The Chemokine System in Innate Immunity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prognostic Value of CXCL17 and CXCR8 Expression in Patients with Colon Cancer
ONCOLOGY LETTERS 20: 2711-2720, 2020 Prognostic value of CXCL17 and CXCR8 expression in patients with colon cancer HONGYAN YAO1,2, YUFENG LV3, XUEFENG BAI4, ZHAOJIN YU4 and XIAOJIAN LIU1 1Department of Pharmacology, School of Basic Medical Sciences, Jinzhou Medical University; 2Nuclear Medicine Department, Jinzhou Central Hospital, Jinzhou, Liaoning 121001; 3Department of Respiration and Critical Care, The Affiliated Hongqi Hospital of Mudanjiang Medical University, Mudanjiang, Heilongjiang 157011; 4Department of Pharmacology, School of Pharmacy, China Medical University, Shenyang, Liaoning 110001, P.R. China Received October 11, 2019; Accepted May 27, 2020 DOI: 10.3892/ol.2020.11819 Abstract. C-X-C motif chemokine ligand 17 (CXCL17) is a CXCL17/CXCR8 signalling may be involved in colon cancer mucous chemokine and its expression is highly correlated with and contribute to improved patient outcomes. that of G protein-coupled receptor 35 (GPR35), which has been confirmed as its receptor and named C‑X‑C motif chemokine Introduction receptor 8 (CXCR8). CXCL17 is upregulated in several types of cancer. However, the biological role of this chemokine Chemokines are a large family of cytokines serving important in colon cancer remains unknown. In the present study, the roles in the immune system, such as the regulation of cell traf- expression levels of CXCL17 and CXCR8 were examined ficking to inflammatory sites (1). By regulating the activity of using immunohistochemistry in 101 colon cancer tissues and cells in homeostasis and signal transduction, chemokines are 79 healthy tumour-adjacent tissues. CXCL17 and CXCR8 involved in numerous physiological and pathological processes expression levels were increased in the colon cancer samples such as angiogenesis, embryonic development, wound healing, compared with tumour-adjacent samples. -

Induces Homing of Antigen-Specific and Non Chemokine-Adjuvanted
Chemokine-Adjuvanted Plasmid DNA Induces Homing of Antigen-Specific and Non −Antigen-Specific B and T Cells to the Intestinal and Genital Mucosae This information is current as of September 25, 2021. Yoann Aldon, Sven Kratochvil, Robin J. Shattock and Paul F. McKay J Immunol published online 8 January 2020 http://www.jimmunol.org/content/early/2020/01/07/jimmun ol.1901184 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2020/01/07/jimmunol.190118 Material 4.DCSupplemental http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 25, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Author Choice Freely available online through The Journal of Immunology Author Choice option Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2020 The Authors All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published January 8, 2020, doi:10.4049/jimmunol.1901184 The Journal of Immunology Chemokine-Adjuvanted Plasmid DNA Induces Homing of Antigen-Specific and Non–Antigen-Specific B and T Cells to the Intestinal and Genital Mucosae Yoann Aldon, Sven Kratochvil, Robin J. -

Disease Lymphocytes in Small Intestinal Crohn's Chemokine
Phenotype and Effector Function of CC Chemokine Receptor 9-Expressing Lymphocytes in Small Intestinal Crohn's Disease This information is current as of September 29, 2021. Masayuki Saruta, Qi T. Yu, Armine Avanesyan, Phillip R. Fleshner, Stephan R. Targan and Konstantinos A. Papadakis J Immunol 2007; 178:3293-3300; ; doi: 10.4049/jimmunol.178.5.3293 http://www.jimmunol.org/content/178/5/3293 Downloaded from References This article cites 26 articles, 12 of which you can access for free at: http://www.jimmunol.org/content/178/5/3293.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 29, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2007 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Phenotype and Effector Function of CC Chemokine Receptor 9-Expressing Lymphocytes in Small Intestinal Crohn’s Disease1 Masayuki Saruta,2*QiT.Yu,2* Armine Avanesyan,* Phillip R. Fleshner,† Stephan R. -

Differentiation and Bone Resorption Role of CX3CL1/Fractalkine In
Role of CX3CL1/Fractalkine in Osteoclast Differentiation and Bone Resorption Keiichi Koizumi, Yurika Saitoh, Takayuki Minami, Nobuhiro Takeno, Koichi Tsuneyama, Tatsuro Miyahara, This information is current as Takashi Nakayama, Hiroaki Sakurai, Yasuo Takano, Miyuki of September 29, 2021. Nishimura, Toshio Imai, Osamu Yoshie and Ikuo Saiki J Immunol published online 18 November 2009 http://www.jimmunol.org/content/early/2009/11/18/jimmuno l.0803627.citation Downloaded from Why The JI? Submit online. http://www.jimmunol.org/ • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average by guest on September 29, 2021 Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published November 18, 2009, doi:10.4049/jimmunol.0803627 The Journal of Immunology Role of CX3CL1/Fractalkine in Osteoclast Differentiation and Bone Resorption1 Keiichi Koizumi,2* Yurika Saitoh,* Takayuki Minami,* Nobuhiro Takeno,* Koichi Tsuneyama,†‡ Tatsuro Miyahara,§ Takashi Nakayama,¶ Hiroaki Sakurai,*† Yasuo Takano,‡ Miyuki Nishimura,ʈ Toshio Imai,ʈ Osamu Yoshie,¶ and Ikuo Saiki*† The recruitment of osteoclast precursors toward osteoblasts and subsequent cell-cell interactions are critical for osteoclast dif- ferentiation. -

CD74 Targeted Nanoparticles As Dexamethasone Delivery System for B Lymphoid Malignancies
CD74 targeted nanoparticles as Dexamethasone Delivery System for B lymphoid malignancies DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Georgia Triantafillou, MPH Integrated Biomedical Sciences Graduate Program The Ohio State University 2011 Dissertation Committee John C. Byrd, MD, advisor Natarajan Muthusamy, PhD co-advisor Robert J.Lee, PhD, co-advisor Mitch A.Phelps, PhD, co-advisor Guido Marcucci, MD committee member Susheela Tridandapani, PhD committee member Copyright page Georgia Triantafillou 2011 ABSTRACT Chronic Lymphocytic Leukemia (CLL) is the most common adult leukemia and is not curable with standard therapy. In CLL the B lymphocytes appear morphologically mature but immunologically express less mature B cell makers. Specifically, the CLL B cells co-express surface antigens including CD19, CD20, CD5, CD23. Due to nonspecific delivery of the drugs to malignant as well as normal cells, patients experience numerous side effects. Targeted drug delivery to cancer cells is a desirable goal for all anti cancer strategies. Corticosteroids have been proven to be a beneficial and well established part of CLL treatment. Dexamethasone(DEX) is frequently used in CLL therapies as well as other malignancies and antiinflammatory diseases. However, DEX nonspecifically enters all tissues inducing various toxicities to patients. Therefore, DEX treatment is often discontinued or not administered to certain patients. We aimed to deliver this efficient clinical agent via a targeted delivery vehicle and examine its effect on its target B-CLL cells. The main scope of the work presented is the creation of a sterically stable nanoparticle, an ii immunoliposome (ILP), that has DEX encapsulated in its interior and a monoclonal antibody(Mab) in its exterior targeting CLL B cells expressing the surface antigen that is recognized by the Mab. -

Atypical Chemokine Receptor 4 Shapes Activated B Cell Fate
Brief Definitive Report Atypical chemokine receptor 4 shapes activated B cell fate Ervin E. Kara,1 Cameron R. Bastow,1 Duncan R. McKenzie,1 Carly E. Gregor,1 Kevin A. Fenix,1 Rachelle Babb,1 Todd S. Norton,1 Dimitra Zotos,3 Lauren B. Rodda,4 Jana R. Hermes,6 Katherine Bourne,6 Derek S. Gilchrist,7 Robert J. Nibbs,7 Mohammed Alsharifi,1 Carola G. Vinuesa,8 David M. Tarlinton,3,9 Robert Brink,6,10 Geoffrey R. Hill,11 Jason G. Cyster,4,5 Iain Comerford,1 and Shaun R. McColl1,2 1Department of Molecular and Cellular Biology, School of Biological Sciences and 2Centre for Molecular Pathology, School of Biological Sciences, University of Adelaide, Adelaide, South Australia, Australia 3Walter and Eliza Hall Institute of Medical Research, Parkville, Victoria, Australia 4Department of Microbiology and Immunology and 5Howard Hughes Medical Institute, Department of Microbiology and Immunology, University of California, Downloaded from http://rupress.org/jem/article-pdf/215/3/801/1168927/jem_20171067.pdf by guest on 28 September 2021 San Francisco, San Francisco, CA 6Immunology Division, Garvan Institute of Medical Research, Darlinghurst, New South Wales, Australia 7Institute of Infection, Immunity and Inflammation, College of Medicine, Veterinary and Life Sciences, University of Glasgow, Glasgow, Scotland, UK 8Department of Immunology and Infectious Disease, John Curtin School of Medical Research, Australian National University, Canberra, Australian Capital Territory, Australia 9Department of Immunology and Pathology, Monash University, Melbourne, Victoria, Australia 10St Vincent’s Clinical School, University of New South Wales, Darlinghurst, New South Wales, Australia 11Immunology Department, QIMR Berghofer Medical Research Institute, Brisbane, Queensland, Australia Activated B cells can initially differentiate into three functionally distinct fates—early plasmablasts (PBs), germinal center (GC) B cells, or early memory B cells—by mechanisms that remain poorly understood. -

Single-Cell RNA Sequencing Identifies Candidate Renal
BASIC RESEARCH www.jasn.org Single-Cell RNA Sequencing Identifies Candidate Renal Resident Macrophage Gene Expression Signatures across Species Kurt A. Zimmerman,1 Melissa R. Bentley,1 Jeremie M. Lever ,2 Zhang Li,1 David K. Crossman,3 Cheng Jack Song,1 Shanrun Liu,4 Michael R. Crowley,3 James F. George,5 Michal Mrug,2,6 and Bradley K. Yoder1 1Department of Cell, Developmental, and Integrative Biology, 2Division of Nephrology, Department of Medicine, 3Department of Genetics, 4Department of Biochemistry and Molecular Genetics, and 5Division of Cardiothoracic Surgery, Department of Surgery, University of Alabama at Birmingham, Birmingham, Alabama; and 6Department of Veterans Affairs Medical Center, Birmingham, Alabama ABSTRACT Background Resident macrophages regulate homeostatic and disease processes in multiple tissues, in- cluding the kidney. Despite having well defined markers to identify these cells in mice, technical limita- tions have prevented identification of a similar cell type across species. The inability to identify resident macrophage populations across species hinders the translation of data obtained from animal model to human patients. Methods As an entry point to determine novel markers that could identify resident macrophages across species, we performed single-cell RNA sequencing (scRNAseq) analysis of all T and B cell–negative CD45+ innate immune cells in mouse, rat, pig, and human kidney tissue. Results We identified genes with enriched expression in mouse renal resident macrophages that were also present in candidate resident macrophage populations across species. Using the scRNAseq data, we defined a novel set of possible cell surface markers (Cd74 and Cd81) for these candidate kidney resident macrophages. We confirmed, using parabiosis and flow cytometry, that these proteins are indeed enriched in mouse resident macrophages. -
Cxcl17 and Its Association with T Cells
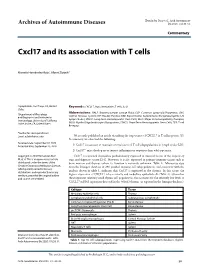
Hernández-Ruiz et al., Arch Autoimmune Archives of Autoimmune Diseases Dis 2020; 1(1):28-31. Commentary Cxcl17 and its association with T cells Marcela Hernández-Ruiz1, Albert Zlotnik2* 1Lymphotrek, San Diego, CA, United Keywords: CXCL17, Auto immunities, T cells, IL-23 States Abbreviations: BALF: Bronchoalveolar Lavage Fluid; CLP: Common Lymphoid Progenitor; CNS: 2Department of Physiology Central Nervous System; DP: Double Positive; EAE: Experimental Autoimmune Encephalomyelitis; LN: and Biophysics and Institute for Lymph Nodes; LTHSC: Long-term Hematopoietic Stem Cells; MHC: Major Histocompatibility Complex; Immunology, University of California Irvine, Irvine, CA, United States MOG: Myelin Oligodendrocyte Glycoprotein; STHCS: Short-Term Hematopoietic Stem Cells; TCR: T cell Receptor *Author for correspondence: Email: [email protected] We recently published an article describing the importance of CXCL17 in T cell responses [1]. In summary, we observed the following: Received date: September 02, 2020 Accepted date: September 23, 2020 1) Cxcl17 is necessary to maintain normal ratios of T cell subpopulations in lymph nodes (LN). 2) Cxcl17-/- mice develop more intense inflammatory responses than wild type mice. Copyright: © 2020 Hernández-Ruiz Cxcl17 is a mucosal chemokine predominantly expressed in mucosal tissues of the respiratory M, et al. This is an open-access article tract and digestive system [2-4]. However, it is also expressed in primary immune tissues such as distributed under the terms of the bone marrow and thymus (where its function is currently unknown- Table 1). Microarray data Creative Commons Attribution License, from the Immgen database of 298 purified immune cell subpopulations, and consistent with the which permits unrestricted use, distribution, and reproduction in any analysis shown in table 1, indicates that Cxcl17 is expressed in the thymus. -

Human B Cells Expression in Terminally Differentiating Induces
1,25-Dihydroxyvitamin D3 Induces CCR10 Expression in Terminally Differentiating Human B Cells This information is current as Aiko-Konno Shirakawa, Daisuke Nagakubo, Kunio of September 28, 2021. Hieshima, Takashi Nakayama, Zhe Jin and Osamu Yoshie J Immunol 2008; 180:2786-2795; ; doi: 10.4049/jimmunol.180.5.2786 http://www.jimmunol.org/content/180/5/2786 Downloaded from References This article cites 55 articles, 29 of which you can access for free at: http://www.jimmunol.org/content/180/5/2786.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 28, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2008 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology 1,25-Dihydroxyvitamin D3 Induces CCR10 Expression in Terminally Differentiating Human B Cells1 Aiko-Konno Shirakawa,2 Daisuke Nagakubo,2 Kunio Hieshima, Takashi Nakayama, Zhe Jin, and Osamu Yoshie3 In the B cell lineage, CCR10 is known to be selectively expressed by plasma cells, especially those secreting IgA. -

Acting on the CCR1 Receptor Mediates Neutrophil Migration in Immune Inflammation Via Sequential ␣ Release of TNF- and LTB4 Cleber D
MIP-1␣[CCL3] acting on the CCR1 receptor mediates neutrophil migration in immune inflammation via sequential ␣ release of TNF- and LTB4 Cleber D. L. Ramos,* Claudio Canetti,*,† Janeusa T. Souto,‡,§ Joa˜ o S. Silva,‡ Cory M. Hogaboam,¶ Sergio H. Ferreira,* and Fernando Q. Cunha*,1 Departments of *Pharmacology and ‡Biochemistry and Immunology, School of Medicine of Ribeira˜o Preto, University of Sa˜o Paulo, Brazil; §Department of Microbiology and Parasitology, Federal University of Rio Grande do Norte, Natal, RN, Brazil; and †Division of Pulmonary & Critical Care Medicine and ¶Department of Pathology, University of Michigan, Ann Arbor Abstract: In the present study, we investigated nists might have a therapeutic potential. J. Leukoc. the involvement of macrophage-inflammatory pro- Biol. 78: 167–177; 2005. tein-1␣ (MIP-1␣)[CC chemokine ligand 3 (CCL3)], MIP-1[CCL4], regulated on activation, normal Key Words: chemokines ⅐ chemokine receptors ⅐ chemotaxis T expressed and secreted (RANTES)[CCL5], and CC chemokine receptors (CCRs) on neutrophil mi- gration in murine immune inflammation. Previ- INTRODUCTION ously, we showed that ovalbumin (OVA)-triggered neutrophil migration in immunized mice depends on the sequential release of tumor necrosis factor Neutrophil migration is a complex process, which results ␣ ␣ mainly from the release of neutrophil chemotactic factors by (TNF- ) and leukotriene B4 (LTB4). Herein, we show increased mRNA expression for MIP- resident cells, inducing rolling and adhesion of neutrophils on 1␣[CCL3], MIP-1[CCL4], RANTES[CCL5], and endothelial cells, followed by their transmigration to the ex- travascular space [1, 2]. Apart from its importance in host CCR1 in peritoneal cells harvested from OVA-chal- defense, the migration of neutrophils to the inflammatory site lenged, immunized mice, as well as MIP-1␣[CCL3] is, at least in part, responsible for tissue damage observed in and RANTES[CCL5] but not MIP-1[CCL4] proteins several inflammatory diseases such as rheumatoid arthritis, in the peritoneal exudates. -

Antimicrobial Activity As a Chemokine with Broad-Spectrum CCL28 Has
CCL28 Has Dual Roles in Mucosal Immunity as a Chemokine with Broad-Spectrum Antimicrobial Activity This information is current as Kunio Hieshima, Haruo Ohtani, Michiko Shibano, Dai of September 26, 2021. Izawa, Takashi Nakayama, Yuri Kawasaki, Fumio Shiba, Mitsuru Shiota, Fuminori Katou, Takuya Saito and Osamu Yoshie J Immunol 2003; 170:1452-1461; ; doi: 10.4049/jimmunol.170.3.1452 Downloaded from http://www.jimmunol.org/content/170/3/1452 References This article cites 36 articles, 19 of which you can access for free at: http://www.jimmunol.org/content/170/3/1452.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists by guest on September 26, 2021 • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2003 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology CCL28 Has Dual Roles in Mucosal Immunity as a Chemokine with Broad-Spectrum Antimicrobial Activity1 Kunio Hieshima,* Haruo Ohtani,2‡ Michiko Shibano,* Dai Izawa,* Takashi Nakayama,* Yuri Kawasaki,* Fumio Shiba,* Mitsuru Shiota,† Fuminori Katou,§ Takuya Saito,¶ and Osamu Yoshie3* CCL28 is a CC chemokine signaling via CCR10 and CCR3 that is selectively expressed in certain mucosal tissues such as exocrine glands, trachea, and colon. -

G Protein-Coupled Receptors As Therapeutic Targets for Multiple Sclerosis
npg GPCRs as therapeutic targets for MS Cell Research (2012) 22:1108-1128. 1108 © 2012 IBCB, SIBS, CAS All rights reserved 1001-0602/12 $ 32.00 npg REVIEW www.nature.com/cr G protein-coupled receptors as therapeutic targets for multiple sclerosis Changsheng Du1, Xin Xie1, 2 1Laboratory of Receptor-Based BioMedicine, Shanghai Key Laboratory of Signaling and Disease Research, School of Life Sci- ences and Technology, Tongji University, Shanghai 200092, China; 2State Key Laboratory of Drug Research, the National Center for Drug Screening, Shanghai Institute of Materia Medica, Chinese Academy of Sciences, 189 Guo Shou Jing Road, Pudong New District, Shanghai 201203, China G protein-coupled receptors (GPCRs) mediate most of our physiological responses to hormones, neurotransmit- ters and environmental stimulants. They are considered as the most successful therapeutic targets for a broad spec- trum of diseases. Multiple sclerosis (MS) is an inflammatory disease that is characterized by immune-mediated de- myelination and degeneration of the central nervous system (CNS). It is the leading cause of non-traumatic disability in young adults. Great progress has been made over the past few decades in understanding the pathogenesis of MS. Numerous data from animal and clinical studies indicate that many GPCRs are critically involved in various aspects of MS pathogenesis, including antigen presentation, cytokine production, T-cell differentiation, T-cell proliferation, T-cell invasion, etc. In this review, we summarize the recent findings regarding the expression or functional changes of GPCRs in MS patients or animal models, and the influences of GPCRs on disease severity upon genetic or phar- macological manipulations.