Docosahexaenoic Acid
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fatty Acid Diets: Regulation of Gut Microbiota Composition and Obesity and Its Related Metabolic Dysbiosis
International Journal of Molecular Sciences Review Fatty Acid Diets: Regulation of Gut Microbiota Composition and Obesity and Its Related Metabolic Dysbiosis David Johane Machate 1, Priscila Silva Figueiredo 2 , Gabriela Marcelino 2 , Rita de Cássia Avellaneda Guimarães 2,*, Priscila Aiko Hiane 2 , Danielle Bogo 2, Verônica Assalin Zorgetto Pinheiro 2, Lincoln Carlos Silva de Oliveira 3 and Arnildo Pott 1 1 Graduate Program in Biotechnology and Biodiversity in the Central-West Region of Brazil, Federal University of Mato Grosso do Sul, Campo Grande 79079-900, Brazil; [email protected] (D.J.M.); [email protected] (A.P.) 2 Graduate Program in Health and Development in the Central-West Region of Brazil, Federal University of Mato Grosso do Sul, Campo Grande 79079-900, Brazil; pri.fi[email protected] (P.S.F.); [email protected] (G.M.); [email protected] (P.A.H.); [email protected] (D.B.); [email protected] (V.A.Z.P.) 3 Chemistry Institute, Federal University of Mato Grosso do Sul, Campo Grande 79079-900, Brazil; [email protected] * Correspondence: [email protected]; Tel.: +55-67-3345-7416 Received: 9 March 2020; Accepted: 27 March 2020; Published: 8 June 2020 Abstract: Long-term high-fat dietary intake plays a crucial role in the composition of gut microbiota in animal models and human subjects, which affect directly short-chain fatty acid (SCFA) production and host health. This review aims to highlight the interplay of fatty acid (FA) intake and gut microbiota composition and its interaction with hosts in health promotion and obesity prevention and its related metabolic dysbiosis. -

Omega-3 Eicosapentaenoic Acid (EPA)
nutrients Article Omega-3 Eicosapentaenoic Acid (EPA) Rich Extract from the Microalga Nannochloropsis Decreases Cholesterol in Healthy Individuals: A Double-Blind, Randomized, Placebo-Controlled, Three-Month Supplementation Study Amanda Rao 1,2 , David Briskey 1,3, Jakob O Nalley 4 and Eneko Ganuza 4,* 1 RDC Clinical, Brisbane 4006, Australia; [email protected] (A.R.); [email protected] (D.B.) 2 School of Medicine, University of Sydney, Sydney, NSW 2006, Australia 3 School of Human Movement and Nutrition Sciences, The University of Queensland, Brisbane, QLD 4067, Australia 4 Qualitas Health, Houston, TX 77056, USA; [email protected] * Correspondence: [email protected] Received: 26 May 2020; Accepted: 20 June 2020; Published: 23 June 2020 Abstract: The aim of this trial is to assess the effect of Almega®PL on improving the Omega-3 Index, cardio-metabolic parameters, and other biomarkers in generally healthy individuals. The benefits of long-chain omega-3 fatty acids for cardiovascular health are primarily built upon mixtures of docosahexaenoic (DHA) and eicosapentaenoic acids (EPA). Highly purified EPA therapy has proven to be particularly effective in the treatment of cardiovascular disease, but less is known about the benefits of EPA-only supplementation for the general healthy population. Almega®PL is a polar rich oil (>15%) derived from the microalga Nannochloropsis that contains EPA (>25%) with no DHA. Participants (n = 120) were given a capsule of 1 g/day of either Almega®PL or placebo for 12 weeks. Differences in the Omega-3 Index, cardiometabolic markers, and other general health indicators were measured at the baseline, six, and 12 weeks. -

Pathway Development Via Retinoid X Receptor Vitamin a Enhances In
Vitamin A Enhances in Vitro Th2 Development Via Retinoid X Receptor Pathway This information is current as Charles B. Stephensen, Reuven Rasooly, Xiaowen Jiang, of September 24, 2021. Michael A. Ceddia, Casey T. Weaver, Roshantha A. S. Chandraratna and R. Patterson Bucy J Immunol 2002; 168:4495-4503; ; doi: 10.4049/jimmunol.168.9.4495 http://www.jimmunol.org/content/168/9/4495 Downloaded from References This article cites 40 articles, 24 of which you can access for free at: http://www.jimmunol.org/content/168/9/4495.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 24, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2002 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Vitamin A Enhances in Vitro Th2 Development Via Retinoid X Receptor Pathway1 Charles B. Stephensen,2* Reuven Rasooly,* Xiaowen Jiang,* Michael A. Ceddia,3* Casey T. Weaver,† Roshantha A. S. Chandraratna,‡ and R. Patterson Bucy† Vitamin A deficiency diminishes Th2-mediated Ab responses, and high-level dietary vitamin A or treatment with the vitamin A metabolite retinoic acid (RA) enhances such responses. -

TAZORAC® (Tazarotene) Gel 0.05% (Tazarotene) Gel 0.1%
NDA 020600 ® TAZORAC (tazarotene) Gel 0.05% (tazarotene) Gel 0.1% FOR DERMATOLOGIC USE ONLY NOT FOR OPHTHALMIC, ORAL, OR INTRAVAGINAL USE DESCRIPTION TAZORAC® Gel is a translucent, aqueous gel and contains the compound tazarotene, a member of the acetylenic class of retinoids. It is for topical dermatologic use only. The active ingredient is represented by the following structural formula: O OCH2CH3 N S TAZAROTENE C21H21NO2S Molecular Weight: 351.46 Chemical Name: Ethyl 6-[(4,4-dimethylthiochroman-6-yl)ethynyl]nicotinate Contains: Active: Tazarotene 0.05% or 0.1% (w/w) Preservative: Benzyl alcohol 1% (w/w) Inactives: Ascorbic acid, butylated hydroxyanisole, butylated hydroxytoluene, carbomer 934P, edetate disodium, hexylene glycol, poloxamer 407, polyethylene glycol 400, polysorbate 40, purified water, and tromethamine. CLINICAL PHARMACOLOGY Tazarotene is a retinoid prodrug which is converted to its active form, the cognate carboxylic acid of tazarotene (AGN 190299), by rapid deesterification in animals and man. AGN 190299 (“tazarotenic acid”) binds to all three members of the retinoic acid receptor (RAR) family: RARα, RARβ, and RARγ but shows relative selectivity for RARβ, and RARγ and may modify gene expression. The clinical significance of these findings is unknown. Psoriasis: The mechanism of tazarotene action in psoriasis is not defined. Topical tazarotene blocks induction of mouse epidermal ornithine decarboxylase (ODC) activity, which is associated with cell proliferation and hyperplasia. In cell culture and in vitro models of skin, tazarotene suppresses expression of MRP8, a marker of inflammation present in the epidermis of psoriasis patients at high levels. In human keratinocyte cultures, it inhibits cornified envelope formation, whose build-up is an element of the psoriatic scale. -

Compounds with Anti-Aging Activities
(19) TZZ ZZ_T (11) EP 2 862 600 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 22.04.2015 Bulletin 2015/17 A61Q 19/08 (2006.01) A61K 8/49 (2006.01) A61K 8/36 (2006.01) A61K 8/44 (2006.01) (2006.01) (2006.01) (21) Application number: 14196664.8 A61K 8/63 A61K 8/64 A61K 8/33 (2006.01) A61K 8/60 (2006.01) (2006.01) (2006.01) (22) Date of filing: 20.12.2011 A61Q 17/04 A61K 8/42 A61Q 1/02 (2006.01) A61Q 19/00 (2006.01) A61Q 19/02 (2006.01) A61Q 19/04 (2006.01) A61Q 19/10 (2006.01) A61K 31/11 (2006.01) A61K 31/197 (2006.01) A61K 31/202 (2006.01) A61K 31/343 (2006.01) A61K 31/353 (2006.01) A61K 31/704 (2006.01) (84) Designated Contracting States: • Mavon, Alain Robert Pierre AL AT BE BG CH CY CZ DE DK EE ES FI FR GB 11264 Stockholm (SE) GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO • Duracher, Lucie PL PT RO RS SE SI SK SM TR 11761 Stockholm (SE) Designated Extension States: • Klack, Anke BA ME 11244 Stockholm (SE) • Cattley, Kevin (62) Document number(s) of the earlier application(s) in Wexford (IE) accordance with Art. 76 EPC: 11797020.2 / 2 729 220 (74) Representative: Moore, Michael Richard et al Keltie LLP (71) Applicant: Oriflame Research and Development No.1 London Bridge Ltd. London SE1 9BA (GB) Bray, Co. Wicklow (IE) Remarks: (72) Inventors: This application was filed on 05-12-2014 as a • Gillbro, Johanna Maria divisional application to the application mentioned 11736 Stockholm (SE) under INID code 62. -

Oxidation of Retinol to Retinoic Acid As a Requirement for Biological Activity in Mouse Epidermis1
[CANCER RESEARCH 48, 7038-7040, December 15, 1988] Oxidation of Retinol to Retinoic Acid as a Requirement for Biological Activity in Mouse Epidermis1 Michael J. Connor Division of Dermatology, Department of Medicine, UCLA School of Medicine, Los Angeles, California 90024 ABSTRACT of retinal, which may explain its ability to inhibit both steps in The food and fragrance additive citral (3,7-dimethyl-2,6-octadienal) retinoic acid synthesis from retinol, since as an aldehyde it can inhibits the oxidation of retino! to retinole acid in mouse epidermis on act as a substrate for both the alcohol- and aldehyde-dehydro- local application. This inhibitory property was used to test the hypothesis genases involved. that oxidation to retinole acid is rate limiting for the biological activity The ability of citral to inhibit retinol oxidation provides an of vitamin A (retinol) in epithelial tissues. Citral was tested as a modulator experimental tool for testing the paradigm that retinoic acid is of the biological activities of retinol and retinole acid using two bioassays an obligatory intermediate in at least some aspects of vitamin performed in Skh.hrI (hairless) mice: (a) the ability to induce epidermal A activity in the epithelia in vivo. Citral was proposed as a hyperplasia; (/>)the ability to inhibit the induction of epidermal ornithine vitamin A antagonist in 1956 (7). Aydelotte (8, 9) studied the decarboxylase activity by tumor promoters. Citral treatment inhibited interaction of citral and retinol in whole organ cultures of chick the ability of retinol, but not of retinoic acid, to induce epidermal epithelial tissues and concluded that citral had a competitive hyperplasia. -
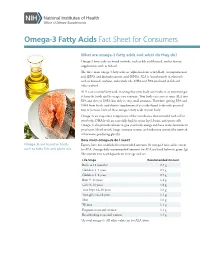
Omega-3 Fatty Acids Fact Sheet for Consumers
Omega-3 Fatty Acids Fact Sheet for Consumers What are omega-3 fatty acids and what do they do? Omega-3 fatty acids are found in foods, such as fish and flaxseed, and in dietary supplements, such as fish oil. The three main omega-3 fatty acids are alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). ALA is found mainly in plant oils such as flaxseed, soybean, and canola oils. DHA and EPA are found in fish and other seafood. ALA is an essential fatty acid, meaning that your body can’t make it, so you must get it from the foods and beverages you consume. Your body can convert some ALA into EPA and then to DHA, but only in very small amounts. Therefore, getting EPA and DHA from foods (and dietary supplements if you take them) is the only practical way to increase levels of these omega-3 fatty acids in your body. Omega-3s are important components of the membranes that surround each cell in your body. DHA levels are especially high in retina (eye), brain, and sperm cells. Omega-3s also provide calories to give your body energy and have many functions in your heart, blood vessels, lungs, immune system, and endocrine system (the network of hormone-producing glands). How much omega-3s do I need? Omega-3s are found in foods Experts have not established recommended amounts for omega-3 fatty acids, except such as fatty fish and plant oils. for ALA. Average daily recommended amounts for ALA are listed below in grams (g). -

Revealing the Role of Short Chain and Polyunsaturated Fatty Acids As
Southern Illinois University Carbondale OpenSIUC Honors Theses University Honors Program 2019 Revealing the Role of Short Chain and Polyunsaturated Fatty Acids as Regulators of Metabolic Activity and Gene Expression in Ovarian Cancer Abigayle Ochs [email protected] Follow this and additional works at: https://opensiuc.lib.siu.edu/uhp_theses Recommended Citation Ochs, Abigayle, "Revealing the Role of Short Chain and Polyunsaturated Fatty Acids as Regulators of Metabolic Activity and Gene Expression in Ovarian Cancer" (2019). Honors Theses. 461. https://opensiuc.lib.siu.edu/uhp_theses/461 This Dissertation/Thesis is brought to you for free and open access by the University Honors Program at OpenSIUC. It has been accepted for inclusion in Honors Theses by an authorized administrator of OpenSIUC. For more information, please contact [email protected]. REVEALING THE ROLE OF SHORT CHAIN AND POLYUNSATURATED FATTY ACIDS AS REGULATORS OF METABOLIC ACTIVITY AND GENE EXPRESSION IN OVARIAN CANCER Abigayle Ochs A thesis submitted to the University Honors Program in partial fulfillment of the requirements for the Honors Certificate with Thesis Southern Illinois University Carbondale May 2019 Ochs 2 I. Abstract Previous research using the chicken model has provided evidence that a flaxseed- supplemented diet decreases both the severity and the incidence of ovarian cancer. Flaxseed is a source of omega-3 (OM3) polyunsaturated fatty acids (PUFA), particularly α-linolenic acid (ALA). ALA is converted into longer chain OM3s, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which inhibit prostaglandins, thereby inhibiting oxidative stress, inflammation, angiogenesis, and proliferation. The dietary fiber component of flaxseed can be fermented in the gut to produce short chain fatty acids (SCFA). -

Omega-3, Omega-6 and Omega-9 Fatty Acids
Johnson and Bradford, J Glycomics Lipidomics 2014, 4:4 DOI: 0.4172/2153-0637.1000123 Journal of Glycomics & Lipidomics Review Article Open Access Omega-3, Omega-6 and Omega-9 Fatty Acids: Implications for Cardiovascular and Other Diseases Melissa Johnson1* and Chastity Bradford2 1College of Agriculture, Environment and Nutrition Sciences, Tuskegee University, Tuskegee, Alabama, USA 2Department of Biology, Tuskegee University, Tuskegee, Alabama, USA Abstract The relationship between diet and disease has long been established, with epidemiological and clinical evidence affirming the role of certain dietary fatty acid classes in disease pathogenesis. Within the same class, different fatty acids may exhibit beneficial or deleterious effects, with implications on disease progression or prevention. In conjunction with other fatty acids and lipids, the omega-3, -6 and -9 fatty acids make up the lipidome, and with the conversion and storage of excess carbohydrates into fats, transcendence of the glycome into the lipidome occurs. The essential omega-3 fatty acids are typically associated with initiating anti-inflammatory responses, while omega-6 fatty acids are associated with pro-inflammatory responses. Non-essential, omega-9 fatty acids serve as necessary components for other metabolic pathways, which may affect disease risk. These fatty acids which act as independent, yet synergistic lipid moieties that interact with other biomolecules within the cellular ecosystem epitomize the critical role of these fatty acids in homeostasis and overall health. This review focuses on the functional roles and potential mechanisms of omega-3, omega-6 and omega-9 fatty acids in regard to inflammation and disease pathogenesis. A particular emphasis is placed on cardiovascular disease, the leading cause of morbidity and mortality in the United States. -

Breast Milk Docosahexaenoic Acid (DHA) Correlates with DHA Status Of
Arch Dis Child 2000;82:493–494 493 Breast milk docosahexaenoic acid (DHA) correlates Arch Dis Child: first published as 10.1136/adc.82.6.493 on 1 June 2000. Downloaded from with DHA status of malnourished infants Ella N Smit, Esther A Oelen, Ejaz Seerat, Frits A J Muskiet, E Rudy Boersma Abstract ished, mostly breast fed, 4–56 month old chil- Aim—To investigate whether low docosa- dren, living in and around Islamabad, North hexaenoic acid (22:6ù3; DHA) status of Pakistan.3 malnourished, mostly breast fed infants is We hypothesised that the low RBC DHA a result of low ù3 fatty acid intake via content in these infants was a result of low breast milk. ù3-LCPUFA intake via breast milk. In an Methods—Fatty acid composition of attempt to test this hypothesis we studied the breast milk of eight Pakistani mothers, FA composition of both the breast milk of eight and of the erythrocytes of their malnour- Pakistani mothers and that of the RBC of their ished children was analysed. malnourished children. Results—The milk of the Pakistani moth- ers contained low percentages of all ù3 Subjects and methods and most ù6 fatty acids, compared with The study population consisted of eight milk of Dutch mothers. Breast milk DHA mother–child pairs from a low socioeconomic was positively correlated with infant class. They were recruited from the Nutrition erythrocyte DHA and arachidonic acid Rehabilitation Center of the Pediatric Depart- (20:4ù6). ment, Federal Government Services Hospital, Conclusion—DHA status of these mal- Islamabad. The children were classified as nourished children is strongly dependent malnourished, defined as weight for age below on the ù3 fatty acid intake from breast the mean minus 2SD, according to WHO milk. -

Vitamins and Healthy Skin Zoe Diana Draelos, MD
COSMETIC CONSULTATION Vitamins and Healthy Skin Zoe Diana Draelos, MD he term nutricosmetic combines the words nutri- to prevent vitamin D deficiency.1 Vitamin D deficiency, tion and cosmetic. Many of the new food intro- the cause of rickets in children, was virtually eliminated T ductions at the grocery store are nutricosmetics. when milk was enriched with 400 IU vitamin D per quart For example, milk is enriched with vitamin D whereas in the 1930s. One cup of milk supplies 25% of the recom- yogurt is not. However, a new line of yogurt contains mended daily allowance of vitamin D in adults; however, both vitamin D and inulin, a nonabsorbable fiber to aid it is probable that the current recommended daily allow- elimination. A competing yogurt brand contains probiotic ances are too low.2 Two hundred IU are recommended organisms, which are bacteria designed to recolonize the daily from birth to age 50 years; 400 IU from age 51 to gut, resulting in improved elimination and better overall 70 years; and 600 IU from age 71 years and older.3 health from the inside out. Adding nutrients is an impor- It is important to recognize that only milk is enriched tant marketing tactic because it allows existing foods to with vitamin D. Cheese, yogurt, and ice cream are not be made new with the addition of one ingredient. An required to include vitamin D; however, a new trend in existing food with decreasing sales can be reinvigorated some nutricosmetic yogurts, mentioned previously, is to in the marketplace with littleCOS upfront cost. -

Bexarotene) Capsules, 75 Mg
1 PACKAGE INSERT Targretin® (bexarotene) capsules, 75 mg Rx only. Targretin® capsules are a member of the retinoid class of drugs that is associated with birth defects in humans. Targretin® capsules also caused birth defects when administered orally to pregnant rats. Targretin® capsules must not be administered to a pregnant woman. See CONTRAINDICATIONS. DESCRIPTION Targretin® (bexarotene) is a member of a subclass of retinoids that selectively activate retinoid X receptors (RXRs). These retinoid receptors have biologic activity distinct from that of retinoic acid receptors (RARs). Each soft gelatin capsule for oral administration contains 75 mg of bexarotene. The chemical name is 4-[1-(5,6,7,8-tetrahydro-3,5,5,8,8-pentamethyl-2- naphthalenyl) ethenyl] benzoic acid, and the structural formula is as follows: CH2 H3C CH3 CH3 COOH H3CCH3 Bexarotene is an off-white to white powder with a molecular weight of 348.48 and a molecular formula of C24H28O2. It is insoluble in water and slightly soluble in vegetable oils and ethanol, USP. Each Targretin® (bexarotene) capsule also contains the following inactive ingredients: polyethylene glycol 400, NF, polysorbate 20, NF, povidone, USP, and butylated hydroxyanisole, NF. The capsule shell contains gelatin, NF, sorbitol special-glycerin blend, and titanium dioxide, USP. CLINICAL PHARMACOLOGY Mechanism of Action Bexarotene selectively binds and activates retinoid X receptor subtypes (RXRα, RXRβ, RXRγ). RXRs can form heterodimers with various receptor partners such as retinoic acid receptors (RARs), vitamin D receptor, thyroid receptor, and peroxisome proliferator activator receptors (PPARs). Once activated, these receptors function as transcription factors that regulate the expression of genes that control cellular 2 differentiation and proliferation.