dermatosis; however, its secondary skin lesions must be differentiated from specific dermatoses of pregnancy. This overview comprises clinical features and prognosis of the physiologic skin changes that occur during pregnancy; dermatoses influenced by pregnancy and the specific dermatoses of pregnancy. A discussion on drugs and pregnancy is presented at the end of this review. Keywords: Dermatology; Pregnancy; Pathology. GRAVIDEZ E PELE INTRODUÇÃO A gravidez representa um período de intensas ções do apetite, náuseas e vômitos, refluxo gastroeso- modificações para a mulher. Praticamente todos os fágico, constipação; e alterações imunológicas varia- sistemas do organismo são afetados, entre eles a pele. -

Vaginal Breech Birth Mary Olusile Lecturer in Practice
1 Vaginal Breech birth Mary Olusile Lecturer in Practice Breech: is where the fetal buttocks is the presenting part. Occurs in 15% of pregnancies at 28wks reducing to 3-4% at term Usually associated with: Uterine & pelvic anomalies - bicornuate uterus, lax uterus, fibroids and cysts Fetal anomalies - anencephaly, hydrocephaly, multiple gestation, oligohydraminous and polyhydraminous Cornually placed placenta (probably the commonest cause). Diagnosis: by abdominal examination or vaginal examination and confirmed by ultrasound scan Vaginal Breech VS. Caesarean Section Trial by Hannah et al (2001) found CS to produce better outcomes than vaginal breech but does acknowledge that may be due to lost skills of operators Therefore recommended mode of delivery is CS Limitations of trial by Hannah et al have since been highlighted questioning results and conclusion (Kotaska 2004) Now some advocates for vaginal breech birth when selection is based on clear prelabour and intrapartum criteria (Alarab et al 2004) Breech birth is u sually not an option except at clients choice Important considerations are size of fetus, presentation, attitude, size of maternal pelvis and parity of the woman NICE recommendation: External cephalic version (ECV) to be considered and offered if appropriate Produced by CETL 2007 2 Vaginal Breech birth Anterior posterior diameter of the pelvic brim is 11 cm Oblique diameter of the pelvic brim is 12 cm Transverse diameter of the pelvic brim is 13 cm Anterior posterior diameter of the outlet is 13 cm Produced by CETL 2007 3 -

Shoulder Dystocia Abnormal Placentation Umbilical Cord
Obstetric Emergencies Shoulder Dystocia Abnormal Placentation Umbilical Cord Prolapse Uterine Rupture TOLAC Diabetic Ketoacidosis Valerie Huwe, RNC-OB, MS, CNS & Meghan Duck RNC-OB, MS, CNS UCSF Benioff Children’s Hospital Outreach Services, Mission Bay Objectives .Highlight abnormal conditions that contribute to the severity of obstetric emergencies .Describe how nurses can implement recommended protocols, procedures, and guidelines during an OB emergency aimed to reduce patient harm .Identify safe-guards within hospital systems aimed to provide safe obstetric care .Identify triggers during childbirth that increase a women’s risk for Post Traumatic Stress Disorder and Postpartum Depression . Incorporate a multidisciplinary plan of care to optimize care for women with postpartum emergencies Obstetric Emergencies • Shoulder Dystocia • Abnormal Placentation • Umbilical Cord Prolapse • Uterine Rupture • TOLAC • Diabetic Ketoacidosis Risk-benefit analysis Balancing 2 Principles 1. Maternal ‒ Benefit should outweigh risk 2. Fetal ‒ Optimal outcome Case Presentation . 36 yo Hispanic woman G4 P3 to L&D for IOL .IVF Pregnancy .3 Prior vaginal births: 7.12, 8.1, 8.5 (NCB) .Late to care – EDC ~ 40-41 weeks .GDM Type A2 – somewhat uncontrolled .4’11’’ .Hx of Lupus .BMI 40 .Gained ~ 40 lbs during pregnancy Question: What complication is she a risk for? a) Placental abruption b) Thyroid Storm c) Preeclampsia with severe features d) Shoulder dystocia e) Uterine prolapse Case Presentation . 36 yo Hispanic woman G4 P3 to L&D for IOL .IVF Pregnancy .3 -

Single Stage Release Surgery for Congenital Constriction Band in a Clubfoot Patient Managed at a Teaching Hospital in Uganda: a Case Report G
Case report East African Orthopaedic Journal SINGLE STAGE RELEASE SURGERY FOR CONGENITAL CONSTRICTION BAND IN A CLUBFOOT PATIENT MANAGED AT A TEACHING HOSPITAL IN UGANDA: A CASE REPORT G. Waiswa, FCS, J. Nassaazi, MD and I. Kajja, PhD, Department of Orthopaedics, Makerere University, Kampala, Uganda Correspondence to: Dr. Judith Nassaazi, Department of Orthopaedics, Makerere University, Kampala, Uganda. Email: [email protected] ABSTRACT Congenital constriction band or amniotic band syndrome is a rare condition with a prevalence of 1:11200. It is characterized by presence of strictures around a body part, commonly around the distal part of the extremities. These bands can be treated with a single or staged approach. This study presents the case of a 3 month old infant who presented with a type III constriction band localized on the right leg and surgery was indicated. A single stage multiple Z-plasty was performed. The postoperative course was uneventful and the outcome was satisfactory at 10 months of follow-up. A single-stage constriction band release approach provided satisfactory results; both functional and aesthetic results and is feasible in our setting. Key words: Constriction bands, Single stage release, Stricture INTRODUCTION of worsening right leg deformity since birth (Figure 1). The mother reported that the child had been born Congenital constriction band or commonly referred to after a full-term pregnancy and normal delivery. This as amniotic band syndrome or Streeter dysplasia is a was the mother’s fifth child and there was no history rare condition characterized by congenital strictures of illness or drug use during pregnancy. No one else that can be partial or circumferential. -

OB/GYN – Childbirth/Labor/Delivery Protocol 6 - 2
Section SECTION: Obstetrical and Gynecological Emergencies REVISED: 06/2015 6 1. Physiologic Changes with Pregnancy Protocol 6 - 1 2. OB/GYN – Childbirth/Labor/Delivery Protocol 6 - 2 3. Medical – Newborn/Neonatal Protocol 6 - 3 OB / GYN Resuscitation 4. OB/GYN – Pregnancy Related Protocol 6 - 4 Emergencies (Delivery – Shoulder Dystocia) 5. OB/GYN – Pregnancy Related Protocol 6 - 5 Emergencies (Delivery – Breech Presentation) 6. OB/GYN – Pregnancy Related Protocol 6 - 6 Emergencies (Ectopic Pregnancy/Rupture) 7. OB/GYN – Pregnancy Related Protocol 6 - 7 EMERGENCIES Emergencies (Abruptio Placenta) 8. OB/GYN – Pregnancy Related Protocol 6 - 8 Emergencies (Placenta Previa) 9. OB/GYN – Pregnancy Related Protocol 6 - 9 Emergencies (Umbilical Cord Prolapse) 10. OB/GYN - Eclampsia Protocol 6 - 10 (Hypertension/Eclampsia/HELLPS) 11. OB/GYN – Pregnancy Related Protocol 6 - 11 Emergencies (Premature Rupture of Membranes (PROM)) 12. OB/GYN - Pre-term Labor Protocol 6 - 12 (Pre-term Labor) 13. OB/GYN – Post-partum Hemorrhage Protocol 6 - 13 Created, Developed, and Produced by the Old Dominion EMS Alliance Section 6 Continued This page intentionally left blank. OB / GYN EMERGENCIES Created, Developed, and Produced by the Old Dominion EMS Alliance Protocol SECTION: Obstetrical/Gynecological Emergencies PROTOCOL TITLE: Physiologic Changes with Pregnancy 6-1 REVISED: 06/2017 OVERVIEW: Many changes occur in the pregnant woman’s body, starting from the time of conception and throughout the pregnancy. The most obvious body system to undergo change is the reproductive system, but all of the others will change as well. Brief summaries of the physiologic changes that occur during pregnancy have been listed by system. Most of these physiologic changes will resolve during the postpartum period. -

Clinical Guideline Home Births
Clinical Guideline Guideline Number: CG038 Ver. 2 Home Births Disclaimer Clinical guidelines are developed and adopted to establish evidence-based clinical criteria for utilization management decisions. Oscar may delegate utilization management decisions of certain services to third-party delegates, who may develop and adopt their own clinical criteria. The clinical guidelines are applicable to all commercial plans. Services are subject to the terms, conditions, limitations of a member’s plan contracts, state laws, and federal laws. Please reference the member’s plan contracts (e.g., Certificate/Evidence of Coverage, Summary/Schedule of Benefits) or contact Oscar at 855-672-2755 to confirm coverage and benefit conditions. Summary Oscar members who chose to have a home birth may be eligible for coverage of provider services. An expectant mother has options as to where she may plan to give birth including at home, at a birthing center, or at a hospital. The American College of Obstetricians and Gynecologists (ACOG) believes that an at home birth is riskier than a birth at a birthing center or at a hospital, but ACOG respects the right of the woman to make this decision. A planned home birth is not appropriate for all pregnancies, and a screening should be done with an in-network provider to evaluate if a pregnancy is deemed low-risk and a home birth could be appropriate. Screening may include evaluating medical, obstetric, nutritional, environmental and psychosocial factors. Appropriate planning should also include arrangements for care at an in-network hospital should an emergent situation arise. Definitions “Certified Nurse-Midwife (CNM)” is a registered nurse who has completed education in a midwife program. -

Psycho-Socio-Cultural Risk Factors for Breech Presentation Caroline Peterson University of South Florida
University of South Florida Scholar Commons Graduate Theses and Dissertations Graduate School 7-2-2008 Psycho-Socio-Cultural Risk Factors for Breech Presentation Caroline Peterson University of South Florida Follow this and additional works at: https://scholarcommons.usf.edu/etd Part of the American Studies Commons Scholar Commons Citation Peterson, Caroline, "Psycho-Socio-Cultural Risk Factors for Breech Presentation" (2008). Graduate Theses and Dissertations. https://scholarcommons.usf.edu/etd/451 This Dissertation is brought to you for free and open access by the Graduate School at Scholar Commons. It has been accepted for inclusion in Graduate Theses and Dissertations by an authorized administrator of Scholar Commons. For more information, please contact [email protected]. Psycho-Socio-Cultural Risk Factors for Breech Presentation by Caroline Peterson A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy Department of Anthropology College of Arts and Science University of South Florida Major Professor: Lorena Madrigal, Ph.D. Wendy Nembhard, Ph.D. Nancy Romero-Daza, Ph.D. David Himmelgreen, Ph.D. Getchew Dagne, Ph.D. Date of Approval: July 2, 2008 Keywords: Maternal Fetal Attachment, Evolution, Developmental Plasticity, Logistic Regression, Personality © Copyright 2008, Caroline Peterson Dedication This dissertation is dedicated to all the moms who long for answers about their babys‟ presentation and to the babies who do their best to get here. Acknowledgments A big thank you to the following folks who made this dissertation possible: Jeffrey Roth who convinced ACHA to let me use their Medicaid data then linked it with the birth registry data. David Darr who persuaded the Florida DOH to let me use the birth registry data for free.