Ruptured Aneurysm of the Sinus of Valsalva Causing Pulmonary Embolism: a Rare Association
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Venous Air Embolism, Result- Retrospective Study of Patients with Venous Or Arterial Ing in Prompt Hemodynamic Improvement
Ⅵ REVIEW ARTICLE David C. Warltier, M.D., Ph.D., Editor Anesthesiology 2007; 106:164–77 Copyright © 2006, the American Society of Anesthesiologists, Inc. Lippincott Williams & Wilkins, Inc. Diagnosis and Treatment of Vascular Air Embolism Marek A. Mirski, M.D., Ph.D.,* Abhijit Vijay Lele, M.D.,† Lunei Fitzsimmons, M.D.,† Thomas J. K. Toung, M.D.‡ exogenously delivered gas) from the operative field or This article has been selected for the Anesthesiology CME Program. After reading the article, go to http://www. other communication with the environment into the asahq.org/journal-cme to take the test and apply for Cate- venous or arterial vasculature, producing systemic ef- gory 1 credit. Complete instructions may be found in the fects. The true incidence of VAE may be never known, CME section at the back of this issue. much depending on the sensitivity of detection methods used during the procedure. In addition, many cases of Vascular air embolism is a potentially life-threatening event VAE are subclinical, resulting in no untoward outcome, that is now encountered routinely in the operating room and and thus go unreported. Historically, VAE is most often other patient care areas. The circumstances under which phy- associated with sitting position craniotomies (posterior sicians and nurses may encounter air embolism are no longer fossa). Although this surgical technique is a high-risk limited to neurosurgical procedures conducted in the “sitting procedure for air embolism, other recently described position” and occur in such diverse areas as the interventional radiology suite or laparoscopic surgical center. Advances in circumstances during both medical and surgical thera- monitoring devices coupled with an understanding of the peutics have further increased concern about this ad- pathophysiology of vascular air embolism will enable the phy- verse event. -

Pulmonary Embolism a Pulmonary Embolism Occurs When a Blood Clot Moves Through the Bloodstream and Becomes Lodged in a Blood Vessel in the Lungs
Pulmonary Embolism A pulmonary embolism occurs when a blood clot moves through the bloodstream and becomes lodged in a blood vessel in the lungs. This can make it hard for blood to pass through the lungs to get oxygen. Diagnosing a pulmonary embolism can be difficult because half of patients with a clot in the lungs have no symptoms. Others may experience shortness of breath, chest pain, dizziness, and possibly swelling in the legs. If you have a pulmonary embolism, you need medical treatment right away to prevent a blood clot from blocking blood flow to the lungs and heart. Your doctor can confirm the presence of a pulmonary embolism with CT angiography, or a ventilation perfusion (V/Q) lung scan. Treatment typically includes medications to thin the blood or placement of a filter to prevent the movement of additional blood clots to the lungs. Rarely, drugs are used to dissolve the clot or a catheter-based procedure is done to remove or treat the clot directly. What is a pulmonary embolism? Blood can change from a free flowing fluid to a semi-solid gel (called a blood clot or thrombus) in a process known as coagulation. Coagulation is a normal process and necessary to stop bleeding and retain blood within the body's vessels if they are cut or injured. However, in some situations blood can abnormally clot (called a thrombosis) within the vessels of the body. In a condition called deep vein thrombosis, clots form in the deep veins of the body, usually in the legs. A blood clot that breaks free and travels through a blood vessel is called an embolism. -

Pulmonary Embolism in the First Trimester of Pregnancy
Obstetrics & Gynecology International Journal Case Report Open Access Pulmonary embolism in the first trimester of pregnancy Summary Volume 11 Issue 1 - 2020 Pulmonary embolism in the first trimester of pregnancy without a known medical history Orfanoudaki Irene M is a very rare complication, which if it is misdiagnosed and left untreated leads to sudden Obstetric Gynecology, University of Crete, Greece pregnancy-related death. The sings and symptoms in this trimester are no specific. The causes for pulmonary embolism are multifactorial but in the first trimester of pregnancy, Correspondence: Orfanoudaki Irene M, Obstetric the most important causes are hereditary factors. Many times the pregnant woman ignores Gynecology, University of Crete, Greece, 22 Archiepiskopou her familiar hereditary history and her hemostatic system is progressively activated for the Makariou Str, 71202, Heraklion, Crete, Greece, Tel +30 hemostatic challenge of pregnancy and delivery. The hemostatic changes produce enhance 6945268822, +302810268822, Email coagulation and formation of micro-thrombi or thrombi and prompt diagnosis is crucial to prevent and treat pulmonary embolism saving the lives of a pregnant woman and her fetus. Received: January 19, 2020 | Published: January 28, 2020 Keywords: pregnancy, pulmonary embolism, mortality, diagnosis, risk factors, arterial blood gases, electrocardiogram, ventilation perfusion scan, computed tomography pulmonary angiogram, magnetic resonanance, compression ultrasonography, echocardiogram, D-dimers, troponin, brain -

Pulmonary Embolism
Pulmonary Embolism Pulmonary Embolism (PE) is the blockage of one or more arteries in the lungs, ultimately eliminating the oxygen supply causing heart failure. This can take place when a blood clot from another area of the body, most often from the legs, breaks free, enters the blood stream and gets trapped in the lung's arteries. Once a clot is lodged in the artery of the lung, the tissue is then starved of fuel and may die (pulmonary infarct) or the blockage of blood flow may result in increased strain on the right side of the heart. It is estimated that approximately 600,000 patients suffer from pulmonary embolism each year in the US. Of these 600,000, 1/3 will die as a result. Deep Vein Thrombosis (DVT) is the most common precursor of pulmonary embolism. With early treatment of DVT, patients can reduce their chances of developing a life threatening pulmonary embolism to less than one percent. Early treatment with blood thinners is important to prevent a life-threatening pulmonary embolism, but does not treat the existing clot in the leg. Get more information on Deep Vein Thrombosis. Symptoms of PE Symptoms of pulmonary embolism can include shortness of breath; rapid pulse; sweating; sharp chest pain; bloody sputum (coughing up blood); and fainting. These symptoms are frequently nonspecific to pulmonary embolism and can mimic other cardiopulmonary events. Since pulmonary embolism can be life-threatening, if any of these symptoms are present please see your physician immediately. Treatments for PE Anticoagulation The first line of defense when treating pulmonary embolism is by using an anticoagulant. -

Status Epilepticus Due to Cerebral Air Embolism After the Valsalva Maneuver CASE REPORT
eISSN 2508-1349 J Neurocrit Care 2019;12(1):51-54 https://doi.org/10.18700/jnc.190075 Status epilepticus due to cerebral air embolism after the Valsalva maneuver CASE REPORT Hyun Ji Lyou, MD; Hye Jeong Lee, MD; Grace Yoojin Lee, MD; Received: March 11, 2019 Won-Joo Kim, MD, PhD Revised: May 3, 2019 Accepted: May 27, 2019 Department of Neurology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea Corresponding Author: Won-Joo Kim, MD Department of Neurology, Gangnam Severance Hospital, Yonsei University College of Medicine, 211 Eonju-ro, Gangnam-gu, Seoul 06273, Republic of Korea Tel: +82-2-2019-3324 Fax: +82-2-3462-5904 E-mail: [email protected] Background: Cerebral air embolism is uncommon but potentially causes catastrophic events such as cardiac damage or even death. However, due to a low overall incidence, it may go undiagnosed. Case Report: A 56-year-old man with a medical history of right upper lobectomy due to lung cancer showed changes in mental status after the Valsalva maneuver, followed by status epilepticus during admission. Brain and chest computed tomography showed cerebral air embolism and accidental pneumothorax in the right major fissure. After antiepileptic drug infusion and oxygen therapy, he recov- ered completely. Conclusion: Since cerebral air embolism may result in fatal outcomes, it should be suspected in patients with sudden neurological de- terioration after routine medical procedures. Keywords: Status epilepticus; Embolism, air; Pneumothorax; Valsalva maneuver INTRODUCTION CASE REPORT Cerebral air embolism is a rare but potentially severe complication A 56-year-old man with a medical history of right upper lobectomy of iatrogenic procedures or destructive lung disease, possibly re- due to lung cancer presented to the emergency room with changes sulting in neurological disorders such as encephalopathy, stroke, or in mental status after the Valsalva maneuver during a pulmonary seizure. -

Hypercoagulability in Hereditary Hemorrhagic Telangiectasia With
Published online: 2019-09-26 Case Report Hypercoagulability in hereditary hemorrhagic telangiectasia with epilepsy Josef Finsterer, Ernst Sehnal1 Departments of Neurological and 1Cardiology and Intensive Care Medicine, General Hospital Rudolfstiftung, Vienna, Austria, Europe ABSTRACT Recent data indicate that in patients with hereditary hemorrhagic teleangiectasia (HHT), low iron levels due to inadequate replacement after hemorrhagic iron losses are associated with elevated factor‑VIII plasma levels and consecutively increased risk of venous thrombo‑embolism. Here, we report a patient with HHT, low iron levels, elevated factor‑VIII, and recurrent venous thrombo‑embolism. A 64‑year‑old multimorbid Serbian gipsy was diagnosed with HHT at age 62 years. He had a history of recurrent epistaxis, teleangiectasias on the lips, renal and pulmonary arterio‑venous malformations, and a family history positive for HHT. He had experienced recurrent venous thrombosis (mesenteric vein thrombosis, portal venous thrombosis, deep venous thrombosis), insufficiently treated with phenprocoumon during 16 months and gastro‑intestinal bleeding. Blood tests revealed sideropenia and elevated plasma levels of coagulation factor‑VIII. His history was positive for diabetes, arterial hypertension, hyperlipidemia, smoking, cerebral abscess, recurrent ischemic stroke, recurrent ileus, peripheral arterial occluding disease, polyneuropathy, mild renal insufficiency, and epilepsy. Following recent findings, hypercoagulability was attributed to the sideropenia‑induced elevation -

A Practical Handbook on Pediatric Cardiac Intensive Care Therapy
A Practical Handbook on Pediatric Cardiac Intensive Care Therapy Dietrich Klauwer Christoph Neuhaeuser Josef Thul Rainer Zimmermann Editors 123 A Practical Handbook on Pediatric Cardiac Intensive Care Therapy Dietrich Klauwer · Christoph Neuhaeuser Josef Thul · Rainer Zimmermann Editors A Practical Handbook on Pediatric Cardiac Intensive Care Therapy Editors Dietrich Klauwer Christoph Neuhaeuser Center for Paediatrics and Youth Universitätsklinikum Gießen und Marburg Health Singen Paediatric Cardiac ICU and Heart Singen Transplantation Program Germany Gießen Germany Josef Thul Universitätsklinikum Gießen und Marburg Rainer Zimmermann Paediatric Cardiac ICU and Heart Global Medical Leader in Medical Affairs Transplantation Program Actelion Pharmaceuticals Gießen Allschwil Germany Switzerland Translation from the German language edition: Pädiatrische Intensivmedizin – Kinderkardiologische Praxis, 2. erw. Auflage by D. Klauwer / C. Neuhaeuser / J. Thul / R. Zimmermann, © Deutscher Ärzteverlag 2017 ISBN 978-3-319-92440-3 ISBN 978-3-319-92441-0 (eBook) https://doi.org/10.1007/978-3-319-92441-0 Library of Congress Control Number: 2018957468 © Springer International Publishing AG, part of Springer Nature 2019 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. -
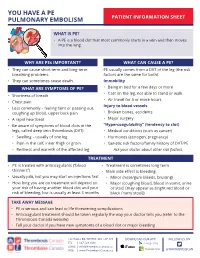
You Have a Pulmonary Embolism (PE)
YOU HAVE A PE PULMONARY EMBOLISM PATIENT INFORMATION SHEET WHAT IS PE? • A PE is a blood clot that most commonly starts in a vein and then moves into the lung. WHY ARE PEs IMPORTANT? WHAT CAN CAUSE A PE? • They can cause short term and long-term PE usually comes from a DVT of the leg (the risk breathing problems. factors are the same for both). • They can sometimes cause death. Immobility WHAT ARE SYMPTOMS OF PE? • Being in bed for a few days or more • Cast on the leg, not able to stand or walk • Shortness of breath • Air travel for 6 or more hours • Chest pain Injury to blood vessels • Less commonly – feeling faint or passing out, coughing up blood, upper back pain • Broken bones, accidents • A rapid heartbeat • Major surgery • Be aware of symptoms of blood clots in the “Hypercoagulability” (tendency to clot) legs, called deep vein thrombosis (DVT): • Medical conditions (such as cancer) • Swelling – usually of one leg • Hormones (estrogen, pregnancy) • Pain in the calf, inner thigh or groin • Genetic risk factors/family history of DVT/PE • Redness and warmth of the affected leg Ask your doctor about other risk factors. TREATMENT • PE is treated with anticoagulants (“blood • Treatment is sometimes long term thinners”) • Main side effect is bleeding: • Usually pills, but you may start on injections first • Minor (nose/gum bleeds, bruising) • How long you are on treatment will depend on • Major (coughing blood, blood in vomit, urine your risk of having another blood clot and your or stool [may appear as bright red blood or risk of bleeding, but is usually at least 3 months black / tarry stool]) TAKE AWAY MESSAGE • PE is serious and can lead to life threatening complications • Anticoagulant treatment should be taken regularly the way your doctor tells you (refer to the Thrombosis Canada website) • Tell your doctor if you have new symptoms of a blood clot or major bleeding 128 HALLS RD, WHITBY, ON, L1P 1Y8 DOWNLOAD OUR APP FOLLOW US ON TEL | 647-528-8586 EMAIL | [email protected] WEB | www.ThrombosisCanada.ca @THROMBOSISCAN. -

Heart Murmur Detection System
Heart Murmur Detection/ Classification using Cochlea-like Pre-processing A THESIS SUBMITTED TO THE FACULTY OF THE GRADUATE SCHOOL OF THE UNIVERSITY OF MINNESOTA BY Waqas Ahmad IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE Prof. M. Imran Hayee January 2010 © Waqas Ahmad 2010 Acknowledgements I would like to thank the Department of Electrical Engineering at the University of Minnesota Duluth (ECE at UMD) for providing me opportunity to research. I am indebted to ECE for continuously providing me support both in terms of moral and financial. I am also thankful to the University of Minnesota, School of Medicine Duluth (UMSMD) for the support in my research and experimentations. I want to extend my gratitude towards the very helpful and supportive teachers namely Dr. Stanley Burns, Dr. Glenn Nordehn, Dr. Todd Loushine, Dr. Mohammad Hassan and Dr. Jingshu Yang. Special thanks to Whiteside Institute at St. Luke‘s Hospital Duluth for generously providing the funding for this research work. My family, friends especially Nisar Ahmed, Scott Klar, office colleagues Shey Peterson, Kathy Bergh, Carol and Geni were very supportive to me I want to thank them for their encouragement throughout my stay here at UMD. Last but not the least, I want thank my advisor and mentor Dr. M Imran Hayee for his continuous guidance throughout the project and without which I would not be able to finish this research. I want to extend my thanks to the family of Dr. Imran Hayee namely his wife Hifsa Imran and kids Zarar and Shanze for inviting me to the dinner for numerous occasions. -

Takayasu's Arteritis Associated with Tuberculosis Infections Abstract
Case Report iMedPub Journals JOURNAL OF NEUROLOGY AND NEUROSCIENCE 2016 http://www.imedpub.com/ Vol.7 No.3:114 ISSN 2171-6625 DOI: 10.21767/2171-6625.1000114 Takayasu’s Arteritis associated with Tuberculosis Infections Reshkova V, Kalinova D and Rashkov R Clinic of Rheumatology, Medical University of Sofia, Sofia, Bulgaria Corresponding author: Dr. Valentina Reshkova, Clinic of Rheumatology, Medical University of Sofia, 13 Urvich Str, 1612, Sofia, Bulgaria, Tel: Tel: 359878622443; E-mail: [email protected] Received: May 05, 2016; Accepted: Jun 07, 2016; Published: Jun 10, 2016 grade fever which used to appear at evening and gradually Abstract became persistent. Physical examination revealed asthenic habit, enlarged Takayasu’s arteritis (TA) is an inflammatory disease of peripheral lymph nodes in the left axillary region-firm in unknown etiology characterized by granulomatous consistency, non-tender and not fixed with surrounding vasculitis affecting the aorta, its main branches and the structures. It was found pulse celer of the a. radialis dextra, pulmonary arteries. It occurs most often in women of diminished pulse of the a. radialis sinistra and the a. brachialis child-bearing age. At the time of diagnosis 10% to 20% of sinistra. Carotid pulses were presented without bruits. Blood patients with TA are clinically asymptomatic. The pressure measurements: in the right upper limb 120/80 remaining 80% to 90% of patients present with systemic mmHg, in the left upper limb 80/50 mmHg. Cardiac or vascular symptoms. The most important points in examination showed diastolic heart murmur over the right diagnosing Takayasu’s arteritis are the clinical features, second intercostal space, systolic fremisman over 2nd and 3rd physical examination and diagnostic imaging (catheter- left intercostal space, systolic murmur over the left sternal directed dye arteriography, magnetic resonance border. -

Real-World Data from the Gemelli Hospital HHT Registry
Journal of Clinical Medicine Article Antithrombotic Therapy in Hereditary Hemorrhagic Telangiectasia: Real-World Data from the Gemelli Hospital HHT Registry Eleonora Gaetani 1,2,*, Fabiana Agostini 1,2, Igor Giarretta 1,2 , Angelo Porfidia 1,3 , Luigi Di Martino 1,2, Antonio Gasbarrini 1,2, Roberto Pola 1,4 1, and on behalf of the Multidisciplinary Gemelli Hospital Group for HHT y 1 Multidisciplinary Gemelli Hospital Group for HHT, Fondazione Policlinico Universitario A. Gemelli IRCCS Università Cattolica del Sacro Cuore, 00168 Rome, Italy; [email protected] (F.A.); [email protected] (I.G.); angelo.porfi[email protected] (A.P.); [email protected] (L.D.M.); [email protected] (A.G.); [email protected] (R.P.) 2 Department of Translational Medicine and Surgery, Fondazione Policlinico Universitario A. Gemelli IRCCS Università Cattolica del Sacro Cuore, 00168 Rome, Italy 3 Division of Internal Medicine, Fondazione Policlinico Universitario A. Gemelli IRCCS Università Cattolica del Sacro Cuore, 00168 Rome, Italy 4 Department of Cardiovascular Sciences, Fondazione Policlinico Universitario A. Gemelli IRCCS Università Cattolica del Sacro Cuore, 00168 Rome, Italy * Correspondence: [email protected]; Tel.: +39-06-30157075 Multidisciplinary Gemelli Hospital Group for HHT: Giulio C. Passali, Maria E. Riccioni, Annalisa Tortora, y Veronica Ojetti, Daniela Feliciani, Leonardo Stella, Clara De Simone, Luigi Corina, Alfredo Puca, Carmelo L. Sturiale, Laura Riccardi, Aldobrando Broccolini, Carmine Di StasiAndrea Contegiacomo, Annemilia Del Ciello, Pietro M. Ferraro, Emanuela Lucci-Cordisco, Giuseppe Zampino, Valentina Giorgio, Giuseppe Marrone, Gabriele Spoletini, Gabriella Locorotondo, Gaetano Lanza, Erica De Candia, Elisabetta Peppucci, Marianna Mazza, Giuseppe Marano, Maria T. Lombardi, Maria G. -

Guidelines for the Use of Echocardiography in the Evaluation of a Cardiac Source of Embolism
ASE GUIDELINES AND STANDARDS Guidelines for the Use of Echocardiography in the Evaluation of a Cardiac Source of Embolism Muhamed Saric, MD, PhD, FASE, Chair, Alicia C. Armour, MA, BS, RDCS, FASE, M. Samir Arnaout, MD, Farooq A. Chaudhry, MD, FASE, Richard A. Grimm, DO, FASE, Itzhak Kronzon, MD, FASE, Bruce F. Landeck, II, MD, FASE, Kameswari Maganti, MD, FASE, Hector I. Michelena, MD, FASE, and Kirsten Tolstrup, MD, FASE, New York, New York; Durham, North Carolina; Beirut, Lebanon; Cleveland, Ohio; Aurora, Colorado; Chicago, Illinois; Rochester, Minnesota; and Albuquerque, New Mexico Embolism from the heart or the thoracic aorta often leads to clinically significant morbidity and mortality due to transient ischemic attack, stroke or occlusion of peripheral arteries. Transthoracic and transesophageal echo- cardiography are the key diagnostic modalities for evaluation, diagnosis, and management of stroke, systemic and pulmonary embolism. This document provides comprehensive American Society of Echocardiography guidelines on the use of echocardiography for evaluation of cardiac sources of embolism. It describes general mechanisms of stroke and systemic embolism; the specific role of cardiac and aortic sour- ces in stroke, and systemic and pulmonary embolism; the role of echocardiography in evaluation, diagnosis, and management of cardiac and aortic sources of emboli including the incremental value of contrast and 3D echocardiography; and a brief description of alternative imaging techniques and their role in the evaluation of cardiac sources of emboli. Specific guidelines are provided for each category of embolic sources including the left atrium and left atrial appendage, left ventricle, heart valves, cardiac tumors, and thoracic aorta. In addition, there are recommen- dation regarding pulmonary embolism, and embolism related to cardiovascular surgery and percutaneous procedures.