DRUG NAME: Megestrol
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
PMBJP Product.Pdf
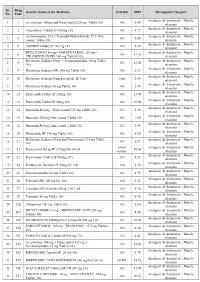
Sr. Drug Generic Name of the Medicine Unit Size MRP Therapeutic Category No. Code Analgesic & Antipyretic / Muscle 1 1 Aceclofenac 100mg and Paracetamol 325 mg Tablet 10's 10's 8.00 relaxants Analgesic & Antipyretic / Muscle 2 2 Aceclofenac Tablets IP 100mg 10's 10's 4.37 relaxants Acetaminophen 325 + Tramadol Hydrochloride 37.5 film Analgesic & Antipyretic / Muscle 3 4 10's 8.00 coated Tablet 10's relaxants Analgesic & Antipyretic / Muscle 4 5 ASPIRIN Tablets IP 150 mg 14's 14's 2.70 relaxants DICLOFENAC 50 mg+ PARACETAMOL 325 mg+ Analgesic & Antipyretic / Muscle 5 6 10's 11.30 CHLORZOXAZONE 500 mg Tablets 10's relaxants Diclofenac Sodium 50mg + Serratiopeptidase 10mg Tablet Analgesic & Antipyretic / Muscle 6 8 10's 12.00 10's relaxants Analgesic & Antipyretic / Muscle 7 9 Diclofenac Sodium (SR) 100 mg Tablet 10's 10's 6.12 relaxants Analgesic & Antipyretic / Muscle 8 10 Diclofenac Sodium 25mg per ml Inj. IP 3 ml 3 ml 2.00 relaxants Analgesic & Antipyretic / Muscle 9 11 Diclofenac Sodium 50 mg Tablet 10's 10's 2.90 relaxants Analgesic & Antipyretic / Muscle 10 12 Etoricoxilb Tablets IP 120mg 10's 10's 33.00 relaxants Analgesic & Antipyretic / Muscle 11 13 Etoricoxilb Tablets IP 90mg 10's 10's 25.00 relaxants Analgesic & Antipyretic / Muscle 12 14 Ibuprofen 400 mg + Paracetamol 325 mg Tablet 10's 15's 5.50 relaxants Analgesic & Antipyretic / Muscle 13 15 Ibuprofen 200 mg film coated Tablet 10's 10's 1.80 relaxants Analgesic & Antipyretic / Muscle 14 16 Ibuprofen 400 mg film coated Tablet 10's 15's 3.50 relaxants Analgesic & Antipyretic -

Megestrol Acetate/Melengestrol Acetate 2115 Adverse Effects and Precautions Megestrol Acetate Is Also Used in the Treatment of Ano- 16
Megestrol Acetate/Melengestrol Acetate 2115 Adverse Effects and Precautions Megestrol acetate is also used in the treatment of ano- 16. Mwamburi DM, et al. Comparing megestrol acetate therapy with oxandrolone therapy for HIV-related weight loss: similar As for progestogens in general (see Progesterone, rexia and cachexia (see below) in patients with cancer results in 2 months. Clin Infect Dis 2004; 38: 895–902. p.2125). The weight gain that may occur with meges- or AIDS. The usual dose is 400 to 800 mg daily, as tab- 17. Grunfeld C, et al. Oxandrolone in the treatment of HIV-associ- ated weight loss in men: a randomized, double-blind, placebo- trol acetate appears to be associated with an increased lets or oral suspension. A suspension of megestrol ace- controlled study. J Acquir Immune Defic Syndr 2006; 41: appetite and food intake rather than with fluid reten- tate that has an increased bioavailability is also availa- 304–14. tion. Megestrol acetate may have glucocorticoid ef- ble (Megace ES; Par Pharmaceutical, USA) and is Hot flushes. Megestrol has been used to treat hot flushes in fects when given long term. given in a dose of 625 mg in 5 mL daily for anorexia, women with breast cancer (to avoid the potentially tumour-stim- cachexia, or unexplained significant weight loss in pa- ulating effects of an oestrogen—see Malignant Neoplasms, un- Effects on carbohydrate metabolism. Megestrol therapy der Precautions of HRT, p.2075), as well as in men with hot 1-3 4 tients with AIDS. has been associated with hyperglycaemia or diabetes mellitus flushes after orchidectomy or anti-androgen therapy for prostate in AIDS patients being treated for cachexia. -

Us Anti-Doping Agency
2019U.S. ANTI-DOPING AGENCY WALLET CARDEXAMPLES OF PROHIBITED AND PERMITTED SUBSTANCES AND METHODS Effective Jan. 1 – Dec. 31, 2019 CATEGORIES OF SUBSTANCES PROHIBITED AT ALL TIMES (IN AND OUT-OF-COMPETITION) • Non-Approved Substances: investigational drugs and pharmaceuticals with no approval by a governmental regulatory health authority for human therapeutic use. • Anabolic Agents: androstenediol, androstenedione, bolasterone, boldenone, clenbuterol, danazol, desoxymethyltestosterone (madol), dehydrochlormethyltestosterone (DHCMT), Prasterone (dehydroepiandrosterone, DHEA , Intrarosa) and its prohormones, drostanolone, epitestosterone, methasterone, methyl-1-testosterone, methyltestosterone (Covaryx, EEMT, Est Estrogens-methyltest DS, Methitest), nandrolone, oxandrolone, prostanozol, Selective Androgen Receptor Modulators (enobosarm, (ostarine, MK-2866), andarine, LGD-4033, RAD-140). stanozolol, testosterone and its metabolites or isomers (Androgel), THG, tibolone, trenbolone, zeranol, zilpaterol, and similar substances. • Beta-2 Agonists: All selective and non-selective beta-2 agonists, including all optical isomers, are prohibited. Most inhaled beta-2 agonists are prohibited, including arformoterol (Brovana), fenoterol, higenamine (norcoclaurine, Tinospora crispa), indacaterol (Arcapta), levalbuterol (Xopenex), metaproternol (Alupent), orciprenaline, olodaterol (Striverdi), pirbuterol (Maxair), terbutaline (Brethaire), vilanterol (Breo). The only exceptions are albuterol, formoterol, and salmeterol by a metered-dose inhaler when used -

U.S. Medical Eligibility Criteria for Contraceptive Use, 2016
Morbidity and Mortality Weekly Report Recommendations and Reports / Vol. 65 / No. 3 July 29, 2016 U.S. Medical Eligibility Criteria for Contraceptive Use, 2016 U.S. Department of Health and Human Services Centers for Disease Control and Prevention Recommendations and Reports CONTENTS Introduction ............................................................................................................1 Methods ....................................................................................................................2 How to Use This Document ...............................................................................3 Keeping Guidance Up to Date ..........................................................................5 References ................................................................................................................8 Abbreviations and Acronyms ............................................................................9 Appendix A: Summary of Changes from U.S. Medical Eligibility Criteria for Contraceptive Use, 2010 ...........................................................................10 Appendix B: Classifications for Intrauterine Devices ............................. 18 Appendix C: Classifications for Progestin-Only Contraceptives ........ 35 Appendix D: Classifications for Combined Hormonal Contraceptives .... 55 Appendix E: Classifications for Barrier Methods ..................................... 81 Appendix F: Classifications for Fertility Awareness–Based Methods ..... 88 Appendix G: Lactational -

Combined Estrogen–Progestogen Menopausal Therapy
COMBINED ESTROGEN–PROGESTOGEN MENOPAUSAL THERAPY Combined estrogen–progestogen menopausal therapy was considered by previous IARC Working Groups in 1998 and 2005 (IARC, 1999, 2007). Since that time, new data have become available, these have been incorporated into the Monograph, and taken into consideration in the present evaluation. 1. Exposure Data 1.1.2 Progestogens (a) Chlormadinone acetate Combined estrogen–progestogen meno- Chem. Abstr. Serv. Reg. No.: 302-22-7 pausal therapy involves the co-administration Chem. Abstr. Name: 17-(Acetyloxy)-6-chlo- of an estrogen and a progestogen to peri- or ropregna-4,6-diene-3,20-dione menopausal women. The use of estrogens with IUPAC Systematic Name: 6-Chloro-17-hy- progestogens has been recommended to prevent droxypregna-4,6-diene-3,20-dione, acetate the estrogen-associated risk of endometrial Synonyms: 17α-Acetoxy-6-chloro-4,6- cancer. Evidence from the Women’s Health pregnadiene-3,20-dione; 6-chloro-Δ6-17- Initiative (WHI) of adverse effects from the use acetoxyprogesterone; 6-chloro-Δ6-[17α] of a continuous combined estrogen–progestogen acetoxyprogesterone has affected prescribing. Patterns of exposure Structural and molecular formulae, and relative are also changing rapidly as the use of hormonal molecular mass therapy declines, the indications are restricted, O CH and the duration of the therapy is reduced (IARC, 3 C 2007). CH3 CH3 O C 1.1 Identification of the agents CH3 H O 1.1.1 Estrogens HH For Estrogens, see the Monograph on O Estrogen-only Menopausal Therapy in this Cl volume. C23H29ClO4 Relative molecular mass: 404.9 249 IARC MONOGRAPHS – 100A (b) Cyproterone acetate Structural and molecular formulae, and relative Chem. -

Role of Androgens, Progestins and Tibolone in the Treatment of Menopausal Symptoms: a Review of the Clinical Evidence
REVIEW Role of androgens, progestins and tibolone in the treatment of menopausal symptoms: a review of the clinical evidence Maria Garefalakis Abstract: Estrogen-containing hormone therapy (HT) is the most widely prescribed and well- Martha Hickey established treatment for menopausal symptoms. High quality evidence confi rms that estrogen effectively treats hot fl ushes, night sweats and vaginal dryness. Progestins are combined with School of Women’s and Infants’ Health The University of Western Australia, estrogen to prevent endometrial hyperplasia and are sometimes used alone for hot fl ushes, King Edward Memorial Hospital, but are less effective than estrogen for this purpose. Data are confl icting regarding the role of Subiaco, Western Australia, Australia androgens for improving libido and well-being. The synthetic steroid tibolone is widely used in Europe and Australasia and effectively treats hot fl ushes and vaginal dryness. Tibolone may improve libido more effectively than estrogen containing HT in some women. We summarize the data from studies addressing the effi cacy, benefi ts, and risks of androgens, progestins and tibolone in the treatment of menopausal symptoms. Keywords: androgens, testosterone, progestins, tibolone, menopause, therapeutic Introduction Therapeutic estrogens include conjugated equine estrogens, synthetically derived piperazine estrone sulphate, estriol, dienoestrol, micronized estradiol and estradiol valerate. Estradiol may also be given transdermally as a patch or gel, as a slow release percutaneous implant, and more recently as an intranasal spray. Intravaginal estrogens include topical estradiol in the form of a ring or pessary, estriol in pessary or cream form, dienoestrol and conjugated estrogens in the form of creams. In some countries there is increasing prescribing of a combination of estradiol, estrone, and estriol as buccal lozenges or ‘troches’, which are formulated by private compounding pharmacists. -

Periodic Hypokalaemic Paralysis, Adrenal Adenoma, and Normal Colonic Transport of Sodium and Potassium
Gut: first published as 10.1136/gut.14.6.478 on 1 June 1973. Downloaded from Gut, 1973, 14, 478-484 Periodic hypokalaemic paralysis, adrenal adenoma, and normal colonic transport of sodium and potassium PETER RICHARDS1, M. B. S. JONES, AND W. S. PEART From the Medical Unit, St Mary's Hospital Medical School, London SUMMARY A 47-year-old woman was cured of hypokalaemia and recurrent paralysis by the excision of an adrenal adenoma. Hypertension was initially ameliorated but was not cured. Suppression of plasma renin activity was abolished when the adenoma was excised. Repeated measurement of plasma corticosteroids before operation showed a slight increase in aldosterone and normal plasma concentrations of deoxycorticosterone, corticosterone, and cortisol. No evidence of excess mineralo- corticoid was obtained from measurement of the electrolyte composition of colonic fluid or of rectal potential difference, although both these variables responded normally to salt depletion and exogenous aldosterone. The diagnostic importance of the paradoxically normal colonic measure- ments is emphasized and the possibility is considered that the adenoma may have secreted an unidentified hormone. http://gut.bmj.com/ The colon normally responds to excessive plasma not escape from the action of these hormones. One concentrations of aldosterone, corticosterone, and patient has been described in whom colonic sodium deoxycorticosterone by modifying faecal fluid so fluxes were apparently normal and were unchanged that the concentration of sodium is very low and that by the excision of an aldosterone-secreting adrenal of potassium high (Wrong, Morrison, and Hurst, adenoma; potassium influx was nevertheless in- 1961; Wrong and Metcalfe-Gibson, 1965; creased and returned to normal after operation Richards, on September 29, 2021 by guest. -

The Role of Highly Selective Androgen Receptor (AR) Targeted
P h a s e I I S t u d y o f I t r a c o n a z o l e i n B i o c h e m i c a l R e l a p s e Version 4.0: October 8, 2014 CC# 125513 CC# 125513: Hedgehog Inhibition as a Non-Castrating Approach to Hormone Sensitive Prostate Cancer: A Phase II Study of Itraconazole in Biochemical Relapse Investigational Agent: Itraconazole IND: IND Exempt (IND 116597) Protocol Version: 4.0 Version Date: October 8, 2014 Principal Investigator: Rahul Aggarwal, M.D., HS Assistant Clinical Professor Division of Hematology/Oncology, Department of Medicine University of California San Francisco 1600 Divisadero St. San Francisco, CA94115 [email protected] UCSF Co-Investigators: Charles J. Ryan, M.D., Eric Small, M.D., Professor of Medicine Professor of Medicine and Urology Lawrence Fong, M.D., Terence Friedlander, M.D., Professor in Residence Assistant Clinical Professor Amy Lin, M.D., Associate Clinical Professor Won Kim, M.D., Assistant Clinical Professor Statistician: Li Zhang, Ph.D, Biostatistics Core RevisionHistory October 8, 2014 Version 4.0 November 18, 2013 Version 3.0 January 28, 2013 Version 2.0 July 16, 2012 Version 1.0 Phase II - Itraconazole Page 1 of 79 P h a s e I I S t u d y o f I t r a c o n a z o l e i n B i o c h e m i c a l R e l a p s e Version 4.0: October 8, 2014 CC# 125513 Protocol Signature Page Protocol No.: 122513 Version # and Date: 4.0 - October 8, 2014 1. -

Hormonal and Non-Hormonal Management of Vasomotor Symptoms: a Narrated Review
Central Journal of Endocrinology, Diabetes & Obesity Review Article Corresponding authors Orkun Tan, Department of Obstetrics and Gynecology, Division of Reproductive Endocrinology Hormonal and Non-Hormonal and Infertility, University of Texas Southwestern Medical Center, 5323 Harry Hines Blvd. Dallas, TX 75390 and ReproMed Fertility Center, 3800 San Management of Vasomotor Jacinto Dallas, TX 75204, USA, Tel: 214-648-4747; Fax: 214-648-8066; E-mail: [email protected] Submitted: 07 September 2013 Symptoms: A Narrated Review Accepted: 05 October 2013 Orkun Tan1,2*, Anil Pinto2 and Bruce R. Carr1 Published: 07 October 2013 1Department of Obstetrics and Gynecology, Division of Reproductive Endocrinology Copyright and Infertility, University of Texas Southwestern Medical Center, USA © 2013 Tan et al. 2Department of Obstetrics and Gynecology, Division of Reproductive Endocrinology and Infertility, ReproMed Fertility Center, USA OPEN ACCESS Abstract Background: Vasomotor symptoms (VMS; hot flashes, hot flushes) are the most common complaints of peri- and postmenopausal women. Therapies include various estrogens and estrogen-progestogen combinations. However, both physicians and patients became concerned about hormone-related therapies following publication of data by the Women’s Health Initiative (WHI) study and have turned to non-hormonal approaches of varying effectiveness and risks. Objective: Comparison of the efficacy of non-hormonal VMS therapies with estrogen replacement therapy (ERT) or ERT combined with progestogen (Menopausal Hormone Treatment; MHT) and the development of literature-based guidelines for the use of hormonal and non-hormonal VMS therapies. Methods: Pubmed, Cochrane Controlled Clinical Trials Register Database and Scopus were searched for relevant clinical trials that provided data on the treatment of VMS up to June 2013. -

Order in Council 1243/1995
PROVINCE OF BRITISH COLUMBIA ORDER OF THE LIEUTENANT GOVERNOR IN COUNCIL Order in Council No. 12 4 3 , Approved and Ordered OCT 121995 Lieutenant Governor Executive Council Chambers, Victoria On the recommendation of the undersigned, the Lieutenant Governor, by and with the advice and consent of the Executive Council, orders that Order in Council 1039 made August 17, 1995, is rescinded. 2. The Drug Schedules made by regulation of the Council of the College of Pharmacists of British Columbia, as set out in the attached resolution dated September 6, 1995, are hereby approved. (----, c" g/J1"----c- 4- Minister of Heal fandand Minister Responsible for Seniors Presidin Member of the Executive Council (This pan is for adnwustratlye purposes only and is not part of the Order) Authority under which Order Is made: Act and section:- Pharmacists, Pharmacy Operations and Drug Scheduling Act, section 59(2)(1), 62 Other (specify): - Uppodukoic1enact N6145; Resolution of the Council of the College of Pharmacists of British Columbia ("the Council"), made by teleconference at Vancouver, British Columbia, the 6th day of September 1995. RESOLVED THAT: In accordance with the authority established in Section 62 of the Pharmacists, Pharmacy Operations and Drug Scheduling Act of British Columbia, S.B.C. Chapter 62, the Council makes the Drug Schedules by regulation as set out in the attached schedule, subject to the approval of the Lieutenant Governor in Council. Certified a true copy Linda J. Lytle, Phr.) Registrar DRUG SCHEDULES to the Pharmacists, Pharmacy Operations and Drug Scheduling Act of British Columbia The Drug Schedules have been printed in an alphabetical format to simplify the process of locating each individual drug entry and determining its status in British Columbia. -

Medication Use for the Risk Reduction of Primary Breast Cancer in Women: a Systematic Review for the U.S
Evidence Synthesis Number 180 Medication Use for the Risk Reduction of Primary Breast Cancer in Women: A Systematic Review for the U.S. Preventive Services Task Force Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 5600 Fishers Lane Rockville, MD 20857 www.ahrq.gov Contract No. HHSA-290-2015-00009-I, Task Order No. 7 Prepared by: Pacific Northwest Evidence-Based Practice Center Oregon Health & Science University Mail Code: BICC 3181 SW Sam Jackson Park Road Portland, OR 97239 www.ohsu.edu/epc Investigators: Heidi D. Nelson, MD, MPH Rongwei Fu, PhD Bernadette Zakher, MBBS Marian McDonagh, PharmD Miranda Pappas, MA L.B. Miller, BA Lucy Stillman, BS AHRQ Publication No. 19-05249-EF-1 January 2019 This report is based on research conducted by the Pacific Northwest Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (HHSA-290-2015-00009-I, Task Order No. 7). The findings and conclusions in this document are those of the authors, who are responsible for its contents, and do not necessarily represent the views of AHRQ. Therefore, no statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help health care decisionmakers—patients and clinicians, health system leaders, and policymakers, among others—make well-informed decisions and thereby improve the quality of health care services. This report is not intended to be a substitute for the application of clinical judgment. -

Treatment of Cushing's Disease
D CUEVAS-RAMOS and M FLESERIU Treatment of Cushing’s disease 223:2 R19–R39 Review Treatment of Cushing’s disease: a mechanistic update Daniel Cuevas-Ramos1,2 and Maria Fleseriu3 1Department of Medicine, Pituitary Center, Cedars-Sinai Medical Center, Los Angeles, California, USA Correspondence 2Neuroendocrinology Clinic, Department of Endocrinology and Metabolism, Instituto Nacional de Ciencias should be addressed Me´ dicas y Nutricio´ n Salvador Zubira´ n, Mexico City, Mexico to M Fleseriu 3Departments of Medicine and Neurological Surgery, and Northwest Pituitary Center, Oregon Health & Science Email University, 3181 SW Sam Jackson Park Road (BTE 472), Portland, Oregon 97239, USA fl[email protected] Abstract Cushing’s disease (CD) is characterized by an ACTH-producing anterior corticotrope pituitary Key Words adenoma. If hypothalamus–pituitary–adrenal (HPA) axis physiology is disrupted, ACTH " cortisol secretion increases, which in turn stimulates adrenocortical steroidogenesis and cortisol " Cushing’s disease production. Medical treatment plays an important role for patients with persistent disease " ACTH after surgery, for those in whom surgery is not feasible, or while awaiting effects of " pasireotide radiation. Multiple drugs, with different mechanisms of action and variable efficacy and " mifepristone tolerability for controlling the deleterious effects of chronic glucocorticoid excess, are " ketoconazole available. The molecular basis and clinical data for centrally acting drugs, adrenal " LCI699 steroidogenesis inhibitors, and glucocorticoid receptor antagonists are reviewed, as are " cabergoline potential novel molecules and future possible targets for CD treatment. Although progress has been made in the understanding of specific corticotrope adenoma receptor physiology Journal of Endocrinology and recent clinical studies have detected improved effects with a combined medical therapy approach, there is a clear need for a more efficacious and better-tolerated medical therapy for patients with CD.