Pt Orientation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Susan Horton
SUSAN HORTON September 2014 ADDRESS: University of Waterloo Waterloo, Ont N2L 3G1 Tel 519-888-4567 X 33560 Email [email protected] EDUCATION: 1977-1982 HARVARD UNIVERSITY Ph.D. in economics June 1982. Thesis: Labor use, nutrition and household behavior: Results from Western India. A.M. November 1981. 1974-1977 CAMBRIDGE UNIVERSITY, ENGLAND B.A. with first-class honors in economics June 1977. M.A. March 1981. RESEARCH INTERESTS: Health, nutrition, labour markets, social policy, particularly in developing countries. WORK EXPERIENCE: July 09 – present CIGI Chair in Global Health Economics, Balsillie School of International Affairs July 09- June 14 Associate Provost, Graduate Studies, University of Waterloo Aug 04- June 09 Vice-President Academic (to July 08) and Professor, Wilfrid Laurier University Sept 82- July 04 University of Toronto: Interim Vice-Principal (Academic) and Dean, University of Toronto at Scarborough (03-04); Chair, Division of Social Sciences, University of Toronto at Scarborough (00-03); Cross-appointed to Dept. of Public Health Sciences (98-04); Associate Dean, Social Sciences, Faculty of Arts and Science (95-96), Professor (95-06); Associate Professor (88-95), Assistant Professor (82-88) Undergraduate courses taught: micro, quantitative methods, development, agricultural economics, political economy of developing countries, labour economics, international health policy, international studies and international communications. Graduate courses taught: development economics, social policy analysis, international perspectives on health of women and children, health policy, economics of public health, international public policy Short courses: labour market institutions, economics of waste management. Supervisor of studies economics 1991-1994, and International Development Studies 1987-89, 1994-1996, 1997-2000. Supervisor, 8 PhD theses (4 completed); advisor, 7 PhD theses (7 completed), 1 MSc thesis (completed); advisor 2 MSc theses (completed). -
Community Profile
Economic Development Division City of Cambridge COMMUNITY PROFILE A Summary of Cambridge’s Economic and Social Features Office of the City Manager Economic Development Division Corporation of the City of Cambridge 50 Dickson Street, 2nd Floor, P.O. Box 669 Cambridge Ontario Canada N1R 5W8 Tel: (519) 740‐4683 Fax: (519) 740‐4512, www.cambridge.ca CAMBRIDGE COMMUNITY PROFILE CITY ECONOMIC OF 2 DEVELOPMENT CAMBRIDGE DIVISION CAMBRIDGE COMMUNITY PROFILE COMMUNITY PROFILE Introduction Cambridge is one of the fastest growing and strongest economic areas in Canada. Over the past ten years, on average, $244 million has been invested annually in building construction, with about one third towards the new residential sector. The average annual population growth rate is just over 1%, while the employment growth over the last census period has been 3% annually. Over the past five years, the establishment of business has increased 3.4% annually. Cambridge’s thriving business climate is why many businesses are choosing to locate and expand here. This booklet provides details on the community and many reasons why the City of Cambridge is your location for success. Economic Development Division The professional staff of the Economic Development Division is available to assist you with your business requirements. Whether you need specific detailed information about Cambridge to help you with your business‐decision making process or a tour of the community and its available “Sites and Buildings”, we are here to provide confidential and expert assistance. Our pro‐business attitude and attention to customer service will facilitate your business transactions with the City’s municipal offices. -

John Milloy Campaign
JohnRe-Elect Milloy On October 6th, experience and hard work matter. Authorized by the CFO for the John Milloy Campaign NAIL 2011 Provincial Kitchener Local PROBLEM? election bike sharing Marquetry KW’s Newest candidates' program artist paints Building Centre NO questionnaires rolling along PROBLEM! with wood is Here... Page 6 & 7 Page 10 Page 1 5 in Your Neighbourhood &KHFN XV RXW # New 10,000-sq. ft. Retail Store 58%< 1$,/6 5 Forwell Rd. off Victoria St. N )RU /DGLHV DQG *HQWOHPHQ SINCE 1923 (UE 6WUHHW :HVW :DWHUORR ZZZUXE\QDLOVFD &DOO 8V 519-745-3250 www.kitchenercitizen.com • Volume 3, 5 • Thurs. September 22, 201 1 • Circulation 31,500 www.boyerfence.com Beam from World Trade Center to rest at firefighter memorial the memorial, there are bronze helmets Linwood said most of the work for that was once a part of the World Trade BY HELEN HALL for each Kitchener firefighter who has getting the beam to Kitchener was done Center’s substructure. lost his life in the line of duty. Many by firefighter Kevin Schmalz. It took The beam made its first public itchener is one of a handful of cities in firefighters die from cancer and other more than a year of planning and appearance in Kitchener at Sportsworld KCanada that is home to a significant illnesses related to years of fighting fires. coordinating with the New York City Crossing on Sunday, August 21 when the piece of the World Trade Center. This October, a bronze helmet will be Port Authority to acquire the artifact Kitchener firefighters held a send-off for A 3,000 pound beam from the building added for Captain Bill Duncan, who ...continued on page 5 will be unveiled in a permanent died of brain cancer in 2011. -

Way to Go Breaststrokes
2nd Edition Winter 2008 Way To Go BreastStrokes Don McKenzie from the University of British Columbia has found through his research that repetitive upper-body exercise discourages lymphedema and improves the quality of life in women who have had breast cancer. The BreastStrokes team trains at Guelph Lake during warmer months and during the off-season team members continue to improve their fitness in the gym and pool at the University of Guelph. This team clearly demonstrates that breast cancer survivors are all winners and that there is ‘life after breast A local dragon boat team has made it their Dragon boating, the fastest growing team cancer’! mission to increase breast cancer awareness sport in the world, is a great way to build The University of Guelph – sponsored and to provide hope and support for those living camaraderie, find support and raise aware- BreastStrokes team was invited to compete in with the impact of breast cancer. The ness of important issues including breast the world dragon boat invitational held last BreastStrokes Dragon Boat team was formed in cancer. In addition to the many noted benefits 1998 when the Guelph and Wellington Breast of dragon boat racing it also offers many summer in Australia. Cancer Support Group decided to start paddling. unique benefits to breast cancer survivors. Dr. (Cont’d page 5) Welcome To The Second Issue The purpose of the newsletter is to provide linked to decreased risk of cancer; a forum for exchange of cancer prevention Wellington - Dufferin - Guelph world record World Record Walk Gets People and screening efforts in the Waterloo walk gets people in motion; Waterloo Wellington Regional Cancer Program and Wellington Breast Cancer Care Pathway Map Of All Ages in motion!2 beyond. -

Integrated Stroke Care in Waterloo-Wellington
Integrated Stroke Care in Waterloo-Wellington Transitions in Stroke Care Stroke Network of Southeastern Ontario September 18, 2019 Our Success • Stroke Care in Waterloo Wellington • 2017/2018 • All data referenced was abstracted through: • Discharge Abstract Data (DAD), accessed through Intellihealth Ontario • National Ambulatory Care Reporting System (NACRS), Accessed through Intellihealth Ontario • Home Care Database (HCD), Accessed through Intellihealth Ontario 2 Ontario Stroke 2017/2018 Report Card 3 2011/2012 Reports: • Identified Significant Gaps: 1. “Improving Access to Quality Stroke Care in • Access Waterloo-Wellington” • Patient Outcomes 2. “Transitioning to a System of Rehabilitative Care • System Efficiencies in Waterloo-Wellington” Our Path to an Aug, 2013 • Hospital Re-organization LHIN Integration • CCAC To Deliver Best Integrated Stroke Practice Stroke Care Order System • Waterloo Wellington Apr 1st, 2014 Stroke Steering Committee Integration of Stroke • Stroke Implementation Services Across the Task Force Continuum • Coordinated Bed Access Steering Committee Current Integrated Stroke System Committee Structure Waterloo Wellington Waterloo Stroke CS Regional Waterloo Wellington Community Home & Stroke Wellington Stroke Partners Community Monitoring & Rehabilitative Implementation Advisory Care Therapy Evaluation Care Council Task Force Committee Working Group Committee - Executive - Representation from - Representation from - Representation from - Waterloo Wellington leadership for WW hospital, H&CC, and community partners -

301 Streetcar Time Schedule & Line Route
301 streetcar time schedule & line map 301 Conestoga Station View In Website Mode The 301 streetcar line (Conestoga Station) has 2 routes. For regular weekdays, their operation hours are: (1) Conestoga Station: 5:30 AM - 11:35 PM (2) Fairway Station: 4:45 AM - 11:40 PM Use the Moovit App to ƒnd the closest 301 streetcar station near you and ƒnd out when is the next 301 streetcar arriving. Direction: Conestoga Station 301 streetcar Time Schedule 16 stops Conestoga Station Route Timetable: VIEW LINE SCHEDULE Sunday 7:00 AM - 11:30 PM Monday 5:30 AM - 11:35 PM Fairway Station Tuesday 5:30 AM - 11:35 PM Block Line Station 1099 Courtland Ave E, Waterloo Wednesday 5:30 AM - 11:35 PM Mill Station Thursday 5:30 AM - 11:35 PM 355 Ottawa St S, Waterloo Friday 5:30 AM - 11:35 PM Borden Station Saturday 6:00 AM - 11:30 PM 497 Charles St E, Waterloo Kitchener Market Station 210 Charles St E, Waterloo 301 streetcar Info Frederick Station Direction: Conestoga Station 15 Frederick St, Waterloo Stops: 16 Trip Duration: 45 min Kitchener City Hall Station Line Summary: Fairway Station, Block Line Station, 72 Duke St W, Waterloo Mill Station, Borden Station, Kitchener Market Station, Frederick Station, Kitchener City Hall Station, Central Station Central Station, Grand River Hospital Station (Lrt), 512 King St W, Waterloo Allen Station, Waterloo Public Square Station, Laurier-Waterloo Park Station, University Of Grand River Hospital Station (Lrt) Waterloo Station, Research & Technology Station, 876 King Street West, Waterloo Northƒeld Station, Conestoga -
King East Field Guide
DOWNTOWN KITCHENER / 2020 WELCOME TO THE NEIGHBOURHOOD You’ve found yourself in the heart of Waterloo Region. Downtown Kitchener (DTK) is bordered by 6 unique neighbourhoods, including: Victoria Park, Olde Berlin in the Civic District, Central Frederick, Cedar Hill, Auditorium and King East. This field guide highlights the King East Neighbourhood (also referred to as the Market District). Here you can find the most authentic international flavours, sustainable shopping, amazing diversity and welcoming people. It won’t take you long to find beauty here. This is a guide to the restaurants, events and hidden gems in the area. We couldn’t possibly fit all of the amazing places to see and things to do -- you’ll just have to get out there and see for yourself. YOU’RE GOING TO LOVE IT HERE. Here are some words GETTING AROUND likely to come across: DTK Downtown Kitchener PUBLIC TRANSIT GRT Grand River Transit, MAJOR STOPS TO HELP YOU GET AROUND: includes buses and the train: public Conestoga Station - Conestoga Mall transit for the Fairway Station - Fairview Mall Waterloo Region Waterloo Public Square Station - Uptown Waterloo KPL Kitchener Public Victoria Park Station - Victoria Park Library Frederick Station - Conestoga College Downtown Campus KW Kitchener-Waterloo, Kitchener Market Station - King East area two different cities that share resources Fairway Station transfer to Bus Route 201 to Conestoga College - through the Waterloo Conestoga Doon Campus Region, with Bus Route 8 (to University/King) - Conestoga Waterloo campus separate municipal governments GRT Customer service kiosk is for maps, passes, etc - King and Benton Street. LRT *GRT Grand River Transit for fares Light Rail Transit, & passes located at 105 King St. -
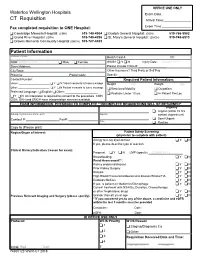
Waterloo Wellington Hospitals Exam Date:______CT Requisition Arrival Time:______
OFFICE USE ONLY Waterloo Wellington Hospitals Exam Date:________________ CT Requisition Arrival Time:_______________ Fax completed requisition to ONE Hospital: Exam Time:________________ o Cambridge Memorial Hospital: (CMH) 519-740-4904 o Guelph General Hospital: (GGH) 519-766-9982 o Grand River Hospital: (GRH) 519-749-4296 o St. Mary’s General Hospital: (SMGH) 519-749-6513 o Groves Memorial Community Hospital:(GMCH) 519-787-4405 Patient Information Last Name, First Name: Health Card #: VC: DOB: DD/MM/YYYY o Male o Female WSIB? o Y o N Injury Date: DD/MM/YYYY Street Address: Please include Claim #: _________________ City/Town: Other Insurance? Third Party or Self Pay Province: Postal Code: Specify: ___________________________________________ Contact Number: Required Patient Information: Home: _____________________ o Y o N Patient consents to leave message Height: ________(cm) Weight: _________(kg) o o Other: _____________________ Y N Patient consents to leave message o Restricted Mobility o Outpatient Preferred Language: o English o Other: ____________________ o Pediatric Under 10 yrs o In-Patient Rm/Loc o Y o N An interpreter is required to consent to the procedure. CMH, ______________________ GGH, GRH and SMGH have interpretation services available. EXAM INFORMATION: PHYSICIAN TO COMPLETE **INCOMPLETE REQUISITIONS WILL BE RETURNED” Urgency o Urgent (within 72 hrs Ordering Physician Name (Please print): Signature contact department) o Semi-Urgent Contact #: Fax#: Date o Routine Copy to (Please print) Region/Organ of Interest: Patient -
Embracing Challenge Innovating Change
Embracing Challenge Innovating Change STRATEGIC PRIORITIES FOR 2017-19 INNOVATIVE IDEAS. Bold commitments. Grand River Hospital’s new strategic Integration Network, St. Mary’s General plan for 2017-19 builds on our and Cambridge Memorial hospitals and achievements of past years and our Guelph Wellington hospital partners, family physicians and health teams as well challenges us to do even more. as community organizations whose work supports and enhances the patient and Our new plan sees us making bold family experience. commitments that will improve the care we provide each and every day at Grand River On the following pages you’ll learn more Hospital while actively participating in the about our priorities for the next two years evolution of our larger health care system. and beyond. You’ll also meet some of the visionaries, from the community and our Of course, a bold vision isn’t achieved hospital, who will challenge us and keep us without bold visionaries and support through focused on the important work that will improve important partnerships. Some of our partners care for patients across Waterloo Wellington. include the Waterloo Wellington Local Health EMBRACING CHALLENGE INNOVATING CHANGE | 3 Our focus FOR THE NEXT TWO YEARS Provide excellent care always Grand River Hospital’s leadership and dedicated physicians are Help to improve our health care system exploring the development of Improve care through research a neuroscience program for our and innovation community. This will leverage the work we are already doing Support our staff, physicians and volunteers in stroke, spinal surgery and Make it all possible interventional radiology while addressing the growing need for this kind of care close to home. -
Executive Summary
2012- Waterloo-Wellington Diabetes RCC Annual Report 2013 Executive Summary Debbie Hollahan, Regional Director Waterloo Wellington Diabetes Regional Coordination Centre January 31, 2013 Executive Summary 2012- 2013 Background The Waterloo Wellington Diabetes Regional Coordination Centre (DRCC) was established in 2010, through funding from the Ontario Diabetes Strategy with the Ministry of Health and Long Term Care (MOHLTC). Langs Farm Village Association (Langs) was selected as the host organization for the DRCC in Waterloo Wellington. The role of the DRCC is to provide regional leadership to integrate and coordinate diabetes care in the region of Waterloo-Wellington, including primary care, diabetes programs, endocrinologists, and the community. The DRCC works closely with the Local Health Integrated Network (LHIN) to provide a clear point of contact within each region for diabetes. The DRCC does not provide direct patient services, but drives the implementation of provincial priorities while monitoring regional performance. The goal of the DRCC is to improve the delivery of care for people and families living with diabetes. In 2010, a workplan was established in the form of a logic model, using the framework of the Chronic Disease Prevention and Management (CDPM) Framework (Fig. 1) and incorporating the principles from Health Quality Ontario—“Safe, integrated, Patient-Centred, Accessible, Equitable, Effective and Efficient”. The Ontario CDPM framework (Fig. 1) is a validated tool which provides a model for system planning for chronic disease prevention and management. The “bubbles” within the framework provide a structure for effective planning of activities. The following report is presented under headings that mirror this CDPM framework. Figure 1: Ontario CDPM Framework 2 | P a g e January 2013 Executive Summary 2012- 2013 For 2012-13, work continued, building on the successes to date, and focusing on the identified priorities established in the past year, with a greater focus on the social determinants of health. -
General Info GRRCC
General Information Grand River Regional Cancer Centre Address & Hours Grand River Regional Cancer Centre is a part of Grand River Hospital. Cancer Centre Hospital Address Registration Desk 835 King Street West Open Kitchener, Ontario Monday - Friday N2G 1G3 7:45am - 4:30pm Patient Call Centre After Hours Care (CareChart@home) 519-749-4380 Monday - Friday 1-877-681-3057 8:30am - 4pm Please note the centre is closed on weekends and on statutory holidays. If you need options on how to get to or from the hospital for your visits, speak to a member of your health care team. Where can I find… GRAND RIVER REGIONAL CANCER CENTRE • Registration • Resource Centre • Clinic D (Radiation Department) 3rd Floor • Supportive Care (Main Floor and Entrance • Clinic E & Nurse Assessment Clinic to Cancer Centre) • MPE Clinic • Lung Diagnostic Assessment Program (DAP) • Lab • Outpatient Oncology Pharmacy • Clinic A (Medical Oncology) 4th Floor • Clinic A+ (Medical Oncology) • Clinic B (Hematology) • Systemic Therapy Suite (Chemo Suite) • Inpatient Oncology 6th Floor • 6OC Treatment Area (outpatient appointments) GRAND RIVER HOSPITAL • Sanctuary • Cafeteria B • Grand River Hospital Pharmacy • Tim Hortons C • Medical Imaging (X-ray, Ultra Sound appointments) D • Hospital Inpatient Floors • 6th Floor Oncology Inpatient Unit • Main Elevator D/F • Gift Shop • Emergency • Security E • Parking Office Parking There are many places to park around the hospital and cancer centre including: 1. Main parking garage - on site at 835 King Street West, Kitchener 2. Pay & Display parking • Along the main entrance circle of Grand River Hospital • 40 Green Street (Kaufman Building) • Rotary lot on King Street (across from the Hospital) • Don McLaren Parking Lot (across from the Kaufman Building) If you will be making many visits you can buy a monthly parking pass. -
LOCAL APPENDICES to the COLLECTIVE AGREEMENT Between: GRAND RIVER HOSPITAL CORPORATION And: ONTARIO NURSES' ASSOCIATION Expiry
LOCAL APPENDICES TO THE COLLECTIVE AGREEMENT Between: GRAND RIVER HOSPITAL CORPORATION (Hereinafter referred to as “the Hospital”) And: ONTARIO NURSES’ ASSOCIATION (hereinafter referred to as “the Union”) Expiry: June 7, 2021 KITCH02.C21 TABLE OF CONTENTS Page APPENDIX 3 – SALARY SCHEDULE ........................................................................................ 1 APPENDIX 4 – SUPERIOR CONDITIONS – FREEPORT SITE ONLY ...................................... 4 APPENDIX 5 – LOCAL PROVISIONS ....................................................................................... 5 ARTICLE A – RECOGNITION ................................................................................................... 5 ARTICLE B – MANAGEMENT RIGHTS ..................................................................................... 5 ARTICLE C – ASSOCIATION SECURITY ................................................................................. 5 ARTICLE D – REPRESENTATIVES AND COMMITTEES ......................................................... 5 ARTICLE E – SENIORITY ......................................................................................................... 6 ARTICLE F – LEAVE OF ABSENCE ......................................................................................... 7 ARTICLE G – HOURS OF WORK AND SCHEDULING ............................................................. 7 ARTICLE H – PAID HOLIDAYS ................................................................................................31 ARTICLE I – VACATIONS