Why Do I Still Have Difficulty Breathing?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Captive Orcas
Captive Orcas ‘Dying to Entertain You’ The Full Story A report for Whale and Dolphin Conservation Society (WDCS) Chippenham, UK Produced by Vanessa Williams Contents Introduction Section 1 The showbiz orca Section 2 Life in the wild FINgerprinting techniques. Community living. Social behaviour. Intelligence. Communication. Orca studies in other parts of the world. Fact file. Latest news on northern/southern residents. Section 3 The world orca trade Capture sites and methods. Legislation. Holding areas [USA/Canada /Iceland/Japan]. Effects of capture upon remaining animals. Potential future capture sites. Transport from the wild. Transport from tank to tank. “Orca laundering”. Breeding loan. Special deals. Section 4 Life in the tank Standards and regulations for captive display [USA/Canada/UK/Japan]. Conditions in captivity: Pool size. Pool design and water quality. Feeding. Acoustics and ambient noise. Social composition and companionship. Solitary confinement. Health of captive orcas: Survival rates and longevity. Causes of death. Stress. Aggressive behaviour towards other orcas. Aggression towards trainers. Section 5 Marine park myths Education. Conservation. Captive breeding. Research. Section 6 The display industry makes a killing Marketing the image. Lobbying. Dubious bedfellows. Drive fisheries. Over-capturing. Section 7 The times they are a-changing The future of marine parks. Changing climate of public opinion. Ethics. Alternatives to display. Whale watching. Cetacean-free facilities. Future of current captives. Release programmes. Section 8 Conclusions and recommendations Appendix: Location of current captives, and details of wild-caught orcas References The information contained in this report is believed to be correct at the time of last publication: 30th April 2001. Some information is inevitably date-sensitive: please notify the author with any comments or updated information. -

The Use of Non-Human Primates in Research in Primates Non-Human of Use The
The use of non-human primates in research The use of non-human primates in research A working group report chaired by Sir David Weatherall FRS FMedSci Report sponsored by: Academy of Medical Sciences Medical Research Council The Royal Society Wellcome Trust 10 Carlton House Terrace 20 Park Crescent 6-9 Carlton House Terrace 215 Euston Road London, SW1Y 5AH London, W1B 1AL London, SW1Y 5AG London, NW1 2BE December 2006 December Tel: +44(0)20 7969 5288 Tel: +44(0)20 7636 5422 Tel: +44(0)20 7451 2590 Tel: +44(0)20 7611 8888 Fax: +44(0)20 7969 5298 Fax: +44(0)20 7436 6179 Fax: +44(0)20 7451 2692 Fax: +44(0)20 7611 8545 Email: E-mail: E-mail: E-mail: [email protected] [email protected] [email protected] [email protected] Web: www.acmedsci.ac.uk Web: www.mrc.ac.uk Web: www.royalsoc.ac.uk Web: www.wellcome.ac.uk December 2006 The use of non-human primates in research A working group report chaired by Sir David Weatheall FRS FMedSci December 2006 Sponsors’ statement The use of non-human primates continues to be one the most contentious areas of biological and medical research. The publication of this independent report into the scientific basis for the past, current and future role of non-human primates in research is both a necessary and timely contribution to the debate. We emphasise that members of the working group have worked independently of the four sponsoring organisations. Our organisations did not provide input into the report’s content, conclusions or recommendations. -

Slipping Rib Syndrome
Slipping Rib Syndrome Jackie Dozier, BS Edited by Lisa E McMahon, MD FACS FAAP David M Notrica, MD FACS FAAP Case Presentation AA is a 12 year old female who presented with a 7 month history of right-sided chest/rib pain. She states that the pain was not preceded by trauma and she had never experienced pain like this before. She has been seen in the past by her pediatrician, chiropractor, and sports medicine physician for her pain. In May 2012, she was seen in the ER after having manipulations done on her ribs by a sports medicine physician. Pain at that time was constant throughout the day and kept her from sleeping. However, it was relieved with hydrocodone/acetaminophen in the ER. Case Presentation Over the following months, the pain became progressively worse and then constant. She also developed shortness of breath. She is a swimmer and says she has had difficulty practicing due to the pain and SOB. AA was seen by a pediatric surgeon and scheduled for an interventional pain management service consult for a test injection. Following good temporary relief by local injection, she was scheduled costal cartilage removal to treat her pain. What is Slipping Rib Syndrome? •Slipping Rib Syndrome (SRS) is caused by hypermobility of the anterior ends of the false rib costal cartilages, which leads to slipping of the affected rib under the superior adjacent rib. •SRS an lead to irritation of the intercostal nerve or strain of the muscles surrounding the rib. •SRS is often misdiagnosed and can lead to months or years of unresolved abdominal and/or thoracic pain. -

Signs and Symptoms of COPD
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES Signs and Symptoms of COPD Chronic obstructive pulmonary disease (COPD) can cause shortness of breath, tiredness, Short ness of Breath production of mucus, and cough. Many people with COPD develop most if not all, of these signs Avo iding Activities and symptoms. Sho rtness wit of Breath h Man s Why is shortness of breath a symptom of COPD? y Activitie Shortness of breath (or breathlessness) is a common Avoiding symptom of COPD because the obstruction in the A breathing tubes makes it difficult to move air in and ny Activity out of your lungs. This produces a feeling of difficulty breathing (See ATS Patient Information Series fact sheet Shor f B tness o on Breathlessness). Unfortunately, people try to avoid this reath Sitting feeling by becoming less and less active. This plan may or Standing work at first, but in time it leads to a downward spiral of: avoiding activities which leads to getting out of shape or becoming deconditioned, and this can result in even more Is tiredness a symptom of COPD? shortness of breath with activity (see diagram). Tiredness (or fatigue) is a common symptom in COPD. What can I do to treat shortness of breath? Tiredness may discourage you from keeping active, which leads to greater loss of energy, which then leads to more If your shortness of breath is from COPD, you can do several tiredness. When this cycle begins it is sometimes hard to things to control it: break. CLIP AND COPY AND CLIP ■■ Take your medications regularly. -

Pneumonia: Prevention and Care at Home
FACT SHEET FOR PATIENTS AND FAMILIES Pneumonia: Prevention and Care at Home What is it? On an x-ray, pneumonia usually shows up as Pneumonia is an infection of the lungs. The infection white areas in the affected part of your lung(s). causes the small air sacs in your lungs (called alveoli) to swell and fill up with fluid or pus. This makes it harder for you to breathe, and usually causes coughing and other symptoms that sap your energy and appetite. How common and serious is it? Pneumonia is fairly common in the United States, affecting about 4 million people a year. Although for many people infection can be mild, about 1 out of every 5 people with pneumonia needs to be in the heart hospital. Pneumonia is most serious in these people: • Young children (ages 2 years and younger) • Older adults (ages 65 and older) • People with chronic illnesses such as diabetes What are the symptoms? and heart disease Pneumonia symptoms range in severity, and often • People with lung diseases such as asthma, mimic the symptoms of a bad cold or the flu: cystic fibrosis, or emphysema • Fatigue (feeling tired and weak) • People with weakened immune systems • Cough, without or without mucus • Smokers and heavy drinkers • Fever over 100ºF or 37.8ºC If you’ve been diagnosed with pneumonia, you should • Chills, sweats, or body aches take it seriously and follow your doctor’s advice. If your • Shortness of breath doctor decides you need to be in the hospital, you will receive more information on what to expect with • Chest pain or pain with breathing hospital care. -
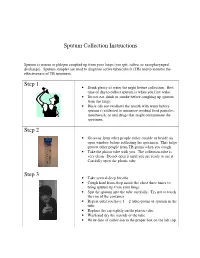
Sputum Collection Instructions Step 1 Step 2 Step 3
Sputum Collection Instructions Sputum is mucus or phlegm coughed up from your lungs (not spit, saliva, or nasopharyngeal discharge). Sputum samples are used to diagnose active tuberculosis (TB) and to monitor the effectiveness of TB treatment. Step 1 • Drink plenty of water the night before collection. Best time of day to collect sputum is when you first wake. • Do not eat, drink or smoke before coughing up sputum from the lungs. • Rinse (do not swallow) the mouth with water before sputum is collected to minimize residual food particles, mouthwash, or oral drugs that might contaminate the specimen. Step 2 • Go away from other people either outside or beside an open window before collecting the specimen. This helps protect other people from TB germs when you cough. • Take the plastic tube with you. The collection tube is very clean. Do not open it until you are ready to use it. Carefully open the plastic tube. Step 3 • Take several deep breaths. • Cough hard from deep inside the chest three times to bring sputum up from your lungs. • Spit the sputum into the tube carefully. Try not to touch the rim of the container. • Repeat until you have 1 – 2 tablespoons of sputum in the tube. • Replace the cap tightly on the plastic tube. • Wash and dry the outside of the tube. • Write date of collection in the proper box on the lab slip. Step 4 • Place the primary specimen container (usually a conical centrifuge tube) in the clear plastic baggie that has the biohazard symbol imprint. • Place the white absorbent sheet in the plastic baggie. -

Perinatal/Neonatal Case Presentation
Perinatal/Neonatal Case Presentation &&&&&&&&&&&&&& Urinary Tract Infection With Trichomonas vaginalis in a Premature Newborn Infant and the Development of Chronic Lung Disease David J. Hoffman, MD vaginal bleeding with suspected abruption resulted in delivery of Gerard D. Brown, DO the infant by Cesarean section. The Apgar scores were 1, 5, and 9 Frederick H. Wirth, MD at 1, 5, and 10 minutes of life, respectively. Betsy S. Gebert, CRNP After delivery, the infant was managed with mechanical Cathy L. Bailey, MS, CRNP ventilation with pressure support and volume guarantee for Endla K. Anday, MD respiratory distress syndrome. She received exogenous surfactant We report a case of a low-birth-weight infant with an infection of the urinary tract with Trichomonas vaginalis, who later developed cystic chronic lung disease suggestive of Wilson-Mikity syndrome. Although she had mild respiratory distress syndrome at birth, the extent of the chronic lung disease was out of proportion to the initial illness. We speculate that maternal infection with this organism may have resulted in an inflammatory response that led to its development. Journal of Perinatology (2003) 23, 59 – 61 doi:10.1038/sj.jp.7210819 CASE PRESENTATION A 956-g, appropriate-for-gestational-age, African–American female was delivered by Cesarean section following 27 5/7 weeks of gestation in breech presentation after a period of advanced cervical dilatation and uterine contractions. Her mother was a 20-year-old gravida 5, para 2022 woman whose prenatal laboratory data were significant for vaginal colonization with Streptococcus agalactiae, treatment for Chlamydia trachomatis, and a history of cocaine and marijuana usage confirmed by urine toxicology. -

Guinea Pig Care
Caring for your Guinea Pig Basic HusBandry General Information Vital Statistics Guinea Pig Body Weight: Male 900g–1,2000g; Female 700–900g Life Span: Average 4–5 years; Maximum 8 years Sexual Maturity: Male 3–4 months of age; Female 2–3 months of age Behavior and Handling • Guinea pigs should be held gently with two hands. Their hind end should always be supported. • When handling guinea pigs, try to avoid excessive noise, needless excitement, and over-handling. • Children handling the guinea pig should sit on the floor and hold the guinea pig in their lap. Children should only handle guinea pigs under adult supervision. • Guinea pigs do not adapt well to changes in their food or environment. Hair barbering (chewing of the fur) may occur in situations of stress and overcrowding. If this occurs please contact your veterinarian. Reproductive Information • It is extremely important not to let your female guinea pig breed as she reaches six months of age. At around this age, the bones of the pelvis fuse if the animal has not been bred. If a guinea pig in this condition becomes pregnant, she will most likely require high risk surgery to remove the babies. • Guinea pigs are social animals and will establish a pecking order that is frequently male-dominated. Overcrowding may incite aggression among guinea pigs, and noncastrated males may be aggressive towards other males in the presence of females. • Guinea pigs should be kept as single pets, or should be kept in separate cages. Housing • Guinea pigs should be housed separately in a cage that is a minimum of 2 ft. -

Factors Associated with Pleurisy in Pigs: a Case-Control Analysis of Slaughter Pig Data for England and Wales
Aus dem Zentrum für Klinische Tiermedizin der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Arbeit angefertigt unter der Leitung von Prof. Dr. Mathias Ritzmann Angefertigt am Cambridge Infectious Diseases Consortium, University of Cambridge, Department of Veterinary Medicine, Cambridge, UK (Dr. A W (Dan) Tucker) Factors associated with pleurisy in pigs: A case-control analysis of slaughter pig data for England and Wales Inaugural-Dissertation zur Erlangung der tiermedizinischen Doktorwürde der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Von Henrike Caroline Jäger aus Wiesbaden München 2012 Gedruckt mit der Genehmigung der Tierärztlichen Fakultät der Ludwig-Maximilians-Universität München Dekan: Univ.-Prof. Dr. Joachim Braun Berichterstatter: Univ.-Prof. Dr. Mathias Ritzmann Korreferent: Univ.-Prof. Dr. Dr. habil. Manfred Gareis Tag der Promotion: 9. Februar 2013 Meinem Vater Dr. med Sepp-Dietrich Jäger Table of Contents 4 TABLE OF CONTENTS I. INTRODUCTION ...................................................................................... 7 II. LITERATURE OVERVIEW .................................................................... 8 1. Anatomy and Physiology of the Pleura ....................................................8 2. Pleurisy ........................................................................................................9 2.1. Morphology ..................................................................................................9 2.2. Prevalence ..................................................................................................11 -

Bovine Respiratory Disease & Diagnostic Veterinary Medicine
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Range Beef Cow Symposium Animal Science Department 2009 Bovine Respiratory Disease & Diagnostic Veterinary Medicine (Managing Respiratory Diseases in the Herd) Donald Montgomery Wyoming State Veterinary Laboratory, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/rangebeefcowsymp Part of the Animal Sciences Commons Montgomery, Donald, "Bovine Respiratory Disease & Diagnostic Veterinary Medicine (Managing Respiratory Diseases in the Herd)" (2009). Range Beef Cow Symposium. 280. https://digitalcommons.unl.edu/rangebeefcowsymp/280 This Article is brought to you for free and open access by the Animal Science Department at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Range Beef Cow Symposium by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Proceedings, The Range Beef Cow Symposium XXI December 1, 2 and 3 2009, Casper, WY Bovine Respiratory Disease & Diagnostic Veterinary Medicine (Managing Respiratory Diseases in the Herd) Donald Montgomery, DVM, PhD, Dipl ACVP Pathologist and Director, Wyoming State Veterinary Laboratory Year in and year out, diseases of the respiratory system are a major cause of illness and death in cattle from 6 weeks to two years of age. Sadly, this is as true today as it was 30 years ago despite development of new and improved vaccines, new broad spectrum antibiotics, and increased fundamental knowledge as to the cause of disease. WHY? I don‟t have the answer and I doubt if anyone does. As a pathologist, I often see firsthand the devastating effects that bacteria can have in the lungs of cattle that die from respiratory disease complex or shipping fever. -

Chest Pain in Pediatrics
PEDIATRIC CARDIOLOGY 0031-3955/99 $8.00 + .OO CHEST PAIN IN PEDIATRICS Keith C. Kocis, MD, MS Chest pain is an alarming complaint in children, leading an often frightened and concerned family to a pediatrician or emergency room and commonly to a subsequent referral to a pediatric cardiologist. Because of the well-known associ- ation of chest pain with significant cardiovascular disease and sudden death in adult patients, medical personnel commonly share heightened concerns over pediatric patients presenting with chest pain. Although the differential diagnosis of chest pain is exhaustive, chest pain in children is least likely to be cardiac in origin. Organ systems responsible for causing chest pain in children include*: Idiopathic (12%-85%) Musculoskeletal (15%-31%) Pulmonary (12%-21%) Other (4%-21%) Psychiatric (5%-17%) Gastrointestinal (4'/0-7%) Cardiac (4%4%) Furthermore, chest pain in the pediatric population is rareZy associated with life-threatening disease; however, when present, prompt recognition, diagnostic evaluation, and intervention are necessary to prevent an adverse outcome. This article presents a comprehensive list of differential diagnostic possibilities of chest pain in pediatric patients, discusses the common causes in further detail, and outlines a rational diagnostic evaluation and treatment plan. Chest pain, a common complaint of pediatric patients, is often idiopathic in etiology and commonly chronic in nature. In one study,67 chest pain accounted for 6 in 1000 visits to an urban pediatric emergency room. In addition, chest pain is the second most common reason for referral to pediatric cardiologist^.^, 23, 78 Chest pain is found equally in male and female patients, with an average *References 13, 17, 23, 27, 32, 35, 44, 48, 49, 63-67, 74, and 78. -

Breathing Better with a COPD Diagnosis
Difficulty Breathing Chronic Bronchitis Smoker’s Cough Chronic Coughing Wheezing Em- Chronic Obstructive Pulmonary Disease physema Shortness of Breath Feeling of Suffocation Excess Mucus Difficulty Breathing Chronic Bronchitis Smoker’s Cough Chronic Coughing Wheezing Emphysema Shor tness of Breath Feeling of Suffocation Excess Mucus Difficulty Breathing Chronic Bronchitis Smoker’s Cough Chronic Coughing Wheezing Emphysema Shortness of Breath Feeling of Suffocation Excess Mucus Difficulty Breathing Chronic Bronchitis Smoker’s Cough Chron- ic Coughing Wheezing Emphysema Shortness of Breath Feeling of Suffocation Excess Mu- cus DifficultyBreathing Breathing Chronic Bronchitis Better Smoker’s Cough Chronic Coughing Wheezing Emphysema Shortness of Breath Feeling of Suffocation Excess Mucus Difficulty Breathing Chronic Bronchitis Smoker’s Cough Chronic Coughing Wheezing Emphysema Shor tness of Breath Feeling of SuffocationWith Excess a COPDMucus Difficulty Diagnosis Breathing Chronic Bronchitis Smoker’s Cough Chronic Coughing Wheezing Emphysema Shortness of Breath Feeling of did you know? When COPD is severe, shortness of breath and other COPDdid you is the know? 4th leading cause of death in the symptomswhen you can get are in the diagnosed way of doing even the most UnitedCOPD States.is the 4th The leading disease cause kills ofmore death than in 120,000 basicwith tasks, copd such as doing light housework, taking a Americansthe United eachStates year—that’s and causes 1 serious, death every long-term 4 walk,There and are even many bathing things and that getting you can dressed. do to make minutes—anddisability. The causesnumber serious, of people long-term with COPDdisability. is COPDliving withdevelops COPD slowly, easier: and can worsen over time, increasing.The number More of people than 12with million COPD people is increasing.