Exploring the Links Between Drug Use and Sexual Vulnerability Among Young Female Injecting Drug Users in Manipur
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Format of Test-Check Report Under ADIP Scheme
Format of Test-Check Report under ADIP Scheme Test Check (Minimum of 10/15 percent*) of beneficiaries assisted during the year 2020-21 Name of the Implementing Agency - SVNIRTAR, Olatpur PART-I State: MANIPUR District: IMPHAL Sl. No. Name of Benificiary Father's/Husband's Male/ Age Complete Address Contact Type of Aid Place of Date of Date of Test name Female Number given Camp Camp Check surgical working check(e.g. distribution Whether any confirmed & Finding of test- Sl. No. of list of correction taken well/distribution the covered Beni. 1 2 3 4 5 6 7 8 9 10 11 12 13 14 C/O N. INGOCHA SINGH AT C/O N. INGOCHA PUKHAO PO IMPHAL PS SINGH AT PUKHAO PO IMPHAL DIST IMPHAL WEST IMPHAL PS IMPHAL Working well & IMPHAL, 1 1 NAOREM BEMMA DEVI MANIPUR F 19Y DIST IMPHAL WEST X SMART PHONE Nil Distribution MANIPUR MANIPUR confirmed 15.12.2020 16.12.2020 C/O MAIBAM SANJOY SINGH C/O MAIBAM SANJOY AT THANGJINA IMPHAL DIST SINGH AT THANGJINA IMPHAL WEST MANIPUR IMPHAL DIST IMPHAL Working well & SMART CANE & IMPHAL, 2 2 MAHIBAM PREETY DEVI F 16Y WEST MANIPUR Nil Distribution SMART PHONE MANIPUR confirmed 15.12.2020 9615432561 16.12.2021 AT NAMBOL PO BISHNUPUR AT NAMBOL PO PS BISHNUPUR DIST BISHNUPUR PS BISHNUPUR STATE MANIPUR BISHNUPUR DIST Working well & THOKCHOM JOHNSON IMPHAL, 3 3 M 29Y BISHNUPUR STATE SMART PHONE Nil Distribution SINGH MANIPUR MANIPUR confirmed 15.12.2020 9856699004 16.12.2022 AT OINAM SHAWOMBONG AT OINAM PO IMPHAL DIST IMPHAL SHAWOMBONG PO WEST STATE MANIPUR IMPHAL DIST IMPHAL Working well & KHULAKDAM RABINA IMPHAL, 4 4 F 21Y WEST -

Studies on Nematode Parasites of Fishes of Oinam Lake Bishnupur District, Manipur, India
AL SCI 264 UR EN T C A E N F D O N U A N D D A E I Journal of Applied and Natural Science 3 (2): 264-267 (2011) T L I O P N P A JANS ANSF 2008 Studies on nematode parasites of fishes of Oinam lake Bishnupur district, Manipur, India O. Sangeeta ¹, M. Shomorendra² and Devashish Kar¹* ¹Division of Wetlands, Fishery Science and Aquaculture Biotechnology, Department of Life Science, Assam (Central) University, Silchar – 788011, INDIA ²Fish Disease Research Lab., Department of Zoology, Thambal Marik College, Oinam -795134 (Manipur), INDIA *Corresponding author. E mail: [email protected] Abstract: An extensive survey was done for fish nematode parasites of few economically important fishes of Oinam Lake, Bishnupur district, Manipur. 9 species of nematodes were encountered. They are Camallanus anabantis, Procamallanus (Procamallanus) saccobranchi, Paraquimperia manipurensis, Paragendria sp., juvenile stages of genus Syphacia, Haplonema, Spinitectus, Philometra and Parascarophis etc. Of these nematode species, Procamallanus (Procamallanus) saccobranchi, Paragendria sp and Haplonema sp. showed maximum abundance (14.28%) and Paraquimperia manipurensis, Parascarophis sp. showed minimum abundance (4.76%) of parasites. Among the fish species Anabas testudineus had highest percentage (50%) of parasites and Puntius sophore and Colisa labiosus had lowest percentage (1.25%) of parasites. Keywords: Nematode parasites, Fishes, Oinam lake, Manipur INTRODUCTION water fishes in different climate zones of the world. Kar Fish is a vital source of human food particularly in terms (2007) and Kar and Sen (2007) Studied on systematices of high quality proteins. For the people of Eastern India list and distribution of fish biodiversity in Mizoram, in general, and North East in particular, fish constitutes a Tripura and Barak drainage in North East India. -

District Census Handbook Bishnupur
DISTRICT CENSUS HANDBOOK BISHNUPUR 1 DISTRICT CENSUS HANDBOOK BISHNUPUR 2 DISTRICT CENSUS HANDBOOK BISHNUPUR H A T I M P To Imphal MANIPUR C L I BISHNUPUR DISTRICT 1012 R R NAMBOL ! T NAMBOL Kilometres (M Cl) S W NH 2 6 I 6 ! OINAM D (N P) LEIMAPOKPAM I ! E r e NAMBOL SUB-DIVISION iv T R l u b A m a S N P r e v A i R a T h N c a NH 2 m o E i NGAIKHONG g n KHULLEN a Y S ! BISHNUPUR! (M Cl) C G D P BISHNUPUR 6 6 KHOIJUMAN r H Thon gjao KHULLEN e ro v k i Rive r R l I 6 u NINGTHOUKHONG b m a ! AWANG(PT) N U NINGTHOUKHONG (M Cl) S L O K T A K L A K E R BISHNUPUR SUB-DIVISION T A R C Area (in Sq. Km.)................ 496 THANGA ! Number of Sub-Divisions.... 3 Number of Towns.... 7 Number of Villages.............. 49 I H INDIA C A ! r NH 2 MOIRANG MOIRANG e R v i (M Cl) R BOUNDARY, DISTRICT........................................................ N k 6 a T ,, d r SUB-DIVISION............................................... o MOIRANG SUB-DIVISION h K ! HEADQUARTERS: DISTRICT............................................. P ! ! KHA THINUNGEI D KWAKTA (PART) ,, KWAKTA SUB-DIVISION..................................... R ! KUMBI (N P) T THANGA (N P) VILLAGES HAVING 5000 AND ABOVE POPULATION WITH NAME ! P ! C URBAN AREA WITH POPULATION SIZE: IV & V ............. ! I NH 2 NATIONAL HIGHWAY.......................................................... U R SH WANGOO STATE HIGHWAY................................................................ iver AHALLUP Khu ga R ! T IMPORTANT METALLED ROADS..................................... -

State / Ut : Manipur Nodal Cpsu
REGISTRATION & ATTENDANCE AND RECEIPT OF MEMENTOS AND ID CARDS ANNEXURE - 7 STATE LEVEL PAINTING COMPETITION ON ENERGY CONSERVATION - 2018 STATE / UT : MANIPUR GROUP - A NODAL CPSU : NHPC LIMITED SCHOOL NAME / ADDRESS Sl.No. NAME OF STUDENT FATHER'S / MOTHER'S NAME STD. REMARKS TEL. No. ETC. PH. PREMJIT SINGH CLASS: V 1 PHILEM SAIPRINCY DEVI MOIRANG L.C.M HIGH SCHOOL MOIRANG ROLL NO. 1 PH.NO. 7005844746 M. ROCKY SINGH CLASS: V 2 MOIRANGTHEM THAJAMANBI DEVI TENTHA KHONGBAL MAYAI LEIKAI INAOBI NINGSHING MAHEIKOL TENTHA ROLL NO.15 PH.NO.9856721049 CLASS: VI 3 N. NIHAR SINGH PH.NO. 7005096089 THANGAL GENERAL ACADEMY SAITON ROLL NO. SINAM SANAHAL KHAGEMPALLI PANTHAK CLASS: V 4 LANLEIBA SINAM RAMAKRISHNA MISSION SCHOOL IMPHAL PH.NO. 9612161220 ROLL NO. 14 8837249904 BISHNUPUR KHA GOVT JUNIOR CLASS: IV 5 NAOREM SARIKA DEVI PH.NO. 9862337229 BISHNUPUR HIGH SCHOOL ROLL NO. 11 M. RAJKUMAR SINGH NINGTHOUKHONG MAMANG CLASS: V 6 MOIRANGTHEM REYMASTRIO SINGH NINGTHOUKHONG W/NO.13 NINGTHOUKHONG JR HIGH SCHOOL ROLL NO. 13 PH.NO. 7629090810 L. INAOCHA MEITEI CLASS: VI 7 LAISHRAM SAMUAL MEITEI PHUBALA CAREER FOUNDATION ACADEMY PHUBALA ROLL NO. 14 PH.NO. 9378071258 H. BASANTA SINGH KHOIJUMAN,BISHNUPUR CLASS: VI 8 HAOBIJAM VISHAL SINGH KHOIJUMAN EMINENT SCHOOL 7005392803 ROLL NO. 8 PH.No.7005391803 M. GHANASHYAM SINGH CLASS: V 9 MAIBAM PARBING SINGH MOIRANG THE LITTLE BIRDS SCHOOL MOIRANG ROLL NO. 31 PH.NO. 985202770 TH. ANIL SINGH LANGJING CLASS: VI 10 TH. SANATHOI LANGJING HIGH SCHOOL IMPHAL PH.NO. 9856938756 ROLL NO. 9856938754 P. SOMOKANTA SINGH CLASS: V 11 PUKHRAMBAM SUSHIL SINGH MOIRANG L.C.M HIGH SCHOOL MOIRANG ROLL NO. -

No DEO/IE/PP/11/2006
OFFICE OF THE DISTRICT ELECTION OFFICER: IMPHAL EAST DISTRICT ORDER OF APPOINTMENT OF POLLING OFFICER - III No: DEO/DC(IE)/5/REQ-PP/2019: In pursuance of section 26 of the Representation of the People Act. 1951, I hereby appoint the following officers as Polling Officer - III in the No. 1-Inner Manipur Parliamentary Constituency for Election to the 17-House of People (Lok Sabha) 2019 under Imphal East District. Sl No NAME DEPARTMENT & DIVISION DESIGNATION ADDRESS 1 M BROJENDRO SINGH Public Works Department-MECHANICAL DIVISION NO I Fitter SAGOLBAND MEINO LEIRAK S KHRISHNAMANI 2 Public Works Department-MECHANICAL DIVISION NO I Handyman KHURAI THANGJAM LEIKAI SHARMA THANGMEIBAND MEISNAM 3 Y IBOHANBI SINGH Public Works Department-MECHANICAL DIVISION NO I Bill Assistant LEIKAI 4 MD YUNUS KHAN Public Works Department-MECHANICAL DIVISION NO I Bill Assistant HIYANGTHANG TARAHIE 5 TH NGALAWON Public Works Department-MECHANICAL DIVISION NO II Cane Woman PATSOI 6 MD AYAJUDDIN Public Works Department-MECHANICAL DIVISION NO II Carpenter KHETRIGAO 7 M MANAO SINGH Public Works Department-MECHANICAL DIVISION NO II Carpenter NINGOMBAM MAYAI LEIKAI 8 K IBOPISHAK SINGH Public Works Department-MECHANICAL DIVISION NO II Jugali SOIBAM LEIKAI 9 L SHYAMO SINGH Public Works Department-MECHANICAL DIVISION NO II Jugali HEINGANG KONGPAL CHINGANGBAM 10 CH DHANANJOY SINGH Public Works Department-MECHANICAL DIVISION NO II Jugali LEIKAI 11 O IBOMCHA SING Public Works Department-MECHANICAL DIVISION NO II Jugali KAKWA HUIDROM LEIKAI 12 T GITHCANDRA SINGH Public Works -

Numerals in Sihai Tangkhul
THE DAWN JOURNAL VOL. 3, NO. 2, JULY - DECEMBER 2014 NUMERALS IN SIHAI TANGKHUL Soibam Imoba Singh Oinam Nanao Devi ABSTRACT In this paper, a detail description of numerals of Sihai Tangkhul which comes under Naga-Kuki sub group of Tibeto-Burman language family is present. Sihai Tangkhul is a language spoken by a small tribe, inhabited in the Central sub-division of Ukhrul district (Manipur) with a population of 1,239 in a village called Sihai Khullen. Among 214 villages with their different languages, they communicate either in Standard Tangkhul which is spoken in proper Ukhrul or Manipuri (the officialese of the state). The paper attempts to give the numeral system of Sihai Tangkhul. The formation of numeral in Sihai Tangkhul has three systems: (a) Addition (from 11-19, direct addition) and (from 21-29, complex addition). (b) Multiplication (only 30, direct multiplication) and (from 40-1000, complex multiplication). (c) Multiplication plus addition. Basic Cardinals are identified by different names and higher numerals are identified on the basis of cardinal numerals. INTRODUCTION Sihai Tangkhul is spoken at Sihai Village of Ukhrul District. It is about 118 km from Imphal, the Capital of Manipur. Number of population is 1239 only. There are 214 villages in this hilly district. Since each village has different language, the Tangkhul tribes learn a second language i,e Standard Tangkhul which is spoken at proper Ukhrul for communication. Linguistically this Tangkhul is under the sub-group of Naga-Kuki which is under Naga Group of Tibeto-Burman Language family (Grierson, 2006). Educationally from Primary level onwards, different Tangkhul speakers neglect learning their first language. -

District Census Handbook, Bishnupur, Part-XII a & B, Series-15
CENSUS OF INDIA 2001 SERIES-IS MANIPUR DISTRICT. CENSUS HANDBOOK Part XII - A & B BISHNUPUR VILLAGE & TOWN DIRECTORY & VILLAGE AND TOWNWISE PRIMARY CENSUS ABSTRACT S.V.Ukey Deputy Director of Census Operations, Manipur Product Code Number ??-???-2OO1 - Cen-Book (E) DISTRICT CENSUS HANDBOOK: BISHNUPUR Sangai 'Sanga;', the brow antlered deer, is also known as the dancing deer ofManipur. Listed as a very rare and endangered species, the animal is found in its natural habitat form only in the Keibul Lamjao National Park, a wild sanctuary offloating aquatic plants situated at the south-western portion ofthe Loktak Lake ofBishnupur District about 53 kms from Imphal. Sanga; is now a protected species in the state under the scheme for conservation ofwild life. (iii) DISTRICT CENSUS HANDBOOK: BISHNUPUR Blank (iv) DISTRICT CENSUS HANDBOOK: BISHNUPUR Contents Pages Foreword IX Preface xi Acknowledgements XlIl District highlights ~ 200 I Census XlV Important statistics in the district XV Ranking of Tahsils in the district XVll Statements 1-9 Statement~ 1: Name of the headquarters of district/sub-division, their rural-urban status and distance from district headquarters, 2001 XiX Statement-2: Name of the headquarters of district/TO/CD block their rural urban status and distance from district headquarters, 200 I XiX Statement-3: Population of the district at each census from 1901 to 2001 XiX Statement-4: Area, number of villalges/towns and population in district and sub- xx division, 2001 Statement-5: T.D/C.D. Block wise number of villages and rural population, 2001 xx Statement-6: Population of Urban Agglomerations/towns, 2001 XXI Statement-7: Villages with population of 5,000 and above at T.D/C.D. -

Agriculture Department Felicitates Minister Oinam Lukhoi
IMPHAL, TUESDAY, DECEMBER 8, 2020 AR gifts sports equipments 26th Moirangthem Ibotombi Agriculture Department felicitates IMPHAL, Dec 7 Assam Rifles today distributed sports equipment at Chingrel Memorial Day observed Minister Oinam Lukhoi Tejpur village of Imphal East as a part of the ongoing Khelo Constituency who are de- IMPHAL, Dec 7 (DIPR) India programme. prived of the State Based on the requirement of sports equipment projected Government's pension The Minister for Agriculture, by the locals, Assam Rifles undertook the project in sync scheme till December 12 by Veterinary and Tourism, with the Government of India's youth engagement and pro- adhering to the SOPs of Oinam Lukhoi Singh was moting sport's programme, said a statement released by PRO COVID-19. felicitated today by the Assam Rifles. The programme was attended by Commander He further stated the Department of Agriculture, 9 sector AR, who talked about the importance of sports and dream of the Trust striving Government of Manipur at health. for a peaceful Manipur free Farmers’ Training Hall, The event was attended by the local villagers who lauded from all the violent forces Directorate of Agriculture, the efforts of Assam Rifles for its initiative in reaching out has been achieved to a cer- Sanjenthong, Imphal. to the locals and promoting the culture of sports in the area, tain level and thanked the Speaking at the occasion, added the statement. By Our Staff Reporter Ibotombi. Later on pensions people of Heirok A/C for Minister Lukhoi expressed Assam Rifles also organised today a Jan Andolan Covid were distributed to the eld- their major contributions in gratitude to the Chief Minis- awareness programme at villages of Suvompa, Thinghai, THOUBAL, Dec 7 : The 26th erly people and widows of such a venture since the last ter, N Biren Singh for his Pallel and Anthi of Chandel. -
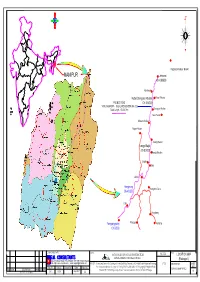
WORK\NHIDCL\Manipur\DRAWING YN UJ SETUP\KEY
L A N D U S E / L A N D C O V E R IMPHAL EAST DISTRICT , MANIPUR ( RESTRICTED CIRCULATION AMONG INTENDED AND AUTHORISED USERS ONLY ) K e Thonamba ith T e lm KeithenmanbiTumnoupokpi an S b i-T ho n a C m b a R 9 o a 3 d - E H N I Matakkhong Heinoupok Makengngularou Bolsang-Kholjang Road M R N o Khoirentampak ln o m - J a Makeng n g m Khonjin Khongjail o T l R o A a d S Kuraopokpi g n P a r i ® o K I 0 1.25 2.5 5 u d Im a S p 800 h # a l - A S D a Puramkhunou ik Kilometers u l R o a d Sadanglonga 807 # T I Puram_Likli aharup Pukhao N Ekpal khunou T I Kanglatongbi A Pukhoahallup Pukhao Khabam Ja mm u & P Khewa Company o K a a d sh h m a k ir o u R P Thongnagpal i Khongban Tangkhul a Ekpalkhullen m k b Himachal Pradesh e A D ja S n S a u g P Chandigarh o lm Sekmai an Haryana d g oa Delhi U R Sin tt Keingamkhunou a S a N m Uyumpok r m i Yumam Patlou P Aarunachal Pradesh n ra g a d in m 968 Rajasthan e e s Sikkim K k # h o 196 I m # S sam As e R k Y o Purumkhulen Nagaland m Meghalaya u a La Tingri E m d mb Bihar a oik Manipur to i n h Kanto an ul K R d N Gujarat g a Tripura o m West Bengal Le a P a a o i Madhya Pradesh im o ra Mizoram d K t a R n s g h k i h b h u S o a Leikinthabi a aretkhul u a T n o P m n n g n m Maharabi S o o g Dadra and Nagar Haveli R u k t u a b e d oa h s u Orissa a a Khurkhul d K S um o n m K Maharashtra t g l i ho H b n b k e R g a a In a K K Tendongyan k u Keibikhulen Laikot m o ro r o a o n Road a M r ei K L donya o mb 812 h e Ten R d ha # ur i l w S uk m o o a sh h a u r e ul Potsangbamkhoiru a R k d a T ad o h -

Untitled Spreadsheet
Nambol L. Sanoi College, Nambol BSc 1st sem online applicants list YEAR OF SL.No. APPLICATION NO. APPLIED DATE COURSE SUBJECT COMBINATION APPLICANT NAME DATE OF BIRTH GENDER CATEGORY PARMANENT ADDRESS STREAM NAME OF BOARD STATUS PASSED 1 UHEM2020027646 17-09-2020 BSC CHE, ZOO, BOT ABUJAM PUSPARANI 16-01-2000 Female UR KHAJIRI MAMANG LEIKAI,NAMBOL Science COHSEM 2017 Applied 2 UHEM2020002395 19-08-2020 BSC BOT, ZOO, GEOG Akoijam Sonia Devi 24-03-2003 Female UR Khoijuman Mayai Leikai Science COHSEM 2020 Applied 4 UHEM2020017285 19-08-2020 BSC CHE, ZOO, BOT Angela Mayanglambam 03-03-2003 Female UR Malom awang leikai opposite army camp Science Telangana board 2020 Applied 5 UHEM2020024000 31-08-2020 BSC BOT, ZOO, GEOG ANJALI YUMNAM 05-03-2003 Female UR Malom Tuliyaima Awang Leikai; PO-Tulihal; PS-Nambol Science COHSEM 2020 Applied Uripok Naoremthong Takhellambam Leikai, Imphal, 8 UHEM2020001459 03-08-2020 BSC BOT, ZOO, GEOG BANDANA KONTHOUJAM 06-02-2003 Female OBC Science COHSEM 2020 Applied Manipur 9 UHEM2020028526 22-09-2020 BSC CHE, ZOO, BOT Chelsea Sinam 29-03-2003 Female OBC Malom Tulihal Makha Leikai Science COHSEM 2020 Applied 10 UHEM2020018832 22-08-2020 BSC CHE, ZOO, BOT CHINGAKHAM MENAKA DEVI 01-04-2003 Female UR Kangmong Trongbam Leikai Science COHSEM 2020 Applied 11 UHEM2020003772 22-09-2020 BSC CHE, ZOO, BOT Chizine Apoumei 22-03-2001 Female ST Tungam khullen village Science COHSEM 2020 Applied 12 UHEM2020001283 03-08-2020 BSC BOT, ZOO, GEOG CHONGTHAM BANDANA DEVI 04-10-2002 Female OBC KANGMONG LANGOLJAM MANING LEIKAI Science COHSEM 2020 Applied 13 UHEM2020025359 05-09-2020 BSC BOT, ZOO, GEOG Gurumayum Tereja Devi 05-03-2003 Female UR Bishnupur C.I. -

1St Selection List of B.A, 2020
SL. NO. APPLICATION NO. APPLICANT NAME Subjects Offered Address BOARD Year P.C. MOBILE NO. SEX CATEGORY 1 UHEM2020004832 MOIRANGTHEM SAYALUXMI DEVI PSC, ESL , HIS Moirang Thana leikai F SC CBSE 2020 95 9612232930 2 UHEM2020015706 K SURBASON SINGH GEG, EDN, HIS moirang phairembam leikai M SC CBSE 2019 87.25 9402651311 3 UHEM2020000401 NONGTHANG MOIRANGTHEM GEG, EDN, MAT Khangabok Part 3 Tangkha Leikai M GEN COHSEM 2012 85 9971349541 4 UHEM2020000401 NONGTHANG MOIRANGTHEM GEG, ECO, MAT Khangabok Part 3 Tangkha Leikai M GEN COHSEM 2012 85 9971349541 5 UHEM2020007563 AFSANA GEG, EDN, HIS KWAKTA WARD NO. 8 F UR COHSEM 2020 83 8723011566 6 UHEM2020005544 RANITA HEMAM PSC, ESL, MSL Sagolband nepra major leikai F SC CBSE 2020 82.8333333333333 9366680710 7 UHEM2020003180 OINAM BHAGAT SINGH GEG, PSC, HIS NARANSEINA AWANG M SC COHSEM 2020 80.6666666666667 8787687029 LEIKAI,Bishnupur,Manipur - 795133,India 8 UHEM2020013246 MOIRANGTHEM GYANESHWORI DEVI GEG, MSL, HIS Thamnapokpi,Moirang F SC COHSEM 2020 80.3333333333333 9089174129 9 UHEM2020000758 HUIREM SHWETA DEVI GEG, PSC, HIS Moirangkhunou Huirem leirak Bishnupur district F OBC COHSEM 2020 79.75 9612639781 10 UHEM2020010675 PRAVASWORI DEVI ELANGBAM PSC, MSL, HIS Takyel khongbal maning leikai, Imphal west F OBC COHSEM 2020 79.6666666666667 9856403562 11 UHEM2020016786 RISHIDAS KONJENGBAM ECO, EDN , PSC MOIRANG THANA LEIKAI M SC CBSE 2020 79.2 8415024648 12 UHEM2020002859 DHANACHANDRA MAIREMBAM PSC, ESL , HIS Moirang M GEN COHSEM 2020 79.1666666666667 6009918880 13 UHEM2020002886 DHANACHANDRA MAIREMBAM -
Officer of the Ministry of Women & Child
No. 141312017-wWH Government of India Ministry of Women and Child Development Shastri Bhavan, A Wing Dr. Rajendra Prasad Road New Delhi- 1 10001 Dated :27.O9.2017 To The Pay and Accounts Of{icer, Ministry of Women and Child Development, New Delhi. Subject : Scheme of Assistance for Construction of Hostel Building for Working Women with Day Care Centre for Children- Grants-in- to Pioneer Welfare Association, Manipur - Release of first installment. Sir, I am'directed to say that the Government of India has sanctioned a non- recurring grant of Rs. L,67,80,646/- (Rupees One Crore Sixty Seven Lacs Eighty Thousand Six Hundred Forty. Six only) as Central Government's share for construction of a Working Women's Hostel for lOO working women and Day Care Centre for 25 children at Oinam, Nambol C.D. Block, Bishnupur, Manipur. The grant for construction of hostel building represents 75%o of the total estimated cost of Rs. 2,23,74,I951- (Rupees TWo Crore Twenty Three Lakh Seventy Four Thousand One Hundred Ninety Five only) as admitted for construction of the working women's hostel subject to the condition that in case the actual expenditure on this project is less than the estimated cost,7Soh of the difference between the estimated cost and the actual expenditure is required to be refunded by the organizalion to the Ministry. 2, I am, accordingly, to convey the sanction of the President to the payment to the Pioneer Welfare Association, Manipur of a sum of Rs. 83,90,323/- (Rs. Eighty Three Lacs Ninety Thousand Three Hundred Twenty Three only) being the first installment of the grant for the construction of the building which wili be used as a hostel for working women.