Health Options Program
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacies Located in North Carolina
Blue Cross and Blue Shield of North Carolina Limited Network: Pharmacies Located in North Carolina Pharmacy Name Address City State Zip Phone Number 1ST RX PHARMACY 837 N CENTER ST STATESVILLE NC 28677 7048720880 1ST RX PHARMACY INC- GREENBRIAR 308-A MOCKSVILLE HWY STATESVILLE NC 28625 7048786225 A1 PHARMACY AND SURGICAL SUPPLY LLC 124 FOREST HILL RD LEXINGTON NC 27295 3362246500 A2Z HEALTHMART PHARMACY 1408 ARCHDALE DR CHARLOTTE NC 28210 9803550906 ABERDEEN PRESCRIPTION SHOPPE 1389 N SANDHILLS BLVD ABERDEEN NC 28315 9109441313 ADDICTION RECOVERY MEDICAL SERVICES 536 SIGNAL HILL DRIVE EXT STATESVILLE NC 28625 7048181117 ADULT CLINIC AND GERIATRIC CENTER A 25 OFFICE PARK DRIVE JACKSONVILLE NC 28546 9103534878 ADVANCED HOME CARE 4001 PIEDMONT PKWY GREENSBORO NC 27265 3368788950 AKERS PHARMACY INC 1595 E GARRISON BLVD GASTONIA NC 28054 7048653411 ALBEMARLE COMPNDN N PRESCRIPT CNT 944 N FIRST ST ALBEMARLE NC 28001 7049836176 ALBEMARLE PHARMACY 105 YADKIN ST ALBEMARLE NC 28001 7049838222 ALLCARE PHARMACY SERVICES, LLC 5176 NC HIGHWAY 42 W STE H GARNER NC 27529 9199267371 ALLEN DRUG 220 S MAIN ST STANLEY NC 28164 7042634876 ALLEN DRUGS INC 9026 HIGHWAY 17 POLLOCKSVILLE NC 28573 2522245591 ALMANDS DRUG STORE 3621 SUNSET AVE ROCKY MOUNT NC 27804 2524433138 ANDERSON CREEK PHARMACY, INC 6779 OVERHILLS RD SPRING LAKE NC 28390 9104976337 ANGIER DISCOUNT DRUG 253 N RALIEGH STREET ANGIER NC 27501 9196399623 ANSON PHARMACY INC 806 CAMDEN RD WADESBORO NC 28170 7046949358 APEX PHARMACY 904 W WILLIAMS ST APEX NC 27502 9196297146 ARCHDALE DRUG AT CORNERSTONE -

Participating Chain Pharmacies
PARTICIPATING CHAIN PHARMACIES A & P Pharmacy Discount Drug Mart Hy-Vee, Drug Town Network Pharmacy Shoppers Pharmacy ABCO Pharmacy Doc's Drugs Ingles Pharmacy Oncology Pharmacy Services Shoprite Pharmacy Acme Pharmacy Drug Emporium Integrity Healthcare Services P&C Food Market Shurfine Pharmacy Acme, Lucky, Osco, Sav-on Drug Fair Kare Pharmacy Pacmed Clinic Pharmacy Smith's Food & Drug Center Albertson's Pharmacy Duane Reade Kash N' Karry Pharmacy Pamida Pharmacy Snyder Drug Stores Allcare Pharmacy Eagle Pharmacy Kelsey Seybold Clinic Pharmacy Park Nicollet Pharmacy Southern Family Markets Ambulatory Pharmaceutical Services Edgehill Drugs Kerr Drug Pathmark Stadtlander Pharmacy Anchor Pharmacy Express, Thrift, Treasury Keystone Medicine Chest Payless Pharmacy Standard Drug Company Appletree Pharmacy Fagen Pharmacy King Kullen Pharmacy Pediatric Services of America Star Pharmacy Arrow Pharmacy Fairview Pharmacy Kinney Drug's Pharma-Card Statscript Pharmacy Aurora Pharmacy Family Care Pharmacy Kleins Supermarket Pharmacy Pharmacy Plus Steele's Pharmacy B J's Pharmacy Family Drug Klinck, Drug Barn Presbyterian Retail Pharmacy Stop & Shop Pharmacy Bakers Pharmacy Family Fare Klingensmith's Drug Price Chopper Pharmacy Super D Bartell Drugs Family Pharmacy Kmart Pharmacy Price Less Drug Super Food Mart Basha's United Drug Fedco Drug Knight Drugs Price Wise, Piggly Wiggly Super Fresh Pharmacy Bel Air Pharmacy Finast Pharmacy Kohlls Pharmacy Prime Med Pharmacy Super RX Pharmacy Big Bear Pharmacy Food 4 Less Pharmacy Kopp Drug Publix Pharmacy -
Your ASPE Guide to Health Care Coverage
HEALTHBENEFITPLAN ASPEASPE ACCIDENTANDSICKNESSPROGRAMFOREXCHANGES Your ASPE Guide to Health Care Coverage WWW.USDOS.SEVENCORNERS.COM AS PE ACCIDENT AND SICKNESS PROGRAM FOR EXCHANGES The United States Department of State (USDoS) is pleased to welcome you to the Accident and Sickness Program for Exchanges (ASPE) Health Benefit Plan. As an Exchange Participant, you receive a limited health care benefit plan designed by USDoS and administered by Seven Corners, Inc. This plan IS NOT an insurance policy. The ASPE is a self-funded, limited, health care benefit plan designed to pay covered medical expenses for eligible Exchange Participants. Covered medical expenses are subject to limitations, and pre-existing conditions are not covered. This guide is an overview of the health care benefits you are provided while serving on your USDoS funded program. It also explains how payments are made for your covered medical expenses. It is your responsibility to read and under - stand what medical expenses are covered and not covered by the ASPE health care benefit plan. 1 TABLE OF CONTENTS 3 INSIDE THE US: Quick Reference Guide 4 OUTSIDE THE US: Quick Reference Guide 5 Customer Service 6 USDoS WEBSITE: MyPlan 7 Eligibility 8 Identification Cards 9 Benefit Coverage 12 Benefit Exclusions 15 INSIDE THE US: Medical Provider Network 17 OUTSIDE THE US: Medical Network 18 INSIDE THE US: Pharmacy Program 20 OUTSIDE THE US: Prescription Drugs 22 Pharmacy Program Exclusions 23 Payment of Medical Bills 24 Coordination of Benefits 25 Glossary of Terms 29 Program Forms 2 I N S I D E T H E U S : Q U I C K R E F E R E N C E Life-threatening medical emergency Dial 911 from any telephone. -

Houchens Industries Jimmie Gipson 493 2.6E Bowling Green, Ky
SN TOP 75 SN TOP 75 2010 North American Food Retailers A=actual sales; E=estimated sales CORPORATE/ SALES IN $ BILLIONS; RANK COMPANY TOP EXECUTIVE(S) FRancHise STORes DATE FISCAL YEAR ENDS 1 Wal-Mart Stores MIKE DUKE 4,624 262.0E Bentonville, Ark. president, CEO 1/31/10 Volume total represents combined sales of Wal-Mart Supercenters, Wal-Mart discount stores, Sam’s Clubs, Neighborhood Markets and Marketside stores in the U.S. and Canada, which account for approximately 64% of total corporate sales (estimated at $409.4 billion in 2009). Wal-Mart operates 2,746 supercenters in the U.S. and 75 in Canada; 152 Neighborhood Markets and four Marketside stores in the U.S.; 803 discount stores in the U.S. and 239 in Canada; and 605 Sam’s Clubs in the U.S. (The six Sam’s Clubs in Canada closed last year, and 10 more Sam’s are scheduled to close in 2010.) 2 Kroger Co. DAVID B. DILLON 3,634 76.0E Cincinnati chairman, CEO 1/30/10 Kroger’s store base includes 2,469 supermarkets and multi-department stores; 773 convenience stores; and 392 fine jewelry stores. Sales from convenience stores account for approximately 5% of total volume, and sales from fine jewelry stores account for less than 1% of total volume. The company’s 850 supermarket fuel centers are no longer included in the store count. 3 Costco Wholesale Corp. JIM SINEGAL 527 71.4A Issaquah, Wash. president, CEO 8/30/09 Revenues at Costco include sales of $69.9 billion and membership fees of $1.5 billion. -
Health Options Program
Pennsylvania Public School Participating Employees’ Retirement System (PSERS) Pharmacy Directory Health FOR THE BASIC AND ENHANCED MEDICARE Rx OPTIONS This booklet provides a list of the Options HOP Basic and Enhanced Medicare Rx Plan participating network Program pharmacies. This directory is current as of January 1, 2009. Pharmacies may have been added or removed GEORGIA 2009 from the list after this directory was printed. Therefore, all network pharmacies may not be listed in this directory and the fact that the pharmacy is listed in the directory does not guarantee that the pharmacy is still in the network. To get current information about participating network pharmacies in your area, please visit the HOP Web site at www.HOPbenefits.com or contact Prescription Solutions Customer Service at (888) 239-1301, 24 hours a day, 7 days a week. (TTY/TDD users should call (800) 498-5428.) Introduction pharmacy or through our mail-order pharmacy This booklet provides a list of participating HOP service. Once you go to a particular pharmacy, Basic and Enhanced Medicare Rx Plan network you are not required to continue going to the pharmacies and includes some basic information same pharmacy to fill future prescriptions; you about how to best utilize the pharmacy network can go to any of our network pharmacies. to have your prescriptions filled. A complete We will reimburse beneficiaries for covered description of your prescription drug coverage, prescriptions filled at non-network pharmacies including how to have your prescriptions under certain circumstances as described later. filled, is included in the 2009 Annual Notice of Change and Evidence of Coverage document. -

Script Care Ltd. Participating Chain Pharmacies
SCRIPT CARE LTD. PARTICIPATING CHAIN PHARMACIES A & P Pharmacy Drug Emporium Kare Pharmacy Park Nicollet Pharmacy Shurfine Pharmacy ABCO Pharmacy Drug Fair Kash N' Karry Pharmacy Pathmark Smith's Food & Drug Center Acme Pharmacy Duane Reade Kelsey Seybold Clinic Pharmacy Payless Pharmacy Snyder Drug Stores Acme, Lucky, Osco, Sav-on Eagle Pharmacy Kerr Drug Pediatric Services of America Southern Family Markets Albertson's Pharmacy Edgehill Drugs Keystone Medicine Chest PharmacPhar-Mor Stadtlander Pharmacy Allcare Pharmacy Express, Thrift, Treasury King Kullen Pharmacy Pharma-Card Standard Drug Company Ambulatory Pharmaceutical ServiceFagen Pharmacy Kinney Drug's Pharmaca Integrative Pharmacy Star Pharmacy Anchor Pharmacy Fairview Pharmacy Kleins Supermarket Pharmacy Pharmacy Plus Statscript Pharmacy Appletree Pharmacy Family Care Pharmacy Klinck, Drug Barn Presbyterian Retail Pharmacy Steele's Pharmacy Arrow Pharmacy Family Drug Klingensmith's Drug Price Chopper Pharmacy Stop & Shop Pharmacy Aurora Pharmacy Family Fare Kmart Pharmacy Price Less Drug Super D B J's Pharmacy Family Pharmacy Knight Drugs Price Wise, Piggly Wiggly Super Food Mart Bakers Pharmacy Fedco Drug Kohlls Pharmacy Prime Med Pharmacy Super Fresh Pharmacy Bartell Drugs Finast Pharmacy Kopp Drug Publix Pharmacy Super RX Pharmacy Basha's United Drug Food 4 Less Pharmacy Kroger Pharmacy QFC Pharmacy Super Sav-On-Drug's Bel Air Pharmacy Food City Pharmacy Lewis Drugs Quality Pharmacy Supersaver Pharmacy, Sentry Drug Bi-Lo Pharmacy Food Lion Pharmacy Lifecheck Drug Quick Chek -
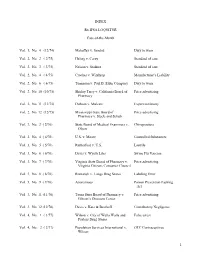
INDEX Rx IPSA LOQUITUR Case-Of-The-Month Vol. 1, No. 4
INDEX Rx IPSA LOQUITUR Case-of-the-Month Vol. 1, No. 4 (12/74) Mahaffey v. Sandoz Duty to warn Vol. 2, No. 2 ( 2/75) Heling v. Carey Standard of care Vol. 2, No. 3 ( 3/75) Nelson v. Stadner Standard of care Vol. 2, No. 4 ( 4/75) Crocker v. Winthrop Manufacturer’s Liability Vol. 2, No. 6 ( 6/75) Tonneson v. Paul B. Elder Company Duty to warn Vol. 2, No. 10 (10/75) Shirley Terry v. California Board of Price advertising Pharmacy Vol. 2, No. 11 (11/75) Dobson v. Mulcare Expert testimony Vol. 2, No. 12 (12/75) Mississippi State Board of Price advertising Pharmacy v. Steele and Schub Vol. 3, No. 2 ( 2/76) State Board of Medical Examiners v. Chiropractors Olson Vol. 3, No. 4 ( 4/76) U.S. v. Moore Controlled Substances Vol. 3, No. 5 ( 5/76) Rutherford v. U.S. Laetrile Vol. 3, No. 6 ( 6/76) Davis v. Wyeth Labs Swine Flu Vaccine Vol. 3, No. 7 ( 7/76) Virginia State Board of Pharmacy v. Price advertising Virginia Citizens Consumer Council Vol. 3, No. 8 ( 8/76) Romanyk v. Longs Drug Stores Labeling Error Vol. 3, No. 9 ( 9/76) Anonymous Poison Prevention Packing Act Vol. 3, No. 11 (11/76) Texas State Board of Pharmacy v. Price advertising Gibson’s Discount Center Vol. 3, No. 12 (12/76) Davis v. Katz & Besthoff Contributory Negligence Vol. 4, No. 1 ( 1/77) Wilson v. City of Walla Walla and False arrest Payless Drug Stores Vol. 4, No. 2 ( 2/77) Population Services International v. -

Newsfood Trade
▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ WorldFood Food Trade NewsWWW.FOODTRADENEWS.COM 20 21 MEDIA KIT ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ WorldFood CONTACTS Food Trade NewsWWW.FOODTRADENEWS.COM FOOD WORLD/FOOD TRADE NEWS p: 410.730.5013 f: 410.740.4680 e: [email protected] Jeffrey W. Metzger Publisher p: 410.730.5013 e: [email protected] Terri Maloney Vice President/Editorial Director p: 410.730.5013 e: [email protected] Maria Maggio Vice President/General Manager, Food Trade News p: 443.631.0172 e: [email protected] Kevin Gallagher Vice President p: 201.250.2217 e: [email protected] Karen T. Fernandez Director, Sales & Marketing p: 443.765.1575 e: [email protected] Beth Pripstein Circulation Manager p: 410.730.5013 e: [email protected] ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ WorldFood COVERAGE MAP Food Trade NewsWWW.FOODTRADENEWS.COM Out of Region Companies Receiving FOOD WORLD & FOOD TRADE NEWS: Ahold Delhaize, Amsterdam, The Netherlands Albertsons Companies, Boise, ID Aldi, Batavia, IL Amazon, Seattle, WA Costco, Issaquah, WA Grocery Outlet, Emeryville, CA Kroger, Cincinnati, OH Sam’s Club, Bentonville, AR Save-A-Lot, St. Ann, MO Sprouts, Phoenix, AZ Target, Minneapolis, MN Trader Joe’s, Monrovia, CA Wal-Mart, Bentonville, AR Walgreens, Deerfield, IL Whole Foods, Austin, TX 7-Eleven, Dallas, TX EDITORIAL OPPORTUNITIES Feature Stories New Bakery & Production Facility Helps Accelerates Crest Hill’s Growth stallations, Koita made the decision to expand to Mustafa Koita Is A Man On A Mission the- U.S.A onMilk a much broader Mission level. Crest Hill Bakery, the fast-growing artisan maker based in Glenn Dale, MD, has craft ed a formula for success: produce high Until he was almost 40, nothing in Mustafa Koi- “Truthfully, it was a painful experience,” he not- quality European hearth baked breads and sell them to retail and ta’s career path would indicate a love and passion ed about the bureaucratic procedure of getting the for the milk business. -

Monitoring and Assessing the Impact of Tax and Price Policies on United States’ Tobacco Use
MONITORING AND ASSESSING THE IMPACT OF TAX AND PRICE POLICIES ON UNITED STATES’ TOBACCO USE Frank J. Chaloupka, Ph.D. University of Illinois at Chicago U01 Advisory Panel Meeting, May 1st 2012, Chicago, Illinois Elizabeth Ginexi STATE AND COMMUNITY TOBACCO CONTROL RESEARCH INITIATIVE BACKGROUND FOR SCTC RESEARCH INITIATIVE Community and social norms favoring tobacco-free lifestyles vary greatly across populations. States and communities have played an important role in implementing tobacco prevention and control policies and programs, as well as in designing and implementing mass media campaigns. Significant knowledge gaps exist about how to best strengthen and reinforce tobacco-free social norms across diverse communities and counteract competing pro-tobacco norms. PURPOSE OF SCTC RESEARCH INITIATIVE NCI established the SCTC Research Initiative in 2009 to address high-priority research gaps in state and community tobacco control research: o Secondhand smoke policies o Tax and pricing policies o Mass media countermeasures and community and social norms o Tobacco industry marketing and promotion PROJECT STRUCTURE FOR SCTC RESEARCH COLLABORATION COORDINATING CENTER FOR THE ADVANCEMENT OF TOBACCO CONTROL RESEARCH AND PRACTICE Research Triangle Institute (RTI) Staff: Carol Schmitt, Project Director; Todd Rogers, Associate Project Director; and Matthew Farrelly, Senior Advisor Role: • Increase scientific and organizational leadership necessary to facilitate interactive and integrative collaboration and communication of the research projects funded by this initiative. Specific Aims: Foster collaboration and communication among research project sites, NCI and the broader public health community. Collaborate with NCI, the Steering Committee and research project sites to identify and facilitate complementary, cross- site developmental research projects. Develop plans for translation and dissemination activities and site-specific and initiative-wide evaluation plans. -

Bake Locall , Wante Everywher
▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲ ▲▲ ▲ ▲ ▲ ▲ ▲ ▲ INSIDE ▲ TAKING THIS ISSUE STOCK by Jeff Metzger Food Trade Jim Donald: We Hardly Knew Ye That Jim Donald will be stepping down as CEO of Albertsons on April Allegiance/PSK Revive 25, seven months after he accepted the position and 13 months after Pathmark Banner With he rejoined the large Boise, ID-based retailer after 27 years, shouldn’t be New Brooklyn, NY Unit surprising. 30 After all, the catalyst for Donald to come back to Albertsons in March 2018 was Bob Miller, then chief executive of the supermarket chain and one of the greatest leaders in the supermarket business of the past 50 years. In the nearly 30 years that I’ve known Jim, he has often mentioned that he’s learned more from Miller (now chairman emeritus) about the grocery business than anybody else. Jim considers him a mentor. So, as Albertsons began the process of attempting to complete a Price Rite Marketplace A PUBLICATION OF BEST-MET PUBLISHING, INC. merger with Rite Aid, Miller called on his old protégé to help run Albert- Revamps Five Discount Supermarkets In CT NVOL. 75 NO. 4 ewsSPECIALTY FOODS ISSUE APRIL 2019 See TAKING STOCK on page 6 32 Donald To Become Co-Chairman Of Large Chain Acme Bullish On ‘19 Initiatives; Sankaran Is Albertsons New CEO It’s been a busy month at Alb- mately 250 suppliers, brokers and weeks. Those stores that will be ertsons, which announced that distributors, was president Jim upgraded are located in: Newark, Jim Donald will be leaving his Perkins. The veteran Albertsons DE; Smyrna, DE; Ogletown, DE; post as president and chief execu- executive, who began with the re- Pike Creek, DE; Mount Freedom, tive April 25 to become co-chair- tailer in 1982 and also serves as a NJ; Woodbury, NJ; Freehold, NJ; man of the company. -

Robert J. Desalvo Papers Business Combinations in the Cosmetic and Pharmaceutical Industries 1944
Robert J. DeSalvo Papers Business Combinations in the Cosmetic and Pharmaceutical Industries 1944 - 1990 Collection #107 Abstract Robert J. DeSalvo’s research focused on business combinations (acquisitions, mergers, and joint ventures in the cosmetic and pharmaceutical industries. This topic was the basis for his master’s thesis in pharmacy administration at the University of Pittsburgh and continued as a life-long interest. This collection consists of two series of notebooks that Dr. DeSalvo developed to record relevant business combinations. The first series records acquisitions, proposed acquisitions, mergers, and joint ventures for the period of 1944 –1990 in an alphabetical arrangement. The information on these entries is cumulative so that the history of an organization is collected in one place. The second series of notebooks is arranged in chronological blocks. The information is arranged alphabetically by the name of the acquirer. The name of the acquired (merged), type of combination (acquisition, proposed acquisition, joint venture) and the date is also provided. The information is cross-referenced between the two series so that the researcher can approach the information by the name of the parent company or chronologically. Dr. DeSalvo used this resource for many of his publications as well as his master’s thesis. A copy of these publications and his thesis make up the remainder of the collection. Donor Gift of Barbara DeSalvo, 2000 Biography Robert James DeSalvo was born on July 20, 1933 in Toledo, OH. He died on January 23, 1993 in Cincinnati, OH. DeSalvo graduated from high school in Toledo and attended pharmacy school at the University of Toledo where he received his B.S. -

Your Benefits Card Merchant List
Your Benefits Card Merchant List ¾ Use your benefits card at these stores that can identify FSA/HRA eligible expenses. ¾ Check the list to find your store before you order prescriptions or shop for over-the- counter (OTC) items. ¾ Swipe your benefits card first and only your FSA/HRA eligible purchases will be deducted from your account. ¾ You won’t have to submit receipts to verify purchases from these stores, but you should still save your receipts for easy reference. ¾ Merchants have the option of accepting MasterCard and/or Visa for payment. Before making a purchase with your benefits card, please make sure you know which cards are accepted. Ist America Prescription Drugs* Albertville Discount Pharmacy* AmiCare Pharmacy Inc* 3C Healthcare Inc, dba Medicap Alden Pharmacy* Anderson and Haile Drug Store* Pharmacy* Alert Pharmacy Services-Mt Anderson County Discount 50 Plus Pharmacy* Holly* Pharmacy* A & P* Alexandria Drugs Inc* Anderson Drug-Athens TX* Aasen Drug* Alfor’s Pharmacy* Anderson Pharmacy-Denver PA Abeldt’s Gaslight Pharmacy* Allcare Pharmacy* Anderson Pharmacy/John M* ACME * Allen Drug* Anderson’s Pharmacy* Acres Market (UT) * Allen’s Discount Pharmacy* Andrews Pharmacy* Acton Pharmacy Allen Family Drug* Anthony Brown Pharmacy Inc* Adams Pharmacy* Allen’s Foodmart* Antwerp Pharmacy* Adams Pharmacy Inc* Allen’s of Hastings, Inc.* Apotek Inc. Adams Pharmacy and Home Allen's Super Save #1 Provo Apotek Pharmacy* Care* UT* Apoteka Compounding LLC* Adamsville Pharmacy* Allen's Super Save #2 Orem UT* Apothecare Pharmacy* Adrien Pharmacy*