2019 Cascade County Community
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Before the Federal Communications Commission Washington, D.C
I BEFORE THE FEDERAL COMMUNICATIONS COMMISSION WASHINGTON, D.C. 20554 Petition of: Tobacco Valley Communication, Inc. To Exclude Eureka and the Remainder CSR- ______ of North Lincoln County from the Spokane, Washington DMA and Include it in the Missoula, Montana DMA PETITION FOR SPECIAL RELIEF January 31, 2014 Michael Strand STRAND LAW FIRM, PLLC P.O. Box 21117 Billings, MT 59101 (406) 465-5792 Attorney for Tobacco Valley Communications, Inc. TABLE OF CONTENTS Page I. Issues Presented 3 II. Brief Answers 3 Ill. Background 4 A. Tobacco Valley Communications, Eu reka and North Lincoln County 4 B. Spokane, Washington 4 c. Missoula, Montana 5 D. Kalispell, Montana 5 E. Distances 5 F. nme Zones 6 G. History of Station Carriage by Tobacco Valley 6 H. Retransmission Consent Agreements 7 IV. Governing Law 8 A. Legislative History 8 B. FederaJStatute 9 C. Prior FCC Decisions 10 V. Analysis 12 A. The Requested Modification is Consistent with Congressional Intent. 12 B. The Requested Modification is Consistent with Federal Statute. 13 VI. Standardized Evidence Approach 19 VII. Conclusion 20 VIII. List of Exhibits 22 2 Tobacco Valley Communications (hereafter "Tobacco Valley") hereby petitions the Federal Communications Commission (hereafter "FCC'') to exclude North Lincoln County, Montana, from the Spokane, Washington DMA and to include North lincoln County in the Missoula, Montana DMA. North Lincoln County, Montana, includes- but is not limited to-the communities of Eureka, Rexford, Trego, Fortine, West Kootenai and Stryker. For the purposes of administrative simplicity, Tobacco Valley recently successfully registered the entire Eureka/North Lincoln County area with the FCC as community unit MT0196 under the community name "Eureka." A copy of the registration is attached as Exhibit A. -

The Last Best Place
discover Montana Genuine The Last Best Place GREAT FALLS · MONTANA “the grandest sight I ever beheld...” 1805 · MERIWETHER LEWIS JOURNAL ENTRY Resting on the high plains along Montana’s Rocky Mountain Front Range, Great Falls is located at the confluence of the Missouri and Sun Rivers. This laid-back, hometown community offers delicious restaurants and a vibrant downtown full of unique shops and art galleries. Considered by many to be the birthplace of western art, Great Falls is home to the Charles M. Russell Museum, which houses works from this iconic western artist. The West’s largest Lewis and Clark museum also resides in Great Falls and documents their historic expedition and one of the most difficult legs of the journey, portaging the falls of the Missouri. Striking out from Great Falls in almost any direction will yield some of the most breathtaking venues in North America. With Glacier National Park, Waterton, Canada and the Bob Marshall Wilderness all a short distance away, Great Falls creates the ideal gateway for your Genuine Montana experience. GENUINEMONTANA.COM Black Eagle Falls © Great Falls Tribune · White Cliffs © BLM Glacier National Park Within an easy two-hour drive from Great Falls, hikers and sightseers can explore Glacier National Park. With the largest concentration of remaining glaciers in the lower 48 states, the park’s shining, glaciated peaks, plunging valleys and turquoise-blue lakes make it one of the most dramatic landscapes in North America. Glacier’s untamed vertical spires of banded granite and ice have earned it the nickname “Backbone of the World,” and these peaks are as wild as they are majestic. -

Construction Now Underway on New Benefis Emergency Department
ContributorSummer 2017 Construction Now Underway on New Benefis Emergency Department A groundbreaking ceremony was held on June 12, 2017, marking the official start of the construction for the new $12.5 million Benefis Emergency Department (ED). The size of the ED will be nearly doubled through both new construction and remodeling, and the innovative design will allow more efficient and patient-friendly care with shorter wait times. Construction for the new ED will take approximately 18 months to complete. Throughout that time, the ED will remain completely functional to meet the needs of our community. The Benefis Foundation committed to raising $2.5 million for this state-of-the art, patient- and family-focused center. To date, more than $2 million has been raised. Continued on page 2 “Our amazing donors are helping to ensure the future of world-class, life-saving emergency care for years to come.” Kevin Langkiet, Benefis Director of Emergency Services and Critical Care Benefis Health System Foundation The current Benefis ED was designed and built nearly two decades ago to care for only 24,000 patients annually. Today, the Benefis ED cares for more than 34,000 patients per year. As one of only four Level II trauma centers in Montana, “When you think about it, the Phase I Benefis Emergency Services Emergency Department probably Relocate helipad, is always ready to provide has more importance to our surrounding parking lots, life-saving care 24 hours community and region than a day, 365 days a year. remodel old cath lab almost any other service "On top of seeing patients way provided by Benefis.” Phase II over the intended capacity, the Benefis CEO John Goodnow Remodel old endoscopy complexity and acuity of the building, build new patients we’re seeing is rising ambulance parking as well," commented Benefis Emergency Services Director Dr. -

Inside Swinging Bridge Mrs
Belt Public School 4 May 2018 Issue 17 Inside Swinging Bridge Mrs. Ray/5th Grade Since the early 1900’s the in order for the community to entertain 2 Featured Staff “swinging” bridge has been a staple in the idea of a new forging a new path Belt’s on-foot transportation. Originally through Belt Creek. Calendar of Events nd 3 built in 1906, the footpath of the Just after midnight on April 22 , CMR Orchestra “swinging” bridge has been present the cables of Belt’s “swinging” bridge DECA IDCD 4 around the community in a variety of snapped under the stress of many people forms and locations. The first suspension jumping up and down, sending the quaint Spanish Class 5 bridge was built by the rodeo grounds little bridge to its demise in the bed of Gov. Debates near the park, but has Belt Creek. Ac- since been moved to cording to the Golf 6 the current location. city’s clerk- Mr. Paulson’s Trip The “swinging” treasurer Lynn May the Fourth Be bridge was originally Schilling, “Belt’s 7 With You constructed of two historic suspension cotton wood trees foot bridge was HS Track 8 and a series of large built strongly to stones. In 1908, a accommodate as Craig Cummings new bridge was con- many people as 9 Tournament structed for a cost of would fit on it end $375.00; the bridge was then replaced to end. Over the years various sports Music Festival about thirty years later, but the cost was teams and groups have been photographed Expanding Hori- 10 substantially steeper, totaling $4,000.00 on the bridge in numbers exceeding 25. -

GREAT FALLS INVESTMENT Offering Memorandum 117 NW Bypass - Great Falls Montana
GREAT FALLS INVESTMENT Offering Memorandum 117 NW Bypass - Great Falls Montana PRESENTED BY: Cameron Simonsen Brittany Ferris +1 801 453 6824 +1 801 453 6807 [email protected] [email protected] Lori Coburn Jane Ebberts +1 801 947 8352 +1 801 947 8326 [email protected] [email protected] MT LICENSE # RRE-BRO-LIC-71401 DISCLAIMER Return to TOC Disclaimer Colliers International (the “Agent”) has been engaged as the exclusive sales The Seller reserves the right, at its sole and absolute discretion, to withdraw the representative for the sale of the Buffalo Wild Wings located at 117 NW Bypass Property from the market for sale at any time and for any reason without notice, Road, Great Falls, Montana 59404 (the ”Property”) by DAPEG Investments Great to reject any and all expressions of interest or offers regarding the Property, and/ Falls LLC or ‘Ownership’ (the “Seller”). or to terminate discussions with any entity at any time, with or without notice. This Offering Memorandum is made subject to omissions, correction of errors, The Property is being offered for sale in an “as-is, where-is” condition, and the change of price or other terms, prior sale or withdrawal from the market without Seller and the Agent make no representations or warranties as to the accuracy of notice. The Agent is not authorized to make any representations or agreements the information contained in this Offering Memorandum. The enclosed materials on behalf of the Seller. The Seller shall have no legal commitment or obligation to include confidential information and are being furnished solely for the purpose of any recipient reviewing the enclosed materials, performing additional investigation, review by prospective purchasers (“Purchasers”) of the interest described herein and/or making an offer to purchase the Property unless and until a binding written for which it shall be fully and solely responsible. -
Highwood Mountains Range Analysis Project Area on Those Resources Affected by Implementation
United States Department of Agriculture Environmental Forest Service Assessment 2015 Highwood Mountains Range Judith Ranger District, Lewis and Clark National Forest Cascade, Choteau and Judith Basin Counties, Montana For More Information Contact: Lewis and Clark National Forest Judith Ranger District Standford, Montana www.fs.fed.us/r1/lewisclark/projects 406-566-2292. The U.S. Department of Agriculture (USDA) prohibits discrimination in all its programs and activities on the basis of race, color, national origin, age, disability, and where applicable, sex, marital status, familial status, parental status, religion, sexual orientation, genetic information, political beliefs, reprisal, or because all or part of an individual’s income is derived from any public assistance program. (Not all prohibited bases apply to all programs.) Persons with disabilities who require alternative means for communication of program information (Braille, large print, audiotape, etc.) should contact USDA’s TARGET Center at (202) 720-2600 (voice and TTY). To file a complaint of discrimination, write to USDA, Director, Office of Civil Rights, 1400 Independence Avenue, SW., Washington, DC 20250-9410, or call (800) 795-3272 (voice) or (202) 720-6382 (TTY). USDA is an equal opportunity provider and employer. Environmental Assessment Table of Contents Introduction ...................................................................................................................................................4 Location of the Proposed Project Area ..........................................................................................................4 -
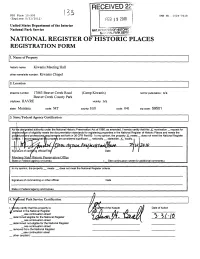
National Register of Historic Places Registration Form
NFS Form 10-900 0MB No. 1024-0018 (Expires 5/31/2012) FEB 1 9 2010 United States Department of the Interior National Park Service NAT. RreWTEFi OF HISTORIC '• NAPONALPARKSEFWI NATIONAL REGISTER OF HISTORIC PLACES REGISTRATION FORM 1. Name of Property historic name: Kiwanis Meeting Hall other name/site number: Kiwanis Chapel 2. Location street & number: 17863 Beaver Creek Road (Camp Kiwanis) not for publication: n/a Beaver Creek County Park city/town: HAVRE vicinity: n/a state: Montana code: MT county: Hill code: 041 zip code: 59501 3. State/Federal Agency Certification As tr|e designated authority under the National Historic Preservation Act of 1986, as amended, I hereby certify t that this X nomination _ request for deti jrminalon of eligibility meets the documentation standards for registering properties in the National Regist er of Historic Places and meets the pro i^duraland professional/equiremants set forth in 36 CFR Part 60. In my opinion, the property X meets _ _ does not meet the National Register Crlt jfria. I JecommendJhat tnis propeay be considered significant _ nationally _ statewide X locally, i 20 W V» 1 ' Signature of certifj^ng official/Title/ Date / Montana State Historic Preservation Office State or Federal agency or bureau ( See continuation sheet for additional comments.) In my opinion, the property _ meets _ does not meet the National Register criteria. Signature of commenting or other official Date State or Federal agency and bureau 4. National Park Service Certification I, hereby certify that this property is: Date of Action entered in the National Register _ see continuation sheet _ determined eligible for the National Register *>(.> 10 _ see continuation sheet _ determined not eligible for the National Register _ see continuation sheet _ removed from the National Register _see continuation sheet _ other (explain): _________________ Kiwanis Meeting Hall Hill County. -

2021 Talent Attraction Plan Approved 2/4/21
2021 Talent Attraction Plan Approved 2/4/21 As we enter the second year of the Live in Great Falls initiative, we are excited to expand upon the tools and services we created in response to recruiter feedback in 2020. Based on research and the suggestions of our talent attraction marketing consultants, this is an outline of our plan for coming year. 1) Get more employers to use existing tools • Continue outreach to engage more employers with goal of 70% investor participation by end of year. • Host trainings for employers and real estate professionals on using Live In Great Falls tools for talent attraction. • Publish regular newsletter for employers and recruiters. • Publish HR webpage on Live in Great Falls website, directing users to GFDA website where all employer/recruiter materials will be located. • Create Talent Attraction Advisory Committee to engage more private sector employers. 2) Develop more tools • Partner with Great Falls Montana Tourism to create Bandwango Self-Tours for visiting job candidates and recent relocatees. • Release three professional Talent Attraction videos. • Create video series as a virtual tour experience for use on Live in Great Falls website, employer career pages, and social media accounts. • Publish and widely promote Version 2.0 of Live In Great Falls website. • Publish 2021 Great Falls Livability magazine and increase presence on Livability.com website and blog. • Enhance Great Falls Wikipedia page. 3) Market living and working in Great Falls, Montana • Implement DCI Marketing Strategy with Ask an Expert videos, social media, content placing, earned media, and targeted content for remote workers. • Secure kiosk placement for Live in Great Falls signs and rack cards at partner locations around town. -

Montana: the Last, Best Place?
CHAPTER 2 Montana: The Last, Best Place? o understand politics in Montana and the process of representation, one T does not begin with people or politicians. One begins with place, because without place the rest does not—cannot—be made to make sense. How Montanans understand themselves, their representatives, their history, and their relationship to others—including the federal government—begins and ends with place. It is also place that presents Montanans with their greatest challenges and opportuni- ties. To use Richard Fenno’s terminology, we must begin with the geographic constituency—not only as a physical space and place, but as a shared idea and experience. To understand Montana and Montanans, we must start with the land known variously as the Treasure State, Big Sky Country,distribute or perhaps the most evocative: The Last, Best Place. In this chapter, I provide the reader with a short historyor of Montana’s relation- ship to the land, its historical development, the complicated relationship it has with the federal government, and the challenges the state faces as it transitions from a resource-intensive economy to a more diverse one based upon tourism and hi-tech industries. I claim that the deep connection Montanans have with their physical surroundings shapes howpost, they view politics, the cleavages which exist among them, and the representatives they choose to represent them. Place also dictates the representational choices members of Congress make to build trust with their constituents. In particular, members of Congress are careful to cultivate a representational style known as “one of us” with their constituents. -

FTC Staff Comment to Texas Health and Human Services Commission
UNITED STATES OF AMERICA Federal Trade Commission WASHINGTON, D.C. 20580 Bureau of Competition Bureau of Economics Office of Policy Planning September 11, 2020 VIA ELECTRONIC MAIL Texas Health and Human Services Commission c/o Phil Wilson, Executive Commissioner Brown-Heatly Building 4900 North Lamar Blvd. Austin, TX 76711-3247 Public Comment Inbox: [email protected] Re: Certificate of Public Advantage Applications of Hendrick Health System and Shannon Health System Dear Executive Commissioner Wilson: On behalf of the staffs of the FTC’s Bureau of Competition, Bureau of Economics, and Office of Policy Planning, and pursuant to Texas Health and Safety Code § 314A.001 et seq., we are providing the attached public comment that presents our views on the respective Applications for Certificate of Public Advantage submitted by Hendrick Health System and Shannon Health System. We can provide copies of any documents referenced in this comment upon request. Please direct questions concerning this submission to Melissa Hill, Deputy Assistant Director of the Mergers IV Division, Bureau of Competition, 202-326-2673, [email protected]; and Stephanie Wilkinson, Attorney Advisor, Office of Policy Planning, 202-326-2084, [email protected]. Respectfully submitted, Ian Conner, Director Bureau of Competition Digitally signed by ANDREW ANDREW SWEETING Date: 2020.09.11 13:44:10 SWEETING -04'00' Andrew Sweeting, Director Bureau of Economics Digitally signed by BILAL SAYYED BILAL SAYYED Date: 2020.09.11 13:40:47 -04'00' Bilal Sayyed, Director Office of Policy Planning cc: W. Kenneth Paxton, Jr., Attorney General of the State of Texas Federal Trade Commission Staff Submission to Texas Health and Human Services Commission Regarding the Certificate of Public Advantage Applications of Hendrick Health System and Shannon Health System Pursuant to Texas Health and Safety Code § 314A.001 et seq. -

Grow Tourism
Boards of Directors Meeting Minutes Great Falls Convention and Visitors Bureau & Great Falls Tourism Business Improvement District Thursday, May 21, 2020 | 9:00 AM – 9:43 AM | https://us02web.zoom.us/j/5456501810 CVB Board: Wayne Thares, Susan Shannon, Scott Lettre, Kaylene Kershner, Brett Doney, Steve Herrig, Kerry McInerney, Karen Venetz, Wendy Lee, Teresa Appelwick, John Faulkner, Kellie Pierce, Brian Thompson, Peggy O’Hare-Becker TBID Board: Sandra Johnson-Thares, Becky Amaral-Miller, Scott Shull, David Buckingham, Peggy O’Haire-Becker, Laurie Price Staff: Rebecca Engum, Kristin Dayao, Marisela Hazzard 9:00 | 1. Welcome, Call to Order, Introductions – Kaylene Kershner, Sandra Thares 9:01 | 2. Public Comment – Kaylene Kershner, Sandra Thares Opportunity for public comment related to items on the agenda No public comment. 9:02 | 3. Consent Agenda – Kaylene Kershner, Sandra Thares Convention and Visitors Bureau Board of Directors a) approve 4-16-2020 Minutes b) approve 4-23-2020 Minutes c) approve 5-7-2020 Minutes d) accept April Financials CVB ACTION TAKEN Motion made to approve consent agenda. Seconded. No discussion. All in favor. None Opposed. The motion passed. Tourism Business Improvement District Board of Directors e) approve 2-20-2020 Minutes f) approve 4-23-2020 Minutes g) accept April Financials TBID ACTION TAKEN Motion made to approve consent agenda. Seconded. No discussion. All in favor. None Opposed. The motion passed. 9:08 | 4. CVB Nomination Slate – Brian Thompson Slate presented to include Scott Lettre with Great Falls Voyagers, Wayne Thares with Taco Johns, Christina Horton with C.M. Russell Museum, and Lexi Jones with The Do Bar. -

Description of the Fort Benton Quadrangle
DESCRIPTION OF THE FORT BENTON QUADRANGLE. INTRODUCTION. steeply inclined sides. In the center of the range of the throat of a volcano, the dikes which radiate heat and cold, varying greatly, of course, with the the limestones and other stratified rocks are hori from these centers of activity, and the loose mate altitude. The annual rainfall is from 13 to 20 General relations. The Fort Benton quad zontal, or nearly so, while on the flanks structure of rials and lava flows of which the cones Structure_. , of. inches, being greatest in the mountains; June and rangle extends in longitude from 110° to 111° of the mountains they are sharply BheuLMoun- were built. The sedimentary strata October are the rainy months. The snowfall is and in latitude from 47° to 48°. It is inclined and dip away from the moun through which the volcanoes broke up heavy and the mountain tracts are well watered. 69.25 miles Ions; from north to south. extent°ofan tains to the lower plains country. The horizontal and upon which their materials accumulated are, Agriculture is therefore confined to the foothills . quadrangle. 47.36 miles wide, and contains 3272.7 attitude is well shown in the rocks of Belt Park, over most of the area, nearly horizontal or inclined and stream bottoms, except where irrigation is square miles. It includes part of Choteau, the whereas farther north the mountain masses near gently to the north. These rocks belong entirely possible. northwest corner of Fergus, and the eastern part Monarch are formed of blocks of tilted limestones to the Cretaceous system, and denudation has Culture.