Obstetric Anesthesia This Page Intentionally Left Blank Obstetric Anesthesia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmaceutical Starting Materials/Essential Drugs
BULLETIN MNS October 2009 PHARMACEUTICAL STARTING MATERIALS MARKET NEWS SERVICE (MNS) BI -MONTHLY EDITION Market News Service Pharmaceutical Starting Materials/Essential Drugs October 2009, Issue 5 The Market News Service (MNS) is made available free of charge to all Trade Support Institutions and enterprises in Sub-Saharan African countries under a joint programme of the International Trade Centre and CBI, the Dutch Centre for the Promotion of Imports from Developing Countries (www.cbi.nl). Should you be interested in becoming an information provider and contributing to MNS' efforts to improve market transparency and facilitate trade, please contact us at [email protected]. This issue continues the series, started at the beginning of the year, focusing on the leading markets in various world regions. This issue covers the trends and recent developments in eastern European pharmaceutical markets. To subscribe to the report or to access MNS reports directly online, please contact [email protected] or visit our website at: http://www.intracen.org/mns. Copyright © MNS/ITC 2007. All rights reserved 1 Market News Service Pharmaceutical Starting Materials Introduction WHAT IS THE MNS FOR PHARMACEUTICAL STARTING MATERIALS/ESSENTIAL DRUGS? In 1986, the World Health Assembly laid before the Organization the responsibility to provide price information on pharmaceutical starting materials. WHA 39.27 endorsed WHO‟s revised drug strategy, which states “... strengthen market intelligence; support drug procurement by developing countries...” The responsibility was reaffirmed at the 49th WHA in 1996. Resolution WHA 49.14 requests the Director General, under paragraph 2(6) “to strengthen market intelligence, review in collaboration with interested parties‟ information on prices and sources of information on prices of essential drugs and starting material of good quality, which meet requirements of internationally recognized pharmacopoeias or equivalent regulatory standards, and provide this information to member states”. -
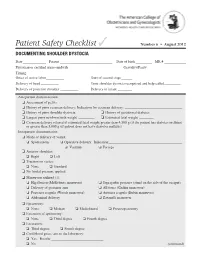
Documenting Shoulder Dystocia
Patient Safety Checklist ✓ Number 6 • August 2012 DOCUMENTING SHOULDER DYSTOCIA Date _____________ Patient _____________________________ Date of birth _________ MR # ____________ Physician or certified nurse–midwife _____________________________ Gravidity/Parity______________________ Timing: Onset of active labor __________ Start of second stage ______ Delivery of head __________ Time shoulder dystocia recognized and help called _________ Delivery of posterior shoulder __________ Delivery of infant ________ Antepartum documentation: ❏ Assessment of pelvis ❏ History of prior cesarean delivery: Indication for cesarean delivery: ________________________________ ❏ History of prior shoulder dystocia ❏ History of gestational diabetes ❏ Largest prior newborn birth weight _________ ❏ Estimated fetal weight ________ ❏ Cesarean delivery offered if estimated fetal weight greater than 4,500 g (if the patient has diabetes mellitus) or greater than 5,000 g (if patient does not have diabetes mellitus) Intrapartum documentation: ❏ Mode of delivery of vertex: ❏ Spontaneous ❏ Operative delivery: Indication: _________________________________________ ❏ Vacuum ❏ Forceps ❏ Anterior shoulder: ❏ Right ❏ Left ❏ Traction on vertex: ❏ None ❏ Standard ❏ No fundal pressure applied ❏ Maneuvers utilized (1): ❏ Hip flexion (McRoberts maneuver) ❏ Suprapubic pressure (stand on the side of the occiput) ❏ Delivery of posterior arm ❏ All fours (Gaskin maneuver) ❏ Posterior scapula (Woods maneuver) ❏ Anterior scapula (Rubin maneuver) ❏ Abdominal delivery ❏ Zavanelli maneuver -
Spring 2009 Student Journal
Volume 8 Number 1 Spring 2009 The International Student Journal of Nurse Anesthesia TOPICS IN THIS ISSUE MS & ECT Cardioprotection of Volatile Agents Hyperthermic Chemotherapy Intubating LMA Pierre Robin Syndrome Alpha Thalassemia Latex Allergy & Spina Bifida Distorted Upper Airway Volunteerism – Honduras INTERNATIONAL STUDENT JOURNAL OF NURSE ANESTHESIA Vol. 8 No. 1 Spring 2009 Editor - in - Chief Ronald L. Van Nest, CRNA, JD Associate Editors Vicki C. Coopmans, CRNA, PhD Julie A. Pearson, CRNA, PhD EDITORIAL BOARD & SECTION EDITORS Pediatrics Janet A. Dewan, CRNA, MS Northeastern University Obstetrics Greg Nezat, CRNA, PhD Navy Nurse Corps Anesthesia Program Research & Capstone Joseph E. Pellegrini, CRNA, University of Maryland PhD Regional / Pain Christopher Oudekerk, CRNA, Uniformed Services Universi- DNP ty of the Health Sciences Cardiovascular Michele Gold, CRNA, PhD University of Southern Cali- fornia Thoracic/ Fluid Balance Lori Ann Winner, CRNA, MSN University of Pennsylvania Unique Patient Syndromes Kathleen R. Wren, CRNA, PhD Florida Hospital College of Health Sciences Equipment Carrie C. Bowman Dalley, Georgetown University CRNA, MS Pharmacology Maria Magro, CRNA, MS, University of Pennsylvania MSN Pathophysiology JoAnn Platko, CRNA, MSN University of Scranton Special Surgical Techniques Russell Lynn, CRNA, MSN University of Pennsylvania 1 Airway & Respiration Michael Rieker, CRNA, DNP Wake Forest University Baptist Medical Center ,Nurse Anesthesia Program, Univer- sity of North Carolina at Greensboro Neurology & Neurosurgery -

Pain Management
BLBK137-Paul February 20, 2009 13:17 CHAPTER 8 8 Pain management Mark Nichols MD, Glenna Halvorson-Boyd PhD, RN, Robert Goldstein MD, Clifford Gevirtz MD, MPH and David Healow MD LEARNING POINTS r Proper selection of medications and nonpharmacological interventions reduces pain and anxiety and enhances patient satisfaction. r Several effective techniques exist for administration of local cervical anesthesia. Limited data support use of deep injections and adjunctive premedication with nonsteroidal antiinflammatory drugs. r The most common conscious sedation regimen used by North American abortion providers is a combination of fentanyl and midazolam. r Deep sedation and general anesthesia carry important benefits for certain patients, but they require specialized personnel and equipment. Introduction Pain associated with abortion Managing pain associated with abortion procedures is an es- Pain management remains an important challenge in abor- sential goal in the care of patients requesting pregnancy ter- tion practice, although studies suggest that progress in pain mination. Effective methods range from local cervical anes- control has been achieved over time in the USA. In a sur- thesia, with or without supplemental oral or intravenous vey in the late 1970s, 2,299 women having abortions with (IV) medications, to general anesthesia (GA). A number cervical anesthesia were asked to rate their pain as “mild, of factors influence the options available to patients, in- moderate, or severe.” Forty-six per cent called the pain mod- cluding local regulations, safety considerations, facility in- erate, and 32% called it severe. [2] A survey conducted two frastructure and resources, cost, and insurance coverage. decades later of more than 2,000 patients at 12 abortion fa- In the USA, where most abortions occur in freestanding cilities in the USA found that 30% of patients felt no pain, clinics, cervical anesthesia with or without IV conscious 25% mild pain, 29% moderate pain, and 14% severe pain. -

Authors Conducted an E-Mail Survey of Anesthesiologists in the US in 2010
Appendix 2: Reference 1 Methods: Authors conducted an e-mail survey of Anesthesiologists in the US in 2010. Results: “Five thousand anesthesiologists were solicited; 615 (12.3%) responses were received. Twenty-four percent of respondents had installed an AIMS, while 13% were either installing a system now or had selected one, and an additional 13% were actively searching. Larger anesthesiology groups with large case loads, urban settings, and government affiliated or academic institutions were more likely to have adopted AIMS. Initial cost was the most frequently cited AIMS barrier. The most commonly cited benefit was more accurate clinical documentation (79%), while unanticipated need for ongoing information technology support (49%) and difficult integration of AIMS with an existing EMR (61%) were the most commonly cited problems.” [Trentman TL, Mueller JT, Ruskin KJ, Noble BN, Doyle CA. Adoption of anesthesia information management systems by US anesthesiologists. J Clin Monit Comput 2011;25:129–35.] Reference 2 Joint Commission Report. 60 [Kohn L, Corrigan JM, Donaldson MS. To Err is Human: Building a Safer Health System. Report from the Committee on Quality of Health Care in America. Washington DC: The Joint Commission journal on quality improvement, 1999:227–34.] Reference 3 Excerpt: “The Department of Health and Human Services (DHHS) released two proposed regulations affecting HIT (www.healthit.hhs.gov). The first, a notice of proposed rule- making (NPRM), describes how hospitals, physicians, and other health care professionals can qualify for billions of dollars of extra Medicare and Medicaid payments through the meaningful use of electronic health records (EHRs). The second, an interim final regulation, describes the standards and certification criteria that those EHRs must meet for their users to collect the payments. -

Unesco – Eolss Sample Chapters
PHARMACOLOGY – Vol. II - Anesthetics - Amanda Baric and David Pescod. ANESTHETICS Amanda Baric and David Pescod. Department of Anesthesia and Perioperative medicine, The Northern Hospital, Melbourne, Australia. Keywords: Anesthesia, pharmacology, inhalational, neuromuscular blockade, induction agent, local anesthetic. Contents 1. Inhalation agents 1.1. Introduction 1.2. Pharmacokinetics and Pharmacodynamics 1.3. Specific Agents 1.3.1. Diethyl Ether (Ether) 1.3.2. Chloroform 1.3.3. Cyclopropane 1.3.4. Trichloroethylene 1.3.5. Halogenated Alkanes and Ethers 1.3.6. Nitrous Oxide. 1.3.7. Xenon 2. Neuromuscular blocking agents. 2.1. Introduction 2.2. Non-Depolarizing Muscle Relaxants 2.2.1. Tubocurarine (1935) 2.2.2. Metocurine (dimethyl tubocurarine chloride/bromide) 2.2.3. Alcuronium (1961) 2.2.4. Gallamine (1948) 2.2.5. Pancuronium (1968) 2.2.6. Vecuronium (1983) 2.2.7. Atracurium (1980s) 2.2.8. Cis-atracurium (1995) 2.2.9. Mivacurium (1993) 2.2.10. Rocuronium (1994) 2.2.11. SugammadexUNESCO (2003) – EOLSS 2.2.12. Rapacuronium 2.3. Reversal Drugs (Anticholinesterase) 2.4. DepolarizingSAMPLE Muscle Relaxants (Suxamethonium CHAPTERS or Succinylcholine) 3. Local anesthetics 3.1. Introduction 3.2. Pharmacokinetics and Pharmacodynamics 3.3. Toxicity 3.4. Specific Agents 3.4.1. Cocaine 3.4.2. Procaine 3.4.3 Chloroprocaine 3.4.4. Tetracaine (Amethocaine) ©Encyclopedia of Life Support Systems (EOLSS) PHARMACOLOGY – Vol. II - Anesthetics - Amanda Baric and David Pescod. 3.4.5. Lidocaine 3.4.6. Prilocaine 3.4.7. Mepivacaine 3.4.8. Bupivacaine 3.4.9. Ropivacaine 3.4.10. Eutectic Mixture of Local Anesthetics (EMLA) 4. Intravenous Induction Agents 4.1. -

Pharmacology – Inhalant Anesthetics
Pharmacology- Inhalant Anesthetics Lyon Lee DVM PhD DACVA Introduction • Maintenance of general anesthesia is primarily carried out using inhalation anesthetics, although intravenous anesthetics may be used for short procedures. • Inhalation anesthetics provide quicker changes of anesthetic depth than injectable anesthetics, and reversal of central nervous depression is more readily achieved, explaining for its popularity in prolonged anesthesia (less risk of overdosing, less accumulation and quicker recovery) (see table 1) Table 1. Comparison of inhalant and injectable anesthetics Inhalant Technique Injectable Technique Expensive Equipment Cheap (needles, syringes) Patent Airway and high O2 Not necessarily Better control of anesthetic depth Once given, suffer the consequences Ease of elimination (ventilation) Only through metabolism & Excretion Pollution No • Commonly administered inhalant anesthetics include volatile liquids such as isoflurane, halothane, sevoflurane and desflurane, and inorganic gas, nitrous oxide (N2O). Except N2O, these volatile anesthetics are chemically ‘halogenated hydrocarbons’ and all are closely related. • Physical characteristics of volatile anesthetics govern their clinical effects and practicality associated with their use. Table 2. Physical characteristics of some volatile anesthetic agents. (MAC is for man) Name partition coefficient. boiling point MAC % blood /gas oil/gas (deg=C) Nitrous oxide 0.47 1.4 -89 105 Cyclopropane 0.55 11.5 -34 9.2 Halothane 2.4 220 50.2 0.75 Methoxyflurane 11.0 950 104.7 0.2 Enflurane 1.9 98 56.5 1.68 Isoflurane 1.4 97 48.5 1.15 Sevoflurane 0.6 53 58.5 2.5 Desflurane 0.42 18.7 25 5.72 Diethyl ether 12 65 34.6 1.92 Chloroform 8 400 61.2 0.77 Trichloroethylene 9 714 86.7 0.23 • The volatile anesthetics are administered as vapors after their evaporization in devices known as vaporizers. -
Chapter 17 Spinal, Epidural, and Caudal Anesthesia
Chapter SPINAL, EPIDURAL, AND 17 CAUDAL ANESTHESIA Alan J.R. Macfarlane, Richard Brull, and Vincent W.S. Chan PRINCIPLES COMBINED SPINAL-EPIDURAL ANESTHESIA PRACTICE Technique ANATOMY CAUDAL ANESTHESIA Spinal Nerves Pharmacology Blood Supply Technique Anatomic Variations COMPLICATIONS MECHANISM OF ACTION Neurologic Drug Uptake and Distribution Cardiovascular Drug Elimination Respiratory PHYSIOLOGIC EFFECTS Infection Cardiovascular Backache Central Nervous System Nausea and Vomiting Respiratory Urinary Retention Gastrointestinal Pruritus Renal Shivering Complications Unique to Epidural Anesthesia INDICATIONS Neuraxial Anesthesia RECENT ADVANCES IN ULTRASONOGRAPHY Neuraxial Analgesia QUESTIONS OF THE DAY CONTRAINDICATIONS Absolute Relative PRINCIPLES SPINAL ANESTHESIA Factors Affecting Block Height Spinal, epidural, and caudal blocks are collectively referred Duration of the Block to as central neuraxial blocks. Significant technical, physi- Pharmacology ologic, and pharmacologic differences exist between the Technique techniques, although all result in one or a combination of Monitoring of the Block sympathetic, sensory, and motor blockade. Spinal anes- EPIDURAL ANESTHESIA thesia requires a small amount of drug to produce rapid, Factors Affecting Epidural Block Height profound, reproducible, but finite sensory analgesia. In Pharmacology contrast, epidural anesthesia progresses more slowly, is Technique commonly prolonged using a catheter, and requires a large amount of local anesthetic, which may be associated with The editors and publisher would like to thank Drs. Kenneth Dras- ner and Merlin D. Larson for contributing to this chapter in the previous edition of this work. It has served as the foundation for the current chapter. 273 Downloaded for Wendy Nguyen ([email protected]) at University Of Minnesota - Twin Cities Campus from ClinicalKey.com by Elsevier on March 26, 2018. For personal use only. -

Spinal Anaesthesia for Laparoscopic Cholecystectomy
Rev. Col. Anest. Mayo-Julio 2009. Vol. 37- No. 2: 111-118 Spinal anaesthesia for laparoscopic cholecystectomy PatIents and MethOds • Patients aged less than 18 and older than 75; -2 • Patients having greater than 30 Kg/m body A descriptive prospective study was carried out mass index (BMI); between June and September 2008 in the Caribe teaching hospital in the city of Cartagena in Co- • Sick patients having contraindication for lapa- lombia, South America. Once the Caribe teaching roscopic surgery; hospital’s medical ethics’ committee’s approval had • Patients having contraindication for spinal been sought and given, patients were included in anaesthesia; the study who had biliary lithiasis accompanied by a clinical picture of chronic cholecystitis as well as • Patients who preferred general anaesthesia; those having a clinical picture of subacute cholecys- and titis diagnosed during preoperative exam. • An inability for carrying out postoperative follow- Patients who had been previously diagnosed as up. having complicated biliary lithiasis (acute chole- Inclusion criteria consisted of ASA I – II patients cystitis, choledocolithiasis, acute cholangitis, acute aged 18 to 75. All the patients complied with a biliary pancreatitis, etc.) were excluded. Other ex- minimum 8 hours fast; antibiotic prophylaxis was clusion criteria were as follows: 115 Anestesia espinal para colecistectomia laparoscópica - Jiménez J.C., Chica J., Vargas D. Rev. Col. Anest. Mayo-Julio 2009. Vol. 37- No. 2: 111-118 administered 15 minutes before the procedure (1 g tolerance to oral route had been produced and the intravenous cephazoline) anaesthesiologist had verified the absence of any type of complication. All patients were prescribed ANAESTHETIC TECHNIQUE ibuprofen as analgesia to be taken at home (400 mgr each 8 hours for 3 days). -

A Guide to Obstetrical Coding Production of This Document Is Made Possible by Financial Contributions from Health Canada and Provincial and Territorial Governments
ICD-10-CA | CCI A Guide to Obstetrical Coding Production of this document is made possible by financial contributions from Health Canada and provincial and territorial governments. The views expressed herein do not necessarily represent the views of Health Canada or any provincial or territorial government. Unless otherwise indicated, this product uses data provided by Canada’s provinces and territories. All rights reserved. The contents of this publication may be reproduced unaltered, in whole or in part and by any means, solely for non-commercial purposes, provided that the Canadian Institute for Health Information is properly and fully acknowledged as the copyright owner. Any reproduction or use of this publication or its contents for any commercial purpose requires the prior written authorization of the Canadian Institute for Health Information. Reproduction or use that suggests endorsement by, or affiliation with, the Canadian Institute for Health Information is prohibited. For permission or information, please contact CIHI: Canadian Institute for Health Information 495 Richmond Road, Suite 600 Ottawa, Ontario K2A 4H6 Phone: 613-241-7860 Fax: 613-241-8120 www.cihi.ca [email protected] © 2018 Canadian Institute for Health Information Cette publication est aussi disponible en français sous le titre Guide de codification des données en obstétrique. Table of contents About CIHI ................................................................................................................................. 6 Chapter 1: Introduction .............................................................................................................. -

Pharmacology on Your Palms CLASSIFICATION of the DRUGS
Pharmacology on your palms CLASSIFICATION OF THE DRUGS DRUGS FROM DRUGS AFFECTING THE ORGANS CHEMOTHERAPEUTIC DIFFERENT DRUGS AFFECTING THE NERVOUS SYSTEM AND TISSUES DRUGS PHARMACOLOGICAL GROUPS Drugs affecting peripheral Antitumor drugs Drugs affecting the cardiovascular Antimicrobial, antiviral, Drugs affecting the nervous system Antiallergic drugs system antiparasitic drugs central nervous system Drugs affecting the sensory Antidotes nerve endings Cardiac glycosides Antibiotics CNS DEPRESSANTS (AFFECTING THE Antihypertensive drugs Sulfonamides Analgesics (opioid, AFFERENT INNERVATION) Antianginal drugs Antituberculous drugs analgesics-antipyretics, Antiarrhythmic drugs Antihelminthic drugs NSAIDs) Local anaesthetics Antihyperlipidemic drugs Antifungal drugs Sedative and hypnotic Coating drugs Spasmolytics Antiviral drugs drugs Adsorbents Drugs affecting the excretory system Antimalarial drugs Tranquilizers Astringents Diuretics Antisyphilitic drugs Neuroleptics Expectorants Drugs affecting the hemopoietic system Antiseptics Anticonvulsants Irritant drugs Drugs affecting blood coagulation Disinfectants Antiparkinsonian drugs Drugs affecting peripheral Drugs affecting erythro- and leukopoiesis General anaesthetics neurotransmitter processes Drugs affecting the digestive system CNS STIMULANTS (AFFECTING THE Anorectic drugs Psychomotor stimulants EFFERENT PART OF THE Bitter stuffs. Drugs for replacement therapy Analeptics NERVOUS SYSTEM) Antiacid drugs Antidepressants Direct-acting-cholinomimetics Antiulcer drugs Nootropics (Cognitive -

Sedative Effect of Propofol and Midazolam in Surgery Under Spinal Anaesthesia: a Comparative Study
Indian Journal of Clinical Anaesthesia 2020;7(1):187–191 Content available at: iponlinejournal.com Indian Journal of Clinical Anaesthesia Journal homepage: www.innovativepublication.com Original Research Article Sedative effect of propofol and midazolam in surgery under spinal anaesthesia: A comparative study Jalpen N Patel1, Jyotsna F Maliwad2,*, Purvi J Mehta1, Raman D Damor3, Kalpita S Shringarpure3 1Dept. of Anesthesiology, Shri M P Shah Medical College, Jamnagar, Gujarat, India 2Dept. of Anasthesiology, Medical College, Baroda, Gujarat, India 3Dept. of Community Medicine, Medical College, Baroda, Gujarat, India ARTICLEINFO ABSTRACT Article history: Introduction: Intravenous medications are invariably required to allay anxiety related to surgical Received 27-11-2019 procedures, in patients undergoing surgery under regional anesthesia. A thorough pre anaesthetic check Accepted 30-11-2019 up and details of the surgical procedure planned are necessary before administration of sedative agents to Available online 28-02-2020 attain desirable levels of sedation and avoid unwanted adverse events. Objective: To observe, record and analyse sedative effect of intravenous Propofol and Midazolam in lower extremities and lower abdominal surgery scheduled under regional anesthesia techniques. Keywords: Materials and Methods: A single blinded comparative study conducted in tertiary care hospital of Gujarat. Sedative effect Sixty patients with no organic pathology & a moderate but definite systemic disturbance categorized into Subarachnoid block two groups labeled as propofol group (n=30) and Midazolam group (n=30) of either gender and shortlisted Anxiety for surgery using subarachnoid block. Observer’s Assessment of Alertness/Sedation Scale (OAA/S Scale) and Ramsay sedation scale was used to assess effective sedation. Results: Basic patients characteristics, Mean age (SD) was 31.57 + 10.57 years in category I (P group) and 35.33 + 9.98 years in category II (M group) was comparable between the groups.