Why D-Neuron? Direction from Psychiatric Research
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Neurotransmitter Resource Guide
NEUROTRANSMITTER RESOURCE GUIDE Science + Insight doctorsdata.com Doctor’s Data, Inc. Neurotransmitter RESOURCE GUIDE Table of Contents Sample Report Sample Report ........................................................................................................................................................................... 1 Analyte Considerations Phenylethylamine (B-phenylethylamine or PEA) ................................................................................................. 1 Tyrosine .......................................................................................................................................................................................... 3 Tyramine ........................................................................................................................................................................................4 Dopamine .....................................................................................................................................................................................6 3, 4-Dihydroxyphenylacetic Acid (DOPAC) ............................................................................................................... 7 3-Methoxytyramine (3-MT) ............................................................................................................................................... 9 Norepinephrine ........................................................................................................................................................................ -

Is TAAR1 a Potential Therapeutic Target for Immune Dysregulation In
Graduate Physical and Life Sciences PhD Pharmacology Abstract ID# 1081 Is TAAR1 a Potential Therapeutic Target for Immune Dysregulation in Drug Abuse? Fleischer, Lisa M; Tamashunas, Nina and Miller, Gregory M Addiction Sciences Laboratory, Northeastern University, Boston MA 02115 Abstract Discovered in 2001, Trace Amine Associated Receptor 1 (TAAR1) is a direct target of Data and Results amphetamine, methamphetamine and MDMA. It is expressed in the brain reward circuity and modulates dopamine transporter function and dopamine neuron firing rates. Newly-developed compounds that specifically target TAAR1 have recently been investigated in animal models In addition to brain, TAAR1 is expressed in immune cells METH promotes PKA and PKC Phosphorylation through TAAR1 as candidate therapeutics for methamphetamine, cocaine and alcohol abuse. These studies • We treated HEK/TAAR1 cells and HEK293 involving classic behavioral measures of drug response, as well as drug self-administration, Rhesus and Human cells with vehicle or METH, with and without strongly implicate TAAR1 as a potential therapeutic target for the treatment of addiction. In activators and inhibitors of PKA and PKC. addition to its central actions, we demonstrated that TAAR1 is upregulated in peripheral blood Cells Lines mononuclear cells (PBMC) and B cells following immune activation, and that subsequent • We performed Western blotting experiments to activation of TAAR1 by methamphetamine stimulates cAMP, similar to the function of measure levels of phospho-PKA and phospho- adenosine A2 receptors which are also present in immune cells and play a critical role in the PKC. immune response. Here, we are investigating the relationship between TAAR1 and the • We found that specific activators of PKA and adenosine A2 receptor at the level of cellular signaling and receptor dimerization. -
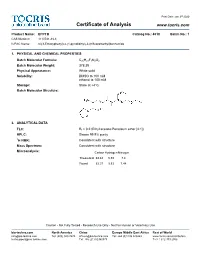
Certificate of Analysis
Print Date: Jan 3rd 2020 Certificate of Analysis www.tocris.com Product Name: EPPTB Catalog No.: 4518 Batch No.: 1 CAS Number: 1110781-88-8 IUPAC Name: N-(3-Ethoxyphenyl)-4-(1-pyrrolidinyl)-3-(trifluoromethyl)benzamide 1. PHYSICAL AND CHEMICAL PROPERTIES Batch Molecular Formula: C20H21F3N2O2 Batch Molecular Weight: 378.39 Physical Appearance: White solid Solubility: DMSO to 100 mM ethanol to 100 mM Storage: Store at +4°C Batch Molecular Structure: 2. ANALYTICAL DATA TLC: Rf = 0.2 (Ethyl acetate:Petroleum ether [4:1]) HPLC: Shows 99.9% purity 1H NMR: Consistent with structure Mass Spectrum: Consistent with structure Microanalysis: Carbon Hydrogen Nitrogen Theoretical 63.48 5.59 7.4 Found 63.37 5.53 7.44 Caution - Not Fully Tested • Research Use Only • Not For Human or Veterinary Use bio-techne.com North America China Europe Middle East Africa Rest of World [email protected] Tel: (800) 343 7475 [email protected] Tel: +44 (0)1235 529449 www.tocris.com/distributors [email protected] Tel: +86 (21) 52380373 Tel:+1 612 379 2956 Print Date: Jan 3rd 2020 Product Information www.tocris.com Product Name: EPPTB Catalog No.: 4518 Batch No.: 1 CAS Number: 1110781-88-8 IUPAC Name: N-(3-Ethoxyphenyl)-4-(1-pyrrolidinyl)-3-(trifluoromethyl)benzamide Description: Storage: Store at +4°C Trace amine 1 (TA ) receptor antagonist/inverse agonist; 1 Solubility & Usage Info: exhibits a higher potency at the mouse TA1 receptor than the rat DMSO to 100 mM and human TA150 receptors (IC values are 27.5, 4539 and 7487 ethanol to 100 mM nM, respectively). -

Modulation by Trace Amine-Associated Receptor 1 of Experimental Parkinsonism, L-DOPA Responsivity, and Glutamatergic Neurotransmission
The Journal of Neuroscience, October 14, 2015 • 35(41):14057–14069 • 14057 Neurobiology of Disease Modulation by Trace Amine-Associated Receptor 1 of Experimental Parkinsonism, L-DOPA Responsivity, and Glutamatergic Neurotransmission Alexandra Alvarsson,1* Xiaoqun Zhang,1* Tiberiu L Stan,1 Nicoletta Schintu,1 Banafsheh Kadkhodaei,2 Mark J. Millan,3 Thomas Perlmann,2,4 and Per Svenningsson1 1Department of Clinical Neuroscience, Center for Molecular Medicine, Karolinska Institutet, SE-17176 Stockholm, Sweden, 2Ludwig Institute for Cancer Research, SE-17177 Stockholm, Sweden, 3Pole of Innovation in Neuropsychiatry, Institut de Recherches Servier, Centre de Recherches de Croissy, Paris 87290, France, and 4Department of Cell and Molecular Biology, Karolinska Institutet, SE-17177 Stockholm, Sweden Parkinson’s disease (PD) is a movement disorder characterized by a progressive loss of nigrostriatal dopaminergic neurons. Restoration of dopamine transmission by L-DOPA relieves symptoms of PD but causes dyskinesia. Trace Amine-Associated Receptor 1 (TAAR1) modulates dopaminergic transmission, but its role in experimental Parkinsonism and L-DOPA responses has been neglected. Here, we report that TAAR1 knock-out (KO) mice show a reduced loss of dopaminergic markers in response to intrastriatal 6-OHDA administra- tion compared with wild-type (WT) littermates. In contrast, the TAAR1 agonist RO5166017 aggravated degeneration induced by intra- striatal6-OHDAinWTmice.Subchronic L-DOPAtreatmentofTAAR1KOmiceunilaterallylesionedwith6-OHDAinthemedialforebrain bundle resulted in more pronounced rotational behavior and dyskinesia than in their WT counterparts. The enhanced behavioral sensitization to L-DOPA in TAAR1 KO mice was paralleled by increased phosphorylation of striatal GluA1 subunits of AMPA receptors. Conversely, RO5166017 counteracted both L-DOPA-induced rotation and dyskinesia as well as AMPA receptor phosphorylation. -

Decarboxylation What Is Decarboxylation?
Decarboxylation What is decarboxylation? Decarboxylation is the removal of a carboxyl group when a compound is exposed to light or heat. A carboxyl group is a grouping of carbon, oxygen, and hydrogen atoms in the form of COOH. When a compound is decarboxylated, this group is released in the form of carbon dioxide. Decarboxylation of cannabinoids When considering the decarboxylation of cannabinoids, it is important to note that this reaction is what causes the neutral acidic cannabinoids to turn into the active cannabinoids found in most products on the market. Both the neutral and acidic cannabinoids are naturally found in the cannabis plant. The active cannabinoids that have psychoactive properties are what occur after decarboxylation. Below is the mechanism for the conversion of THCA to THC. https://www.leafscience.com/2017/04/13/what-is-thca/ Heating THCA converts it to THC by kicking off the carboxyl group seen on the right side of the THCA molecule. Once the carboxyl group is released from the THCA it forms carbon dioxide and the THC compound. The THC is now ready for use in different products and will provide the psychoactive effects that popularized this compound. This simple reaction is all it takes to convert the acidic cannabinoids to their active counterparts. Cannabinolic acid (CBDA) and CBD are both another example of this process. Decarboxylation process Light can start the decarboxylation process after a period of time, but heat is the more common element used. There are different methods to decarboxylate cannabis depending on user preference. In the industry, dabs, vapes and joints decarboxylate instantly when heat is applied to the product. -

Optimization of the Decarboxylation Reaction in Cannabis
APPLICATION NOTE FT-IR Spectroscopy Authors: Dr. Markus Roggen1 Antonio M. Marelli1 Doug Townsend2 Ariel Bohman2 1Outco SanDiego, CA 2PerkinElmer, Inc. Shelton, CT. Optimization of the Decarboxylation Reaction Introduction The production of cannabis in Cannabis Extract extracts and oils for medicinal and recreational products has increased significantly in North America. This growth has been driven by both market demand in newly legalized states and patient demand for a greater diversity in cannabis products.1,2,3 Most cannabis extraction processes, independent of solvent or instrument choice, undergo a decarboxylation step whereby the carboxylic acid functional group is removed from the cannabinoids. The decarboxylation reaction converts the naturally occurring acid forms of the cannabinoids, e.g. tetrahydrocannabinolic acid (THCA) and cannabidiolic acid (CBDA), to their more potent neutral forms, e.g. tetrahydrocannabinol (THC) and cannabidiol (CBD). Because the carboxylic acid group is thermally labile, the industry typically applies a heat source, and at times a catalyst, to decarboxylate the cannabinoids. The heat-promoted decarboxylation reaction has been Decarboxylation Reaction discussed at length within the industry, but an extensive Decarboxylation was achieved by heating the cannabis extract in 4, 5, 6 literature search reveals very few papers on the process. a oil bath with a programmable hot plate. An overhead stirrer The data available represents a large spectrum of reaction was utilized to promote even heat distribution throughout the conditions, including a range in reaction temperature, time experiment. Oil bath and extract temperatures were recorded and instrumental setup. As such, there is a lack of universal every five minutes throughout the 80-minute heating process. -

Effects of the Trace Amine Associated Receptor 1 Agonist RO5263397 On
International Journal of Neuropsychopharmacology, 2015, 1–7 doi:10.1093/ijnp/pyu060 Research Article research article Effects of the Trace Amine Associated Receptor 1 Agonist RO5263397 on Abuse-Related Behavioral Indices of Methamphetamine in Rats Li Jing, PhD; Yanan Zhang, PhD; Jun-Xu Li, PhD Department of Pharmacology and Toxicology, School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, NY (Drs Jing and Li); Department of Physiology and Pathophysiology, Tianjin Medical University, Tianjin, China (Dr Jing); Research Triangle Institute, Research Triangle Park, NC (Dr Zhang). Correspondence: Jun-Xu Li, PhD, Department of Pharmacology and Toxicology, School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, NY ([email protected]). Abstract Background: Methamphetamine is a major drug of abuse with no effective pharmacotherapy available. Trace amine associated receptor 1 is implicated in cocaine addiction and represents a potential therapeutic target. However, the effects of trace amine associated receptor 1 agonists on addiction-related behavioral effects of methamphetamine are unknown. Methods: This study examined the effects of a trace amine associated receptor 1 agonist RO5263397 on methamphetamine- induced behavioral sensitization, methamphetamine self-administration, cue- and methamphetamine-induced reinstatement of drug seeking, and cue-induced reinstatement of sucrose-seeking behaviors in rats. Male Sprague-Dawley rats were used to examine the effects of methamphetamine alone and in combination with the trace amine associated receptor 1 agonist RO5263397 (3.2–10 mg/kg). Results: RO5263397 dose-dependently attenuated the expression of behavioral sensitization to methamphetamine, reduced methamphetamine self-administration, and decreased both cue- and a priming dose of methamphetamine-induced reinstatement of drug-seeking behaviors. -

Catecholamine Levels and Activity of Monoamine Oxidase in Some Hypothalamic Structures and in the Pineal Gland of Sheep After Administration of FSH
Physiol. Res. 45:131-136, 1996 Catecholamine Levels and Activity of Monoamine Oxidase in Some Hypothalamic Structures and in the Pineal Gland of Sheep after Administration of FSH B. PASTOROVA, J. VARADY Department of Comparative Physiology , University of Veterinary Medicine, Kosice, Slovak Republic Receded March 6, 1995 Accepted November 13, 1995 Summary The influence of hormonal preparations of FSH in a dose of 24 mg (480 IU) on levels of catecholamine (dopamine, norepinephrine and epinephrine) and the activity of their degradation enzyme monoamine oxidase (MAO) in the hypothalamic regions regulating the reproductive system of sheep (area preoptica, eminentia mediana, corpus mamillare) and pineal gland were investigated in the ocstrous period employing radiochemical methods. The administration of FSH resulted in significant (p<0.001) increases of dopamine levels in the area preoptica and corpus mamillare of the hypothalamus of sheep as compared to control groups with synchronized oestrus. Hormonal stimulation with FSH increased the levels of hypothalamic norepinephrine in the areas studied and these differences were significant in the eminentia mediana (p<0.05) and corpus mamillare (p<0.05). Significant (p<0.001) changes in epinephrine levels were found in the corpus mamillare and area preoptica (p<0.05). Our results indicate that the administration of FSH caused the most pronounced decrease of MAO activity in corpus mamillare (p<0.001). The pineal gland reacted to the hormonal preparation by decreased levels of norepinephrine and dopamine (p<0.001) and by an increase in MAO activity (p<0.01). We suggest that FSH administration affects catecholamine levels and the activity of monoamine oxidase in the studied areas of the brain of sheep by means of a feedback mechanism. -

Citric Acid Cycle
CHEM464 / Medh, J.D. The Citric Acid Cycle Citric Acid Cycle: Central Role in Catabolism • Stage II of catabolism involves the conversion of carbohydrates, fats and aminoacids into acetylCoA • In aerobic organisms, citric acid cycle makes up the final stage of catabolism when acetyl CoA is completely oxidized to CO2. • Also called Krebs cycle or tricarboxylic acid (TCA) cycle. • It is a central integrative pathway that harvests chemical energy from biological fuel in the form of electrons in NADH and FADH2 (oxidation is loss of electrons). • NADH and FADH2 transfer electrons via the electron transport chain to final electron acceptor, O2, to form H2O. Entry of Pyruvate into the TCA cycle • Pyruvate is formed in the cytosol as a product of glycolysis • For entry into the TCA cycle, it has to be converted to Acetyl CoA. • Oxidation of pyruvate to acetyl CoA is catalyzed by the pyruvate dehydrogenase complex in the mitochondria • Mitochondria consist of inner and outer membranes and the matrix • Enzymes of the PDH complex and the TCA cycle (except succinate dehydrogenase) are in the matrix • Pyruvate translocase is an antiporter present in the inner mitochondrial membrane that allows entry of a molecule of pyruvate in exchange for a hydroxide ion. 1 CHEM464 / Medh, J.D. The Citric Acid Cycle The Pyruvate Dehydrogenase (PDH) complex • The PDH complex consists of 3 enzymes. They are: pyruvate dehydrogenase (E1), Dihydrolipoyl transacetylase (E2) and dihydrolipoyl dehydrogenase (E3). • It has 5 cofactors: CoASH, NAD+, lipoamide, TPP and FAD. CoASH and NAD+ participate stoichiometrically in the reaction, the other 3 cofactors have catalytic functions. -

Lecture: 28 TRANSAMINATION, DEAMINATION and DECARBOXYLATION
Lecture: 28 TRANSAMINATION, DEAMINATION AND DECARBOXYLATION Protein metabolism is a key physiological process in all forms of life. Proteins are converted to amino acids and then catabolised. The complete hydrolysis of a polypeptide requires mixture of peptidases because individual peptidases do not cleave all peptide bonds. Both exopeptidases and endopeptidases are required for complete conversion of protein to amino acids. Amino acid metabolism The amino acids not only function as energy metabolites but also used as precursors of many physiologically important compounds such as heme, bioactive amines, small peptides, nucleotides and nucleotide coenzymes. In normal human beings about 90% of the energy requirement is met by oxidation of carbohydrates and fats. The remaining 10% comes from oxidation of the carbon skeleton of amino acids. Since the 20 common protein amino acids are distinctive in terms of their carbon skeletons, amino acids require unique degradative pathway. The degradation of the carbon skeletons of 20 amino acids converges to just seven metabolic intermediates namely. i. Pyruvate ii. Acetyl CoA iii. Acetoacetyl CoA iv. -Ketoglutarate v. Succinyl CoA vi. Fumarate vii. Oxaloacetate Pyruvate, -ketoglutarate, succinyl CoA, fumarate and oxaloacetate can serve as precursors for glucose synthesis through gluconeogenesis.Amino acids giving rise to these intermediates are termed as glucogenic. Those amino acids degraded to yield acetyl CoA or acetoacetate are termed ketogenic since these compounds are used to synthesize ketone bodies. Some amino acids are both glucogenic and ketogenic (For example, phenylalanine, tyrosine, tryptophan and threonine. Catabolism of amino acids The important reaction commonly employed in the breakdown of an amino acid is always the removal of its -amino group. -

Tyramine and Amyloid Beta 42: a Toxic Synergy
biomedicines Article Tyramine and Amyloid Beta 42: A Toxic Synergy Sudip Dhakal and Ian Macreadie * School of Science, RMIT University, Bundoora, VIC 3083, Australia; [email protected] * Correspondence: [email protected]; Tel.: +61-3-9925-6627 Received: 5 May 2020; Accepted: 27 May 2020; Published: 30 May 2020 Abstract: Implicated in various diseases including Parkinson’s disease, Huntington’s disease, migraines, schizophrenia and increased blood pressure, tyramine plays a crucial role as a neurotransmitter in the synaptic cleft by reducing serotonergic and dopaminergic signaling through a trace amine-associated receptor (TAAR1). There appear to be no studies investigating a connection of tyramine to Alzheimer’s disease. This study aimed to examine whether tyramine could be involved in AD pathology by using Saccharomyces cerevisiae expressing Aβ42. S. cerevisiae cells producing native Aβ42 were treated with different concentrations of tyramine, and the production of reactive oxygen species (ROS) was evaluated using flow cytometric cell analysis. There was dose-dependent ROS generation in wild-type yeast cells with tyramine. In yeast producing Aβ42, ROS levels generated were significantly higher than in controls, suggesting a synergistic toxicity of Aβ42 and tyramine. The addition of exogenous reduced glutathione (GSH) was found to rescue the cells with increased ROS, indicating depletion of intracellular GSH due to tyramine and Aβ42. Additionally, tyramine inhibited the respiratory growth of yeast cells producing GFP-Aβ42, while there was no growth inhibition when cells were producing GFP. Tyramine was also demonstrated to cause increased mitochondrial DNA damage, resulting in the formation of petite mutants that lack respiratory function. -

Biogenic Amine Reference Materials
Biogenic Amine reference materials Epinephrine (adrenaline), Vanillylmandelic acid (VMA) and homovanillic norepinephrine (noradrenaline) and acid (HVA) are end products of catecholamine metabolism. Increased urinary excretion of VMA dopamine are a group of biogenic and HVA is a diagnostic marker for neuroblastoma, amines known as catecholamines. one of the most common solid cancers in early childhood. They are produced mainly by the chromaffin cells in the medulla of the adrenal gland. Under The biogenic amine, serotonin, is a neurotransmitter normal circumstances catecholamines cause in the central nervous system. A number of disorders general physiological changes that prepare the are associated with pathological changes in body for fight-or-flight. However, significantly serotonin concentrations. Serotonin deficiency is raised levels of catecholamines and their primary related to depression, schizophrenia and Parkinson’s metabolites ‘metanephrines’ (metanephrine, disease. Serotonin excess on the other hand is normetanephrine, and 3-methoxytyramine) are attributed to carcinoid tumours. The determination used diagnostically as markers for the presence of of serotonin or its metabolite 5-hydroxyindoleacetic a pheochromocytoma, a neuroendocrine tumor of acid (5-HIAA) is a standard diagnostic test when the adrenal medulla. carcinoid syndrome is suspected. LGC Quality - ISO Guide 34 • GMP/GLP • ISO 9001 • ISO/IEC 17025 • ISO/IEC 17043 Reference materials Product code Description Pack size Epinephrines and metabolites TRC-E588585 (±)-Epinephrine