BMI the Beardwood Hospital Newapproachcomprehensive Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Newsletter 17.5.21
Newsletter 17.5.21 EID We hope that everyone who celebrated Eid has had a lovely day. The children enjoyed celebrating Eid in school on Friday. Covid You will be aware that there has been a rise in Covid cases in the area. This rise is linked, in part, to a new Indian variant that spreads more easily. As well as getting tested if you have symptoms, it is also vital that everyone in Blackburn with Darwen continues to follow the guidelines and the ‘Hands, Face, Space, Fresh Air’ rules – as this is the most effective way to control the spread of all variants of coronavirus. A number of cases of the Covid-19 variant first identified in India have been detected across the North West. It has now been classified as a ‘Variant of Concern’, however there is currently no evidence that it causes more severe illness, is more deadly or makes the current vaccines any less effective. Public Health England is currently working to understand this variant better. The advice to everyone in Blackburn with Darwen is to be cautious of this rise in cases locally, and continue to follow the government guidance. People living in Blackburn with Darwen, are strongly encouraged to continue using free rapid testing twice weekly to keep themselves and their loved ones safe. There are plenty of places to get a test in Blackburn with Darwen, whether you have symptoms or no symptoms. Go here for more information: https://www.blackburn.gov.uk/get-a-test Following the identification of cases of this Variant of Concern in the area that our school ( BB2 6JP) is in and neighbouring areas ( Shear Brow & Corporation Park, Billinge & Beardwood and Bastwell & Daisyfield), Blackburn with Darwen Council is working closely with Public Health England and NHS Test and Trace to develop a programme of additional PCR testing and enhanced contact tracing for these areas. -

Where Will I Live? Place Studies Schemes of Work
Where will I live? Place studies schemes of work School Scheme of Work Regional Place Specific Place Studies Featured Studies Featured Westholme School A Geographical East Lancashire Darwen Mystery Mellor St Peter's Regeneration Area Habergham High What makes an area East Lancashire Burnley School good or bad? South Cambridge Cambridgeshire Queen Elizabeth’s Where would you be East Lancashire Housing Wards Grammar School willing to live? within Blackburn- with-Darwen Bastwell Corporation Park Livesey-with- Pleasington Higher Croft Beardwood-with- Lammack Mill Hill Ivy Bank Business Opinions about East Lancashire Padiham and Technology urban change College Colne Primet High Environmental East Lancashire Colne School Quality Pendle Ribble Valley Edge End High What is all the fuss East Lancashire Whitefield School about? Nelson Coleridge Proposed East Lancashire Redevelopment of Community School redevelopment of South Marshall's Airfield and Parkside Marshall's Airfield Cambridgeshire Community School Sawston Village New housing East Lancashire East Lancashire: College developments South Burnley and Nelson Cambridgeshire South Cambridgeshire: Cambourne Northstowe Trumpington St Bede's Inter- Perceptions of East Lancashire Students own Church School and Places South localities Chesterton Cambridgeshire Localities of the Community College schools Comparison with Burnley house prices Hills Road Sixth Managing Urban South Milton Form College Environments Cambridgeshire Cambourne Northstowe Comberton Village Sustainable South Cambourne College Cambridge? Cambridgeshire Northstowe and Saffron Walden East Lancashire High School Chesterton Housing Design and South Local unusual Community College Housing Needs Cambridgeshire architect designed houses and sustainable housing developments . -

Decision Making Staff 2020|21
] Blackburn with Darwen Clinical Commissioning Group Register of Interests : Decision Making Staff 2020|21 Date of Interest Action taken to Type of Interest From To mitigate risk Current position (s) held - ie: Declared Interest NAME Governing Body, Member Nature of Interest (Name of the organisation & nature of business) Practice, Employee or other Indirect Interests Non-Financial Financial Interests Professional Interests Professional Non-Financial Personal GOVERNING BODY MEMBERS Brownhill Surgery, Blackburn X General Practitioner (GP) Partner 2014 Present East Lancashire Medical Services (ELMS) Member of a GP Practice, which is a X 2014 Present Member Would not take part in decision making or Dr Ridwaan Ahmed Clinical Director of Primary Care and Quality Blackburn with Darwen (BwD) North Primary Care Network (PCN) procurement or other activities relating to this X Clinical Director 01/07/2019 Present interest in accordance with the CCG Policy. Dr Mohammed Hussain Moosa, is a member of the CCG X Brother-in-law 2008 Present Governing Body and a GP Partner at Practice in BwD Cornerstone Practice X GP Partner 2008 Present Cornerstone Healthcare Community Integrated Care (CiC) X Director 2009 Present Member of a GP Practice, which is a Would not take part in decision making or Dr Adam Black GP Executive Member ELMS X Member and I am an Out of Hours 2008 Present procurement or other activities relating to this sessional GP interest in accordance with the CCG Policy. Cornerstone Healthcare Charity X Director 2010 Present Speech and Language Therapist for 'Speak Easy' Charity X Wife 2014 Present Torus Social Housing Company, Warrington and St Helens X Chair 2014 Present Would not take part in decision making or Mr Graham Burgess Chair Rochdale Integrated Commissioning Board X Chair 2018 Present procurement or other activities relating to this Pennine Lancashire Integrated Health and Care Partnership X Chair 2018 Present interest in accordance with the CCG Policy. -
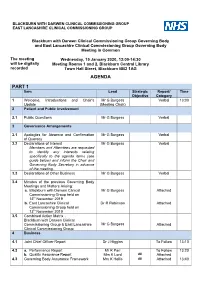
Agenda Part 1
BLACKBURN WITH DARWEN CLINICAL COMMISSIONING GROUP EAST LANCASHIRE CLINICAL COMMISSIONING GROUP Blackburn with Darwen Clinical Commissioning Group Governing Body and East Lancashire Clinical Commissioning Group Governing Body Meeting in Common The meeting Wednesday, 15 January 2020, 13:00-14:30 will be digitally Meeting Rooms 1 and 2, Blackburn Central Library recorded Town Hall Street, Blackburn BB2 1AG AGENDA PART 1 Item Lead Strategic Report/ Time Objective Category 1 Welcome, Introductions and Chair’s Mr G Burgess Verbal 13:00 Update (Meeting Chair) 2 Patient and Public Involvement 2.1 Public Questions Mr G Burgess Verbal 3 Governance Arrangements 3.1 Apologies for Absence and Confirmation Mr G Burgess Verbal of Quoracy 3.2 Declarations of Interest Mr G Burgess Verbal Members and Attendees are requested to identify any interests relating specifically to the agenda items (see guide below) and inform the Chair and Governing Body Secretary in advance of the meeting. 3.3 Declarations of Other Business Mr G Burgess Verbal 3.4 Minutes of the previous Governing Body Meetings and Matters Arising: a. Blackburn with Darwen Clinical Mr G Burgess Attached Commissioning Group held on 13th November 2019 b. East Lancashire Clinical Dr R Robinson Attached Commissioning Group held on 13th November 2019 3.5 Combined Action Matrix : Blackburn with Darwen Clinical Commissioning Group & East Lancashire Mr G Burgess Attached Clinical Commissioning Group 4 Business 4.1 Joint Chief Officer Report Dr J Higgins To Follow 13:10 4.2 a. Performance Report Mr R Parr To Follow 13:20 b. Quality Assurance Report Mrs K Lord All Attached 4.3 Governing Body Assurance Framework Mrs K Hollis All Attached 13:40 4.4 Finance Report a. -

Roe Lee Gardens at Pleckgate Blackburn a New Home
Roe Lee Gardens at Pleckgate Blackburn A new home. The start of a whole new chapter for you and your family. And for us, the part of our job where bricks and mortar becomes a place filled with activity and dreams and fun and love. We put a huge amount of care into the houses we build, but the story’s not finished until we match them up with the right people. So, once you’ve chosen a Miller home, we’ll do everything we can to make the rest of the process easy, even enjoyable. From the moment you make your decision until you’ve settled happily in, we’ll be there to help. Living in Blackburn 02 Welcome home 06 Floor plans 08 Specification 24 How to find us 36 Roe Lee Gardens 1 Plot Information Tolkien N See Page 08 Holy Souls RC Primary School Darwin See Page 10 Darwin DA See Page 12 Kipling See Page 14 24 25 26 Malory 23 See Page 16 22 Rolland 21 See Page 18 Esk See Page 20 20 Chadwick 19 7 See Page 22 31 18 6 32 27 28 29 8 33 30 5 9 34 4 10 11 3 Existing Development 17 16 2 SANDRINGHAM CLOSE 15 BLENHEIM CLOSE 1 14 13 The artist’s impressions (computer-generated 12 graphics) have been prepared for illustrative Existing Development purposes and are indicative only. They do not form part of any Existing Development contract, or constitute a representation or warranty. External appearance may be subject to variation upon completion of the project. -

Destinations by Bus Buses, Taxis and Cycle Hire Local Area Map Taxis
Blackburn Station i Onward Travel Information Buses, Taxis and Cycle Hire Local area map Blackburn is a Blackburn is a PLUSBUS area PlusBus area. Contains Ordnance Survey data © Crown copyright and database right 2018 & also map data © OpenStreetMap contributors, CC BY-SA Rail replacement buses depart from the Vue Cinema car park at the rear PlusBus is a discount price ‘bus pass’ that you buy with your train ticket. It gives you unlimited bus travel around your of the station. chosen town, on participating buses. Visit www.plusbus.info Main destinations by bus (Data correct at November 2019) DESTINATION BUS ROUTES BUS STOP DESTINATION BUS ROUTES BUS STOP DESTINATION BUS ROUTES BUS STOP 24, 24A Bus Stn Stand 6 24, 24A Bus Stn Stand 6 { Abbey Village 24, 24A Bus Stn Stand 6 { Feniscowles Riley Green 152 Bus Stn Stand 5 152 Bus Stn Stand 5 6 Bus Stn Stand 11 6 Bus Stn Stand 11 6 Bus Stn Stand 11 { Accrington ^ { Great Harwood { Rishton ^ 7, 7A Bus Stn Stand 13 7 Bus Stn Stand 13 152 Interchange stop 4 { Altham 152 Interchange stop 4 { Guide ^ 481 Interchange stop 2 { Royal Blackburn Hospital 12A, 12C, 22, 481 Interchange stop 2 10 Bus Stn Stand 4 { St Mary's College (Blackburn) Astley Bridge 1 Interchange stop 1 Haslingden 481 Interchange stop 2 25, 45 Bus Stn Stand 1 { Audley Range 22 Interchange stop 2 Highercroft 12A, 12C Interchange stop 2 Salesbury 45 Bus Stn Stand 1 Beardwood { 59 Bus Stn Stand 3 Higher Walton 152 Bus Stn Stand 5 Samlesbury 59 Bus Stn Stand 3 (For BMI Beardwood Hospital) { Belthorn 481 Interchange stop 2 Hoghton 152 -

Local Authority Major Scheme Decisions
Local Highways Maintenance Challenge Fund Application Form (for Tranche 2A) The level of information provided should be proportionate to the size and complexity of the scheme proposed. Note that DfT funding is a maximum of £5 million per scheme. An individual local authority may apply only for one scheme. For schemes submitted by components of a Combined Authority a separate application form should be completed for each scheme, then the CA should rank them in order of preference. Applicant Information Local authority name: Blackburn with Darwen Borough Council Bid Manager Name and position: Ian Richardson, Director of Growth and Development Name and position of officer with day to day responsibility for delivering the proposed scheme. Contact telephone number: 01254 273 255 Email address: [email protected] Postal address: Growth and Development Blackburn with Darwen Borough Council Town Hall Blackburn BB1 7DY Combined Authorities If the bid is from a local highway authority within a Combined Authority, please specify the contact and ensure that the Combined Authority has submitted a Combined Authority Application Ranking Form. Name and position of Combined Authority Bid Co-ordinator: N/A Contact telephone number: Email address: Postal address: When authorities submit a bid for funding to the Department, as part of the Government’s commitment to greater openness in the public sector under the Freedom of Information Act 2000 and the Environmental Information Regulations 2004, they must also publish a version excluding any commercially sensitive information on their own website within two working days of submitting the final bid to the Department. The Department reserves the right to deem the business case as non- compliant if this is not adhered to. -

The Blackburn with Darwen (Electoral Changes) Order 2017 No
Draft Legislation: This is a draft item of legislation. This draft has since been made as a UK Statutory Instrument: The Blackburn with Darwen (Electoral Changes) Order 2017 No. 1270 DRAFT STATUTORY INSTRUMENTS 2017 No. The Blackburn with Darwen (Electoral Changes) Order 2017 Citation and commencement 1.—(1) This Order may be cited as the Blackburn with Darwen (Electoral Changes) Order 2017. (2) This article and article 2 come into force on the day after the day on which this Order is made. (3) Articles 3 and 4 come into force— (a) for the purpose of proceedings preliminary, or relating, to the election of councillors, on the day after the day on which it is made; (b) for all other purposes, on the ordinary day of election of councillors in England and Wales(1) in 2018. (4) Articles 5 and the Schedule come into force— (a) for the purpose of proceedings preliminary, or relating to, the election of councillors, on the day after the day on which it is made; (b) for all other purposes, on the ordinary day of election of councillors in England and Wales in 2020. Interpretation 2.—(1) In this Order “the map” means the map marked “Map referred to in the Blackburn with Darwen (Electoral Changes) Order 2017”, held by the Local Government Boundary Commission for England(2). (2) Where a boundary is shown on the map as running along a road, railway line, footway, watercourse or similar geographical feature, it is to be treated as running along the centre line of the feature. Wards of the borough of Blackburn with Darwen 3.—(1) The existing wards of the borough of Blackburn with Darwen are abolished. -

Borough Election
NOTICE OF POLL Blackburn with Darwen Election of a Borough Councillor for Audley & Queen`s Park Notice is hereby given that: 1. A poll for the election of a Borough Councillor for Audley & Queen`s Park will be held on Thursday 6 May 2021, between the hours of 7:00 am and 10:00 pm. 2. The number of Borough Councillors to be elected is one. 3. The names, home addresses and descriptions of the Candidates remaining validly nominated for election and the names of all persons signing the Candidates nomination paper are as follows: Names of Signatories Name of Candidate Home Address Description (if any) Proposers(+), Seconders(++) & Assentors BATAN (Address in Blackburn) Labour Party Maherunnisa Jogee (+) Khatija Sidat (++) Maryam PATEL 24 St. Thomas Street, The Conservative and Ibrahim Patel (+) M Asharaf Mangera Tiger Blackburn, BB1 1PB Unionist Party (++) 4. The situation of Polling Stations and the description of persons entitled to vote thereat are as follows: Station Ranges of electoral register numbers of Situation of Polling Station Number persons entitled to vote thereat Church of Jesus Christ of Latter Day Saints, Lambeth Street, 1 AQ1-1 to AQ1-956 Blackburn Accrington Road Community Centre, Accrington Road, 2 AQ2-1 to AQ2-2301 Blackburn Audley & Queen`s Park Neighbourhood Learning Ctre, Pringle 3 AQ3-1 to AQ3-1656 Street, Blackburn Audley & Queen`s Park Neighbourhood Learning Ctre, Pringle 4 AQ4-1 to AQ4-1418 Street, Blackburn 5. Where contested this poll is taken together with the election of Parish Councillors and the election of Police and Crime Commissioner. Dated Tuesday 27 April 2021 Denise Park Returning Officer Printed and published by the Returning Officer, Town Hall, King William Street, Blackburn, Lancashire, BB1 7DY NOTICE OF POLL Blackburn with Darwen Election of a Borough Councillor for Bastwell & Daisyfield Notice is hereby given that: 1. -

MEDICO-LEGAL CURRICULUM VITAE Dr. Joshua Adedokun FCARCSI, FRCA, FFPMRCA Consultant in Pain Medicine
Medicolegal Curriculum Vitae Dr Joshua Adedokun,Consultant in Pain Medicine MEDICO-LEGAL CURRICULUM VITAE Dr. Joshua Adedokun FCARCSI, FRCA, FFPMRCA Consultant in Pain Medicine www.expertpainreports.co.uk March/April 2014 1 Medicolegal Curriculum Vitae Dr Joshua Adedokun,Consultant in Pain Medicine Personal Details Name: Joshua Adedokun Address: Suite 5,Wilmslow House Grove Way,Water Lane Wilmslow, Cheshire, SK9 5AG Email contact; [email protected] Medico legal PA; Nikki Richmond Suite 5,Wilmslow House Grove Way,Water Lane Wilmslow, Cheshire SK9 5AG Tel- 01625 526665 ; 07885913912 E-mail- [email protected] Qualifications; MBBS - 1990 Diploma in Anaesthesia -1999 Fellow of the College of Anaesthesia of the Royal College of Surgeons of Ireland 2004 Fellow of the Royal College of Anaesthetists -2004 NHS Employment; The Pennine Acute NHS Trust (North Manchester General Hospital) GMC Status- Registered with a licence to practice, 5204343 Medico-legal practice; 10 Harley Street, London 88 Rodney Street, Liverpool Spire Manchester Hospital, Manchester Roselands Consulting Rooms, Crumpsall, Manchester The Beardwood Hospital, Blackburn (BMI Group) The Beaumont Hospital, Bolton (BMI Group) The Oakland Hospital, Salford (Ramsey Group) (Other Locations are arranged as required) March/April 2014 2 Medicolegal Curriculum Vitae Dr Joshua Adedokun,Consultant in Pain Medicine Summary of medical practice, expertise and professional interests Professional qualifications: Dr Adedokun became a Fellow of the College of Anaesthetists of the Royal College of Surgeons of Ireland in 2004, in the same year became a Fellow of the Royal College of Anaesthetist. He was granted Fellowship by assessment of the Faculty of Pain Medicine of the Royal College of Anaesthetists in 2009. -
Blackburn Central Library
GB 0332 DDX 1936 Blackburn Central Library This catalogue was digitised by The National Archives as part of the National Register of Archives digitisation project NRA 39910 JA The National Archives DDX 1936 Documents relating to the Woodfold Estate, Pleasington, Blackburn Deposited by Daniel Thwaites pic, Eanam, Blackburn 1991 (acc 7200) but held at Blackburn Library Lancashire Record Office Bow Lane PRESTON PR1 2RE CEH/JB DDX 1936 THE WOODFOLD ESTATE John Fowden Hindle purchased the Woodfold Estate from the Suddell family in the 1820s. He died in 1831 and his will was proved the same year. However, the settling of his estate, by trustees, continued for decades. His son John Fowden Hindle (junior) died in 1849 and gradually property was let or sold. Daniel Thwaites rented Woodfold in the late 1850s for 10 years and i t was probably his son, Daniel Thwaites (junior), who bought it in 1865. When he died in 1888 the estate passed to trustees and to his daughter Elma Amy, who married Robert Armstrong Yerburgh. In 1897, the trustees set up a limited liability company known as Woodfold Estates. In 1926, Amy Yerburgh set up the Woodfold Estates Company Limited. During her lifetime she held property in London on Addison Road, at Princess Gate and at 25 Kensington Gore; at Caythorpe Court in Lincolnshire; at Freeby in Leicestershire; at Colwyn Bay in North Wales: Bryn Eithin and Cae Eithin (the latter was sold for building plots); and at Barwhillanty in Kirkcudbrightshire, Scotland. Mrs. Yerburgh died in 1949 and from 1955 the estates and brewery were managed separately from adjacent offices at Eanam, Blackburn DDX 1936 Contents 1. -
Beardwood with Lammack Ward Profile 2011 Census
2011 Census - simple statistics for Beardwood with Lammack ward Figure 1 - Beardwood with Lammack ward Introduction This briefing provides a summary of the 2011 Census data for Beardwood with Lammack Ward, arranged under the headings ‘Who we are’, ‘How we live’ and ‘What we do’. The original version of these briefings was based on the simple Census tables available as at January 2013. Since then, much more detailed and complex Census data has been released, but this briefing still aims to keep things as simple as possible. The only use made of the newer tables has been to introduce new or improved age breakdowns where this is felt to be of benefit. Health data is now presented by age-group, so that the reader can make fair comparisons between places with different age profiles. The ‘What we do’ section is now able to focus on the 16-64 age-group, which is probably closer to most people’s idea of ‘working age’ than the original 16-74. 1 March v.2 Introduction 2014 Beardwood with Lammack ward Who we are Figure 2 - Beardwood with Lammack population Population size (2011 Census) by age and sex The previous Census in 2001 found that the Source: Tables PP05 and PP06 population of Beardwood with Lammack was approximately 5483. The latest results from the 2011 Census show that this number has risen to 5997. Age structure Figure 2 shows the 5997 population of Beardwood with Lammack broken down by age and sex. 25.3% of its population is aged 0-19, compared with 28.7% for Blackburn with Darwen as a whole.