Ulnar Neuropathy at the Elbow, an Overview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dental Plexopathy Vesta Guzeviciene, Ricardas Kubilius, Gintautas Sabalys
SCIENTIFIC ARTICLES Stomatologija, Baltic Dental and Maxillofacial Journal, 5:44-47, 2003 Dental Plexopathy Vesta Guzeviciene, Ricardas Kubilius, Gintautas Sabalys SUMMARY Aim and purpose of the study were: 1) to study and compare unfavorable factors playing role in the development of upper teeth plexitis and upper teeth plexopathy; 2) to study peculiarities of clinical manifestation of upper teeth plexitis and upper teeth plexopathy, and to establish their diagnostic value; 3) to optimize the treatment. The results of examination and treatment of 79 patients with upper teeth plexitis (UTP-is) and 63 patients with upper teeth plexopathy (UTP-ty) are described in the article. Questions of the etiology, pathogenesis and differential diagnosis are discussed, methods of complex medicamental and surgical treatment are presented. Keywords: atypical facial neuralgia, atypical odontalgia, atypical facial pain, vascular toothache. PREFACE Besides the common clinical tests, in order to ana- lyze in detail the etiology and pathogenesis of the afore- Usually the injury of the trigeminal nerve is re- mentioned disease, its clinical manifestation and pecu- lated to the pathology of the teeth neural plexuses. liarities, we performed specific examinations such as According to the literature data, injury of the upper orthopantomography of the infraorbital canals, mea- teeth neural plexuses makes more than 7% of all sured the velocity of blood flow in the infraorbital blood neurostomatologic diseases. Many terms are used in vessels (doplerography), examined the pain threshold literature to characterize the clinical symptoms com- of facial skin and oral mucous membrane in acute pe- plex of the above-mentioned pathology. Some authors riod and remission, and evaluated the role that the state (1, 2, 3) named it dental plexalgia or dental plexitis. -

An Occupational Therapy Guide for Entry
University of North Dakota UND Scholarly Commons Occupational Therapy Capstones Department of Occupational Therapy 2008 An Occupational Therapy Guide for Entry-Level Therapists not Specializing in the Treatment of Upper Extremity Dysfunction: Three Common Cumulative Trauma Injuries Ryan Edwards University of North Dakota Follow this and additional works at: https://commons.und.edu/ot-grad Part of the Occupational Therapy Commons Recommended Citation Edwards, Ryan, "An Occupational Therapy Guide for Entry-Level Therapists not Specializing in the Treatment of Upper Extremity Dysfunction: Three Common Cumulative Trauma Injuries" (2008). Occupational Therapy Capstones. 57. https://commons.und.edu/ot-grad/57 This Scholarly Project is brought to you for free and open access by the Department of Occupational Therapy at UND Scholarly Commons. It has been accepted for inclusion in Occupational Therapy Capstones by an authorized administrator of UND Scholarly Commons. For more information, please contact [email protected]. AN OCCUPATIONAL THERAPY GUIDE FOR ENTRY-LEVEL THERAPISTS NOT SPECIALIZING IN THE TREATMENT OF UPPER EXTREMITY DYSFUNCTION: THREE COMMON CUMULATIVE TRAUMA INJURIES by Ryan Edwards Advisor: Anne Haskins PhD, OTR/L A Scholarly Project Submitted to the Occupational Therapy Department of the University of North Dakota In partial fulfillment of the requirements for the degree of Master’s of Occupational Therapy Grand Forks, North Dakota August 1, 2008 This Scholarly Project Paper, submitted by Ryan Edwards in partial fulfillment of the requirement for the Degree of Master’s of Occupational Therapy from the University of North Dakota, has been read by the Faculty Advisor under whom the work has been done and is hereby approved. -

Cubital Tunnel Syndrome
Cubital Tunnel Syndrome What many people call the “funny bone” really is a nerve. This ulnar nerve runs behind a bone in the elbow through a space Figure 1: Ulnar Nerve at elbow joint (inner side of elbow) called the “cubital tunnel” (Figure 1). Although “banging the funny bone” usually causes temporary symptoms, chronic pressure on or stretching of the nerve can affect the blood supply to the ulnar nerve, causing numbness or tingling in the ring and small fingers, pain in the forearm, and/or weakness in the hand. This is called “cubital tunnel syndrome.” Humerus Causes There are a few causes of this ulnar nerve problem. These include: Pressure. Because the nerve runs through that “funny bone” groove and has little padding over it, direct pressure (like leaning your arm on an arm rest) can compress the nerve, causing your arm and hand—especially the ring and small fingers—to Ulnar Nerve “fall asleep.” Stretch. Keeping the elbow bent for a long time can stretch Medial Epicondyle the nerve behind the elbow. This usually happens during sleep. Anatomy. Sometimes, the ulnar nerve does not stay in its place and snaps back and forth over a bony bump as the elbow is moved. Repetitive snapping can irritate the nerve. Sometimes, the soft tissues over the nerve become thicker or there is an Ulna “extra” muscle over the nerve that can keep the nerve from working correctly. Treatment Signs and Symptoms The first treatment is to avoid actions that cause symptoms. Cubital tunnel syndrome can cause pain, loss of sensation, Wrapping a pillow or towel around the elbow or wearing a splint and/or tingling. -

Musculoskeletal Ultrasound Technical Guidelines II. Elbow
European Society of MusculoSkeletal Radiology Musculoskeletal Ultrasound Technical Guidelines II. Elbow Ian Beggs, UK Stefano Bianchi, Switzerland Angel Bueno, Spain Michel Cohen, France Michel Court-Payen, Denmark Andrew Grainger, UK Franz Kainberger, Austria Andrea Klauser, Austria Carlo Martinoli, Italy Eugene McNally, UK Philip J. O’Connor, UK Philippe Peetrons, Belgium Monique Reijnierse, The Netherlands Philipp Remplik, Germany Enzo Silvestri, Italy Elbow Note The systematic scanning technique described below is only theoretical, considering the fact that the examination of the elbow is, for the most, focused to one quadrant only of the joint based on clinical findings. 1 ANTERIOR ELBOW For examination of the anterior elbow, the patient is seated facing the examiner with the elbow in an extension position over the table. The patient is asked to extend the elbow and supinate the fore- arm. A slight bending of the patient’s body toward the examined side makes full supination and as- sessment of the anterior compartment easier. Full elbow extension can be obtained by placing a pillow under the joint. Transverse US images are first obtained by sweeping the probe from approximately 5cm above to 5cm below the trochlea-ulna joint, a Pr perpendicular to the humeral shaft. Cranial US images of the supracondylar region reveal the superficial biceps and the deep brachialis mu- Br scles. Alongside and medial to these muscles, follow the brachial artery and the median nerve: * the nerve lies medially to the artery. * Legend: a, brachial artery; arrow, median nerve; arrowheads, distal biceps tendon; asterisks, articular cartilage of the Humerus humeral trochlea; Br, brachialis muscle; Pr, pronator muscle 2 distal biceps tendon: technique The distal biceps tendon is examined while keeping the patient’s forearm in maximal supination to bring the tendon insertion on the radial tuberosity into view. -

Brachial-Plexopathy.Pdf
Brachial Plexopathy, an overview Learning Objectives: The brachial plexus is the network of nerves that originate from cervical and upper thoracic nerve roots and eventually terminate as the named nerves that innervate the muscles and skin of the arm. Brachial plexopathies are not common in most practices, but a detailed knowledge of this plexus is important for distinguishing between brachial plexopathies, radiculopathies and mononeuropathies. It is impossible to write a paper on brachial plexopathies without addressing cervical radiculopathies and root avulsions as well. In this paper will review brachial plexus anatomy, clinical features of brachial plexopathies, differential diagnosis, specific nerve conduction techniques, appropriate protocols and case studies. The reader will gain insight to this uncommon nerve problem as well as the importance of the nerve conduction studies used to confirm the diagnosis of plexopathies. Anatomy of the Brachial Plexus: To assess the brachial plexus by localizing the lesion at the correct level, as well as the severity of the injury requires knowledge of the anatomy. An injury involves any condition that impairs the function of the brachial plexus. The plexus is derived of five roots, three trunks, two divisions, three cords, and five branches/nerves. Spinal roots join to form the spinal nerve. There are dorsal and ventral roots that emerge and carry motor and sensory fibers. Motor (efferent) carries messages from the brain and spinal cord to the peripheral nerves. This Dorsal Root Sensory (afferent) carries messages from the peripheral to the Ganglion is why spinal cord or both. A small ganglion containing cell bodies of sensory NCS’s sensory fibers lies on each posterior root. -

Cubital Tunnel Syndrome)
DISEASES & CONDITIONS Ulnar Nerve Entrapment at the Elbow (Cubital Tunnel Syndrome) Ulnar nerve entrapment occurs when the ulnar nerve in the arm becomes compressed or irritated. The ulnar nerve is one of the three main nerves in your arm. It travels from your neck down into your hand, and can be constricted in several places along the way, such as beneath the collarbone or at the wrist. The most common place for compression of the nerve is behind the inside part of the elbow. Ulnar nerve compression at the elbow is called "cubital tunnel syndrome." Numbness and tingling in the hand and fingers are common symptoms of cubital tunnel syndrome. In most cases, symptoms can be managed with conservative treatments like changes in activities and bracing. If conservative methods do not improve your symptoms, or if the nerve compression is causing muscle weakness or damage in your hand, your doctor may recommend surgery. This illustration of the bones in the shoulder, arm, and hand shows the path of the ulnar nerve. Reproduced from Mundanthanam GJ, Anderson RB, Day C: Ulnar nerve palsy. Orthopaedic Knowledge Online 2009. Accessed August 2011. Anatomy At the elbow, the ulnar nerve travels through a tunnel of tissue (the cubital tunnel) that runs under a bump of bone at the inside of your elbow. This bony bump is called the medial epicondyle. The spot where the nerve runs under the medial epicondyle is commonly referred to as the "funny bone." At the funny bone the nerve is close to your skin, and bumping it causes a shock-like feeling. -

Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies
Anatomical, Clinical, and Electrodiagnostic Features of Radial Neuropathies a, b Leo H. Wang, MD, PhD *, Michael D. Weiss, MD KEYWORDS Radial Posterior interosseous Neuropathy Electrodiagnostic study KEY POINTS The radial nerve subserves the extensor compartment of the arm. Radial nerve lesions are common because of the length and winding course of the nerve. The radial nerve is in direct contact with bone at the midpoint and distal third of the humerus, and therefore most vulnerable to compression or contusion from fractures. Electrodiagnostic studies are useful to localize and characterize the injury as axonal or demyelinating. Radial neuropathies at the midhumeral shaft tend to have good prognosis. INTRODUCTION The radial nerve is the principal nerve in the upper extremity that subserves the extensor compartments of the arm. It has a long and winding course rendering it vulnerable to injury. Radial neuropathies are commonly a consequence of acute trau- matic injury and only rarely caused by entrapment in the absence of such an injury. This article reviews the anatomy of the radial nerve, common sites of injury and their presentation, and the electrodiagnostic approach to localizing the lesion. ANATOMY OF THE RADIAL NERVE Course of the Radial Nerve The radial nerve subserves the extensors of the arms and fingers and the sensory nerves of the extensor surface of the arm.1–3 Because it serves the sensory and motor Disclosures: Dr Wang has no relevant disclosures. Dr Weiss is a consultant for CSL-Behring and a speaker for Grifols Inc. and Walgreens. He has research support from the Northeast ALS Consortium and ALS Therapy Alliance. -

Cubital Tunnel Syndrome
Cubital Tunnel Syndrome What is it? Signs and Symptoms Cubital tunnel syndrome is a condition brought on by Cubital tunnel syndrome symptoms usually include increased pressure on the ulnar nerve at the elbow. pain, numbness, and/or tingling. The numbness or There is a bump of bone on the inner portion of the tingling most often occurs in the ring and little fingers. elbow (medial epicondyle) under which the ulnar The symptoms are usually felt when there is pressure on nerve passes. This site is commonly called the “funny the nerve, such as sitting with the elbow on an arm rest, bone”(see Figure 1). At this site, the ulnar nerve lies or with repetitive elbow bending and straightening. directly next to the bone and is susceptible to pressure. Often symptoms will be felt when the elbow is held in a When the pressure on the nerve becomes great enough bent position for a period of time, such as when holding to disturb the way the nerve works, then numbness, the phone, or while sleeping. Some patients may notice tingling, and pain may be felt in the elbow, forearm, weakness while pinching, occasional clumsiness, and/ hand, and/or fingers. or a tendency to drop things. In severe cases, sensation may be lost and the muscles in the hand may lose bulk What causes it? and strength. Pressure on the ulnar nerve at the elbow can develop in several ways. The nerve is positioned right next to the bone and has very little padding over it, Figure 1: Ulner nerve at elbow joint (inner side of elbow) so pressure on this can put pressure on the nerve. -
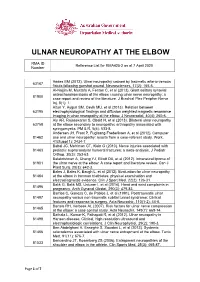
Reference List for RMA425-2 As at 7 April 2020 Number
ULNAR NEUROPATHY AT THE ELBOW RMA ID Reference List for RMA425-2 as at 7 April 2020 Number Addas BM (2012). Ulnar neuropathy caused by traumatic arterio-venous 63167 fistula following gunshot wound. Neurosciences, 17(2): 165-6. Al-Najjim M, Mustafa A, Fenton C, et al (2013). Giant solitary synovial osteochondromatosis of the elbow causing ulnar nerve neuropathy: a 81900 case report and review of the literature. J Brachial Plex Peripher Nerve Inj, 8(1): 1. Altun Y, Aygun SM, Cevik MU, et al (2013). Relation between 63195 electrophysiological findings and diffusion weighted magnetic resonance imaging in ulnar neuropathy at the elbow. J Neuroradiol, 40(4): 260-6. Aly AR, Rajasekaran S, Obaid H, et al (2013). Bilateral ulnar neuropathy 63758 at the elbow secondary to neuropathic arthropathy associated with syringomyelia. PM & R, 5(6): 533-8. Andersen JH, Frost P, Fuglsang-Frederiksen A, et al (2012). Computer 81462 use and ulnar neuropathy: results from a case-referent study. Work, 41(Suppl 1): 2434-7. Babal JC, Mehlman CT, Klein G (2010). Nerve injuries associated with 81463 pediatric supracondylar humeral fractures: a meta-analysis. J Pediatr Orthop, 30(3): 253-63. Balakrishnan A, Chang YJ, Elliott DA, et al (2012). Intraneural lipoma of 81901 the ulnar nerve at the elbow: A case report and literature review. Can J Plast Surg, 20(3): e42-3. Bales J, Bales K, Baugh L, et al (2012). Evaluation for ulnar neuropathy 81464 at the elbow in Ironman triathletes: physical examination and electrodiagnostic evidence. Clin J Sport Med, 22(2): 126-31. Balik G, Balik MS, Ustuner I, et al (2014). -

Perioperative Upper Extremity Peripheral Nerve Injury and Patient Positioning: What Anesthesiologists Need to Know
Anaesthesia & Critical Care Medicine Journal ISSN: 2577-4301 Perioperative Upper Extremity Peripheral Nerve Injury and Patient Positioning: What Anesthesiologists Need to Know Kamel I* and Huck E Review Article Lewis Katz School of Medicine at Temple University, USA Volume 4 Issue 3 Received Date: June 20, 2019 *Corresponding author: Ihab Kamel, Lewis Katz School of Medicine at Temple Published Date: August 01, 2019 University, MEHP 3401 N. Broad street, 3rd floor outpatient building ( Zone-B), DOI: 10.23880/accmj-16000155 Philadelphia, United States, Tel: 2158066599; Email: [email protected] Abstract Peripheral nerve injury is a rare but significant perioperative complication. Despite a variety of investigations that include observational, experimental, human cadaveric and animal studies, we have an incomplete understanding of the etiology of PPNI and the means to prevent it. In this article we reviewed current knowledge pertinent to perioperative upper extremity peripheral nerve injury and optimal intraoperative patient positioning. Keywords: Nerve Fibers; Proprioception; Perineurium; Epineurium; Endoneurium; Neurapraxia; Ulnar Neuropathy Abbreviations: PPNI: Perioperative Peripheral Nerve 2018.The most common perioperative peripheral nerve Injury; MAP: Mean Arterial Pressure; ASA CCP: American injuries involve the upper extremity with ulnar Society of Anesthesiology Closed Claims Project; SSEP: neuropathy and brachial plexus injury being the most Somato Sensory Evoked Potentials frequent [3,4]. In this article we review upper extremity PPNI with regards to anatomy and physiology, Introduction mechanisms of injury, risk factors, and prevention of upper extremity PPNI. Perioperative peripheral nerve injury (PPNI) is a rare complication with a reported incidence of 0.03-0.1% [1,2]. Anatomy and Physiology of Peripheral PPNI is a significant source of patient disability and is the Nerves second most common cause of anesthesia malpractice claims [3,4]. -

New Insights in Lumbosacral Plexopathy
New Insights in Lumbosacral Plexopathy Kerry H. Levin, MD Gérard Said, MD, FRCP P. James B. Dyck, MD Suraj A. Muley, MD Kurt A. Jaeckle, MD 2006 COURSE C AANEM 53rd Annual Meeting Washington, DC Copyright © October 2006 American Association of Neuromuscular & Electrodiagnostic Medicine 2621 Superior Drive NW Rochester, MN 55901 PRINTED BY JOHNSON PRINTING COMPANY, INC. C-ii New Insights in Lumbosacral Plexopathy Faculty Kerry H. Levin, MD P. James. B. Dyck, MD Vice-Chairman Associate Professor Department of Neurology Department of Neurology Head Mayo Clinic Section of Neuromuscular Disease/Electromyography Rochester, Minnesota Cleveland Clinic Dr. Dyck received his medical degree from the University of Minnesota Cleveland, Ohio School of Medicine, performed an internship at Virginia Mason Hospital Dr. Levin received his bachelor of arts degree and his medical degree from in Seattle, Washington, and a residency at Barnes Hospital and Washington Johns Hopkins University in Baltimore, Maryland. He then performed University in Saint Louis, Missouri. He then performed fellowships at a residency in internal medicine at the University of Chicago Hospitals, the Mayo Clinic in peripheral nerve and electromyography. He is cur- where he later became the chief resident in neurology. He is currently Vice- rently Associate Professor of Neurology at the Mayo Clinic. Dr. Dyck is chairman of the Department of Neurology and Head of the Section of a member of several professional societies, including the AANEM, the Neuromuscular Disease/Electromyography at Cleveland Clinic. Dr. Levin American Academy of Neurology, the Peripheral Nerve Society, and the is also a professor of medicine at the Cleveland Clinic College of Medicine American Neurological Association. -

Cubital Tunnel Syndrome: Diagnosis and Management Samir K
Cubital Tunnel Syndrome: Diagnosis and Management Samir K. Trehan, MD, John R. Parziale, MD, and Edward Akelman, MD CUB I TAL TU nn EL SY N DROME IS, AFTER C ARPAL During elbow flexion, the ulnar nerve Populations at risk for cubital tunnel tunnel syndrome, the second most com- is stretched 4.5 to 8 mm (since it lies pos- syndrome include patients with diabetes, mon compression neuropathy of the up- terior to the axis of motion of the elbow) obesity, as well as occupations involving per extremity. Patients often present with and the cubital tunnel cross-sectional area repetitive elbow flexion and extension, pain, paresthesias and/or weakness that if narrows by up to 55% as intraneural pres- holding tools in constant positions and left untreated may lead to significant dis- sures increase up to 20-fold.2, 3 As a result, using vibrating tools. The prevalence ability. This article reviews the etiology, repeated and sustained elbow flexion can within these populations ranges from diagnosis and management of cubital irritate the ulnar nerve and eventually lead 2.8% among workers whose occupations tunnel syndrome. to cubital tunnel syndrome. This relation- require repetitive work (e.g., assembly ship between prolonged elbow flexion line workers, packagers and cashiers) to AN ATOMY A N D ET I OLOGY and cubital tunnel syndrome has been 6.8% in floor cleaners to 42.5% among The ulnar nerve originates from reported in patients who habitually sleep vibrating tool operators.4 branches of the C8 and T1 spinal nerve in the fetal position or sleep in the prone roots and is the terminal branch of the me- position with their hands tucked under CLinicAL EVALUAT I O N A N D dial cord of the brachial plexus.