Toxicological Profile for Toluene Diisocyanate and Methylenediphenyl Diisocyanate
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Synthesis and Characterization of Toluene Diisocyanate
SYNTHESIS AND CHARACTERIZATION OF TOLUENE DIISOCYANATE A THESIS SUBMITTED TO THE GRADUATE SCHOOL OF NATURAL AND APPLIED SCIENCES OF MIDDLE EAST TECHNICAL UNIVERSITY BY AYŞEGÜL HİSAR TELLİ IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE IN CHEMISTRY NOVEMBER 2014 Approval of the thesis: SYNTHESIS AND CHARACTERIZATION OF TOLUENE DIISOCYANATE submitted by AYŞEGÜL HİSAR TELLİ in partial fulfillment of the requirements for the degree of Master of Science in Chemistry Department, Middle East Technical University by, Prof. Dr. Gülbin Dural Ünver _____________________ Dean, Graduate School of Natural and Applied Sciences Prof. Dr. İlker Özkan _____________________ Head of Department, Chemistry Prof. Dr. Özdemir Doğan _____________________ Supervisor, Chemistry Dept., METU Examining Committee Members: Prof. Dr. Cihangir Tanyeli _____________________ Chemistry Dept., METU Prof. Dr. Özdemir Doğan _____________________ Chemistry Dept., METU Prof. Dr. Metin Zora _____________________ Chemistry Dept., METU Prof. Dr. Adnan Bulut _____________________ Chemistry Dept., Kırıkkale University Dr. E. Görkem Günbaş _____________________ Chemistry Dept., METU Date: 28.11.2014 I hereby declare that all information in this document has been obtained and presented in accordance with academic rules and ethical conduct. I also declare that, as required by these rules and conduct, I have fully cited and referenced all material and results that are not original to this work. Name, Last name: Ayşegül Hisar Telli Signature: iv ABSTRACT SYNTHESIS AND CHARACTERIZATION OF TOLUENE DIISOCYANATE Hisar Telli, Ayşegül M.S., Department of Chemistry Supervisor: Prof. Dr. Özdemir Doğan November 2014, 52 pages Toluene diisocyanate (TDI) is one of the important components of solid rocket propellants. It is used for the construction of polyurethane network by reacting with hydroxy terminated polybutadiene (HTPB) and functions as a curing agent. -

Risk Assessment Report
R064_0805_env_hh 28.05.2008 European Union Risk Assessment Report 4-METHYL-M-PHENYLENEDIAMINE (TOLUENE-2,4-DIAMINE) RISK ASSESSMENT CAS-No.: 95-80-7 EINECS-No.: 202-453-1 28.05.2008 FINAL APPROVED VERSION 1 CAS No 95-80-7 R064_0805_env_hh 28.05.2008 Information on the rapporteur Contact point: Bundesanstalt für Arbeitsschutz und Arbeitsmedizin Anmeldestelle Chemikaliengesetz Friedrich-Henkel-Weg 1-25 44149 Dortmund e-mail: [email protected] This document is the last version of the Comprehensive Risk Assessment Report Toluene- 2,4-diamine, a substance chosen from the EU 1st Priority List in 1994. 2 CAS No 95-80-7 R064_0805_env_hh 28.05.2008 LEGAL NOTICE Neither the European Commission nor any person acting on behalf of the Commission is responsible for the use which might be made of the following information A great deal of additional information on the European Union is available on the Internet. It can be accessed through the Europa Server (http://europa.eu.int). Cataloguing data can be found at the end of this publication Luxembourg: Office for Official Publications of the European Communities, [ECB: year] ISBN [ECB: insert number here] © European Communities, [ECB: insert year here] Reproduction is authorised provided the source is acknowledged. Printed in Italy 3 CAS No 95-80-7 R064_0805_env_hh 28.05.2008 Foreword We are pleased to present this Risk Assessment Report which is the result of in-depth work carried out by experts in one Member State, working in co-operation with their counterparts in the other Member States, the Commission Services, Industry and public interest groups. -

MDI and TDI: Safety, Health and the Environment
MDI and TDI: Safety, Health and the Environment. A Source Book and Practical Guide Edited by: DCAllport Gilbert International Ltd, Manchester, UK D S Gilbert Gilbert International Ltd, Manchester, UK and S M Outterside Gilbert International Ltd, Manchester, UK Copyright 2003 John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex PO19 8SQ, England Telephone (+44) 1243 779777 Email (for orders and customer service enquiries): [email protected] Visit our Home Page on www.wileyeurope.com or www.wiley.com All Rights Reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, scanning or otherwise, except under the terms of the Copyright, Designs and Patents Act 1988 or under the terms of a licence issued by the Copyright Licensing Agency Ltd, 90 Tottenham Court Road, London W1T 4LP, UK, without the permission in writing of the Publisher. Requests to the Publisher should be addressed to the Permissions Department, John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex PO19 8SQ, England, or emailed to [email protected], or faxed to (+44) 1243 770620. This publication is designed to provide accurate and authoritative information in regard to the subject matter covered. It is sold on the understanding that the Publisher is not engaged in rendering professional services. If professional advice or other expert assistance is required, the services of a competent professional should be sought. Other Wiley Editorial Offices John Wiley & Sons Inc., 111 River Street, Hoboken, NJ 07030, USA Jossey-Bass, 989 Market Street, San Francisco, CA 94103-1741, USA Wiley-VCH Verlag GmbH, Boschstr. -
MDI and TDI: Safety, Health and the Environment
MDI and TDI: Safety, Health and the Environment. A Source Book and Practical Guide Edited by: DCAllport Gilbert International Ltd, Manchester, UK D S Gilbert Gilbert International Ltd, Manchester, UK and S M Outterside Gilbert International Ltd, Manchester, UK Copyright 2003 John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex PO19 8SQ, England Telephone (+44) 1243 779777 Email (for orders and customer service enquiries): [email protected] Visit our Home Page on www.wileyeurope.com or www.wiley.com All Rights Reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, scanning or otherwise, except under the terms of the Copyright, Designs and Patents Act 1988 or under the terms of a licence issued by the Copyright Licensing Agency Ltd, 90 Tottenham Court Road, London W1T 4LP, UK, without the permission in writing of the Publisher. Requests to the Publisher should be addressed to the Permissions Department, John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex PO19 8SQ, England, or emailed to [email protected], or faxed to (+44) 1243 770620. This publication is designed to provide accurate and authoritative information in regard to the subject matter covered. It is sold on the understanding that the Publisher is not engaged in rendering professional services. If professional advice or other expert assistance is required, the services of a competent professional should be sought. Other Wiley Editorial Offices John Wiley & Sons Inc., 111 River Street, Hoboken, NJ 07030, USA Jossey-Bass, 989 Market Street, San Francisco, CA 94103-1741, USA Wiley-VCH Verlag GmbH, Boschstr. -

Review of the Occupational Exposure to Isocyanates: Mechanisms of Action
[Environmental Health and Preventive Medicine 7, 1–6, April 2002] Review Article Review of the Occupational Exposure to Isocyanates: Mechanisms of Action Kazuko NAKASHIMA, Tatsuya TAKESHITA and Kanehisa MORIMOTO Department of Social and Environmental Medicine, Course of Social Medicine, Osaka University Graduate School of Medicine, Osaka Abstract Polyurethanes are useful polymers in a large variety of technical and consumer products that are generally made from diisocyanates and polyols or similar compounds. Toluene diisocyanate (TDI), 4,4’- methylenediphenyl diisocyanate (MDI) and 1,6’-hexamethylene diisocyanate (HDI) are useful for polyure- thane products. Isocyanates are reactive chemicals that can be handled without problems in manufacturing or technical environments. In general, consumers may only have contact with these chemicals on rare occa- sions. The objective of this study was to review the mechanisms of action of inhalation of isocyanates. This paper describes, in summary, the potential occupational exposure to isocyanates, the chemistry and reactivity of isocyanates, the results from genotoxicity studies, investigative toxicity studies, metabolism and results from epidemiology studies on isocyanate-exposed workers. The overall conclusion is that because humans are not exposed to high levels of respiratory isocyanate particles, concerns over the possible development of lung tumors should not be relevant. There are many mechanisms of action induced by isocyanates, but those entities are unclear. This is because these mechanisms act simultaneously and are complex. Key words: diisocyanate, immunology, genotoxicity, carcinogenicity, review Introduction where chemicals induce occupational symptoms that produce new problems after their sensitization. These problems need to be iden- Polyurethanes are useful polymers in a large variety of tech- tified. -

And 2,6-Toluenediamine in Hydrolysed Urine and Plasma After Occupational Exposure to 2,4- and 2,6- Toluene Diisocyanate 95
94 Occupational and Environmental Medicine 1996;53:94-99 Toxicokinetics of 2,4- and 2,6-toluenediamine in Occup Environ Med: first published as 10.1136/oem.53.2.94 on 1 February 1996. Downloaded from hydrolysed urine and plasma after occupational exposure to 2,4- and 2,6- toluene diisocyanate Pernilla Lind, Marianne Dalene, Gunnar Skarping, Lars Hagmar Abstract Keywords: toluenediisocyanate; biomarkers; toxicoki- Objectives-To assess the toxicokinetics netics; gas chromatography-mass spectrometry of 2,4- and 2,6- toluenediisocyanate (TDI) in chronically exposed subjects. Toluenediisocyanate (TDI) is an important Methods-Blood and urine, from 11 industrial chemical, used in the production of workers at two flexible foam polyurethane polyurethane (PUR) polymers. Commercially production plants, were sampled. By used TDI contains both the 2,4- and 2,6-TDI gas chromatography-mass spectrometry isomers in 80:20 or 65:35 ratios. (GC-MS) 2,4- and 2,6-toluene diamine In high concentrations TDI may cause irri- (TDA) were measured as pentafluoropro- tation of the mucous membranes, have sensi- pionic anhydride (PFPA) derivatives tising properties, and may also cause asthma after acidic hydrolysis ofplasma (P-TDA, and possibly a progressive impairment of pul- ng/ml) and urine (U-TDA, ug/h). monary function.'- Moreover, TDI is carcino- Results-In one of the plants the P-2,4- genic to animals4 but occupational exposure in TDA concentrations were 0*4-1 ng/ml polyurethane foam manufacturing has, to before a four to five week holiday and date, not been associated with an increased 0-2-05 ng/ml afterwards. The corre- risk of cancer.5-7 sponding values for P-2,6-TDA were 2-6 The Swedish occupational exposure limit and 05-2 ng/ml respectively. -

Comparative Study of Aromatic and Cycloaliphatic Isocyanate Effects On
polymers Article Comparative Study of Aromatic and Cycloaliphatic Isocyanate Effects on Physico-Chemical Properties of Bio-Based Polyurethane Acrylate Coatings Nurul Huda Mudri 1,2,*, Luqman Chuah Abdullah 1,3,* , Min Min Aung 3,4 , Mek Zah Salleh 2, Dayang Radiah Awang Biak 1,5 and Marwah Rayung 3,6 1 Department of Chemical and Environmental Engineering, Faculty of Engineering, Universiti Putra Malaysia, Serdang 43400, Selangor, Malaysia; [email protected] 2 Radiation Processing Technology Division, Malaysian Nuclear Agency, Kajang 43000, Selangor, Malaysia; [email protected] 3 Institute of Tropical Forestry and Forest Products (INTROP), Universiti Putra Malaysia, Serdang 43400, Selangor, Malaysia; [email protected] (M.M.A.); [email protected] (M.R.) 4 Centre of Foundation Studies for Agricultural Science, Universiti Putra Malaysia, Serdang 43400, Selangor, Malaysia 5 Institute of Advanced Technology, Universiti Putra Malaysia, Serdang 43000, Selangor, Malaysia 6 Department of Chemistry, Faculty of Science and Technology, Universiti Putra Malaysia, Serdang 43400, Selangor, Malaysia * Correspondence: [email protected] (N.H.M); [email protected] (L.C.A.); Tel.: +60-3-8946-6288 (L.C.A.) Received: 15 May 2020; Accepted: 4 June 2020; Published: 3 July 2020 Abstract: Crude jatropha oil (JO) was modified to form jatropha oil-based polyol (JOL) via two steps in a chemical reaction known as epoxidation and hydroxylation. JOL was then reacted with isocyanates to produce JO-based polyurethane resin. In this study, two types of isocyanates, 2,4-toluene diisocyanate (2,4-TDI) and isophorone diisocyanate (IPDI) were introduced to produce JPUA-TDI and JPUA-IPDI respectively. -
Polyurethane Coating Composition
turopaisches Patentamt (19) European Patent Office © Publication number: 0 263 298 Office europeen des brevets A1 © EUROPEAN PATENT APPLICATION © Application number: 87112643.9 © C08G 18/12 Int. CI.": , C08G 18/66 , C08G - 18/72 , C09D 3/72 © Date of filing: 29.08.87 ® Priority: 08.09.86 US 904732 © Applicant: W.R. GRACE & CO. Grace Plaza 1114 Avenue of the Americas © Date of publication of application: New York New York 10036(US) 13.04.88 Bulletin 88/15 © Inventor: Vu, Cung © Designated Contracting States: 18805 Still Meadows Court AT BE CH DE ES FR GB GR IT LI LU NL SE Gaithersburg Maryland 20879(US) © Representative: UEXKULL & STOLBERG Patentanwalte Beselerstrasse 4 D-2000 Hamburg 52(DE) Polyurethane coating composition. This invention relates to a moisture curable, isocyanate terminated, branched prepolymer which is the reaction product of (a) an alcohol having two or three -OH groups, (b) a hydrophobic polymeric diol or triol and (c) at least one polyisocyanate, said prepolymer having an NCO content in the range 0.3 to 1 .0 meq/g. Exposure Df the prepolymer as a coating on a substrate to moisture under atmospheric conditions results in a cured soating having excellent adhesion to the substrate and excellent abrasion resistance. 30 3) N y) £> N D a. jj «rax Copy Centre 0 263 298 POLYURETHANE COATING COMPOSITION BACKGROUND OF THE INVENTION This invention relates to a process for forming a crosslinked polyurethane. More particularly, this 5 invention relates to a crosslinked, polyurethane of 100% solids content which can be formulated into products usable in the coatings field. -

Technical Fact Sheet- Dinitrotoluene (DNT)
Technical Fact Sheet Dinitrotoluene (DNT) February 2017 This fact sheet, developed by the U.S. Environmental Protection Agency (EPA) Federal Facilities Restoration and Reuse Office (FFRRO), provides a summary of dinitrotoluene (DNT), including physical and chemical properties; environmental and health impacts; existing federal and state guidelines; detection and treatment methods; and additional sources of information. This fact sheet is intended for use by site managers and field personnel who may address DNT contamination at cleanup sites or in drinking water supplies. The widespread use of DNT in manufacturing munitions, polyurethane foams, and other chemical products has contributed to extensive soil and groundwater contamination. DNT can be transported in surface water or groundwater because of its moderate solubility and relatively low volatility, unless degraded by light, oxygen or biota. As a result, releases to water are important sources of human exposure and remain a significant environmental concern. DNT is considered toxic to most organisms, and chronic exposure may result in organ damage. EPA currently classifies DNT as a priority pollutant. _ DNT is a nitroaromatic explosive that exists as six isomers: 2,4- and 2,6- DNT are the two major forms; 2,3-DNT, 2,5-DNT, 3,4-DNT and 3,5-DNT are minor isomers (ATSDR 2016; Lent and others 2012a). _ Technical grade DNT (Tg-DNT) is about 76.5% 2,4-DNT, 18.8% 2,6-DNT, and 4.7% minor isomers (2.43% 3,4-DNT, 1.54% 2,3-DNT, 0.69% 2,5- DNT, and 0.04% 3,5-DNT (ATSDR 2016; Lent and others 2012a). -
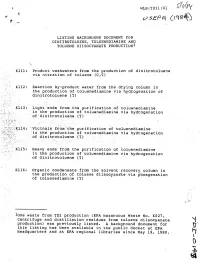
This Listing Has Been Available in the Public Docket at EPA L^ Headquarters and at EPA Regional Libraries Since May 19, 1980
*• WLB:TDI1:01 iffy LISTING BACKGROUND DOCUMENT FOR DINITROTOLUENE, TOLUENEDIAMINE AND TOLUENE DIISOCYANATE PRODUCTION1 Kill: Product washwaters from the production of dinitrotoluene via nitration of toluene (C,T) K112: Reaction by-product water from the drying column in the production of toluenediamine via hydrogenation of dinitrotoluene (T) K113:. Light ends from the purification of toluenediamine in the production of toluenediamine via hydrogenation . .'. of dinitrotoluene (T) -. ..K114V Vicinals from the purification of toluenediamine l'__ , ; in the production of toluenediamine via hydrogenation \ ' of dinitrotoluene (T.) : K115: Heavy ends from the purification of toluenediamine in the production of toluenediamine via hydrogenation of dinitrotoluene (T) K116: Organic condensate from the solvent recovery column in the production of toluene diisocyanate via phosgenation of toluenediamine (T) *One waste from TDI production (EPA Hazardous Waste No. K027, Centrifuge and distillation residues from toluene diisocyanate "i production) was previously listed. A background document for Vl' this listing has been available in the public docket at EPA L^ Headquarters and at EPA regional libraries since May 19, 1980. H v- 4 \ t TABLE OF CONTENTS PAGE I. Summary of Basis for Listing 1 II. Sources of the Wastes 2 A. Profile of the Industry 2 B. Manufacturing Processes 4 1. Nitration of toluene to form dinitrotoluene (DNT) 5 2. Hydrogenation of DNT to form toluenediamine (TDA) 3 3. Formation of toluene diisocyanate (TDI) from TDA 12 III. Composition of the Wastes 16 IV. Waste Management 22 V. Basis for Listing 27 A. Hazards Posed by the Wastes 27 B. Degree of Hazards Posed by These Wastes 34 C. -

2,4-Diaminotoluene C7H10N2
CAS 95-80-7 2,4-Diaminotoluene C7H10N2 Summary of Health Effects 2,4-diaminotoluene causes cancer in animals The European Commission Joint Research and may cause cancer in humans. Centre determined 2,4-diaminotoluene to be toxic to genetic material.5 How is 2,4-diaminotoluene used? 2,4-diaminotoluene is used to make other Exposure: How can a person come in chemical ingredients used in polyurethane, contact with it? paints, varnishes, adhesives and foams.1 A person can come in contact with 2,4- diaminotoluene by breathing in contaminated air, eating and drinking contaminated food and Toxicity: What are its health effects? water, or from skin contact with consumer The EPA classified 2,4-diaminotoluene as a products.2 probable human carcinogen.1 The National Toxicology Program has stated that 2,4- 2,4-Diaminotoluene is used in the production of diaminotoluene is reasonably anticipated to be toluene diisocyanate, which is used to make a human carcinogen.2 The International Agency polyurethane, a synthetic resin used in paints, for Research on Cancer has concluded that 2,4- varnishes, adhesives, and foams.1 diaminotoluene is possibly carcinogenic to humans due to liver and mammary gland The 2014 Nation Health and Nutrition tumors in rats and mice.3 2,4-diaminotoluene is Examination Survey (NHANES) report did not included on California’s Proposition 65 list as a include data for 2,4-diaminotoluene. carcinogen.4 References 1. U.S. Environmental Protection Agency, Technology Transfer Network (2000). Hazard summary for toluene-2,4- diamine. Retrieved from www.epa.gov/sites/production/files/2016-09/documents/toluene-2-4-diamine.pdf 2. -

P-TMXDI Polyurethane Elastomers with Good Compression Set Properties
~" ' MM II II II Ml I Ml II I II Ml II I II J European Patent Office CO Publication number: 0 171 536 B1 Office europeen„ des brevets © EUROPEAN PATENT SPECIFICATION © Date of publication of patent specification: 12.02.92 © Int. CI.5: C08G 18/10, C08G 18/76 © Application number: 85107091.2 @ Date of filing: 08.06.85 The file contains technical information submitted after the application was filed and not included in this specification © P-TMXDI polyurethane elastomers with good compression set properties. © Priority: 30.07.84 US 634081 Proprietor: AMERICAN CYANAMID COMPANY 1937 West Main Street P.O. Box 60 @ Date of publication of application: Stamford Connecticut 06904-0060(US) 19.02.86 Bulletin 86/08 Inventor: Chang, Eugene Yue Chieh © Publication of the grant of the patent: 532 Rolling Hills Road 12.02.92 Bulletin 92/07 Bridgewater New Jersey 08807(US) © Designated Contracting States: AT BE CH DE FR GB IT LI NL SE Representative: Wachtershauser, Gunter, Dr. Tal 29 © References cited: W-8000 Munchen 2(DE) EP-A- 0 022 497 EP-A- 0 111 694 DE-A- 1 645 147 US-A- 3 428 610 US-A- 4 218 543 JOURNAL OF CELLULAR PLASTICS, vol. 18, no. 6, November - December 1982, pages 376-383, Westport, Connecticut, US; V.D. AR- ENDT et al. "M- and P-TMXDI: two new isocyanates for the polyurethane industry" 00 CO CO m Note: Within nine months from the publication of the mention of the grant of the European patent, any person may give notice to the European Patent Office of opposition to the European patent granted.