Khanewal District – Preventive Child Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Muzaffargarh
! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! !! ! ! ! ! ! Overview - Muzaffargarh ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! ! Bhattiwala Kherawala !Molewala Siwagwala ! Mari PuadhiMari Poadhi LelahLeiah ! ! Chanawala ! ! ! ! ! ! ! Ladhranwala Kherawala! ! ! ! Lerah Tindawala Ahmad Chirawala Bhukwala Jhang Tehsil ! ! ! ! ! ! ! Lalwala ! Pehar MorjhangiMarjhangi Anwarwal!a Khairewala ! ! ! ! ! ! ! ! ! Wali Dadwala MuhammadwalaJindawala Faqirewala ! ! ! ! ! ! ! ! ! MalkaniRetra !Shah Alamwala ! Bhindwalwala ! ! ! ! ! Patti Khar ! ! ! Dargaiwala Shah Alamwala ! ! ! ! ! ! Sultanwala ! ! Zubairwa(24e6)la Vasawa Khiarewala ! ! ! ! ! ! ! Jhok Bodo Mochiwala PakkaMochiwala KumharKumbar ! ! ! ! ! ! Qaziwala ! Haji MuhammadKhanwala Basti Dagi ! ! ! ! ! Lalwala Vasawa ! ! ! Mirani ! ! Munnawala! ! ! Mughlanwala ! Le! gend ! Sohnawala ! ! ! ! ! Pir Shahwala! ! ! Langanwala ! ! ! ! Chaubara ! Rajawala B!asti Saqi ! ! ! ! ! ! ! ! ! BuranawalaBuranawala !Gullanwala ! ! ! ! ! Jahaniawala ! ! ! ! ! Pathanwala Rajawala Maqaliwala Sanpalwala Massu Khanwala ! ! ! ! ! ! Bhandniwal!a Josawala ! ! Basti NasirBabhan Jaman Shah !Tarkhanwala ! !Mohanawala ! ! ! ! ! ! ! ! ! ! Basti Naseer Tarkhanwala Mohanawala !Citiy / Town ! Sohbawala ! Basti Bhedanwala ! ! ! ! ! ! Sohaganwala Bhurliwala ! ! ! ! Thattha BulaniBolani Ladhana Kunnal Thal Pharlawala ! ! ! ! ! ! ! ! ! ! ! Ganjiwala Pinglarwala Sanpal Siddiq Bajwa ! ! ! ! ! Anhiwala Balochanwala ! Pahrewali ! ! Ahmadwala ! ! ! -

Impacts of Biradarism on the Politics of Punjab: a Case Study of District Khanewal
Impacts of Biradarism on the Politics of Punjab: A Case Study of District Khanewal Shahnaz Tariq Muhammad Alamgir The aim of this study is to examine the impact of Biradarism on the politics of Punjab in general and on the politics of the Khanewal District in particular. The concept of Biradarism is defined and distinguished from the concept of caste system in the Hindu culture and society. Different aspects of Biradarism which determine the voting behaviour and pattern in the subject area are carefully viewed and analyzed. Historical, analytical and comparative methods are applied which can fairly provide a preliminary base for those who may be interested in further studies on this topic. Introduction It shall be useful if we briefly define some main concepts which form the basis of this study. Politics can be defined as an activity by which conflicting interests of various stake holders are conciliated and resolved with in a given society or political system by providing them a share and opportunity proportionate to their political significance and strength, thus achieving collective welfare and survival of the society1. Impacts of Biradarism on the Politics of Punjab: A Case Study ………….. 183 Biradari or Biradarism is derived from the Persian word Brother which means Brotherhood and can be defined as a common bandage or affiliations on the basis of religion, language, race, caste etc2. In the Subcontinent this term is used for identifying the different clans in terms of their castes for mutual interaction. It is interesting to note that during the British Raj in the Subcontinent all the legal and documentary transactions required declaration of caste by the person concerned thus the caste of a person served as a symbol of his or her identity and introduction. -

Population According to Religion, Tables-6, Pakistan
-No. 32A 11 I I ! I , 1 --.. ".._" I l <t I If _:ENSUS OF RAKISTAN, 1951 ( 1 - - I O .PUlA'TION ACC<!>R'DING TO RELIGIO ~ (TA~LE; 6)/ \ 1 \ \ ,I tin N~.2 1 • t ~ ~ I, . : - f I ~ (bFICE OF THE ~ENSU) ' COMMISSIO ~ ER; .1 :VERNMENT OF PAKISTAN, l .. October 1951 - ~........-.~ .1',l 1 RY OF THE INTERIOR, PI'ice Rs. 2 ~f 5. it '7 J . CH I. ~ CE.N TABLE 6.-RELIGION SECTION 6·1.-PAKISTAN Thousand personc:. ,Prorinces and States Total Muslim Caste Sch~duled Christian Others (Note 1) Hindu Caste Hindu ~ --- (l b c d e f g _-'--- --- ---- KISTAN 7,56,36 6,49,59 43,49 54,21 5,41 3,66 ;:histan and States 11,54 11,37 12 ] 4 listricts 6,02 5,94 3 1 4 States 5,52 5,43 9 ,: Bengal 4,19,32 3,22,27 41,87 50,52 1,07 3,59 aeral Capital Area, 11,23 10,78 5 13 21 6 Karachi. ·W. F. P. and Tribal 58,65 58,58 1 2 4 Areas. Districts 32,23 32,17 " 4 Agencies (Tribal Areas) 26,42 26,41 aIIjab and BahawaJpur 2,06,37 2,02,01 3 30 4,03 State. Districts 1,88,15 1,83,93 2 19 4,01 Bahawa1pur State 18,22 18,08 11 2 ';ind and Kbairpur State 49,25 44,58 1,41 3,23 2 1 Districts 46,06 41,49 1,34 3,20 2 Khairpur State 3,19 3,09 7 3 I.-Excluding 207 thousand persons claiming Nationalities other than Pakistani. -

S. No. Bank Name Office Type* Name Tehsil District Province Address
List of Selected Operational Branches Office S. No. Bank Name Name Tehsil District Province Address License No. Type* BRL-20115 dt: 19.02.2013 1 Soneri Bank Limited Branch Main Br. Lahore-0001 Lahore City Tehsil Lahore Punjab 87, Shahrah-E-Quaid-E-Azam, Lahore (Duplicate) Plot No: Sr-2/11/2/1, Office No: 105-108, Al-Rahim Tower, I.I. Chundrigar Road, BRL-20114 dt: 19.02.2013 2 Soneri Bank Limited Branch Main Br. Karachi-0002 Karachi South District Karachi Sindh Karachi (Duplicate) BRL-20116 dt: 19.02.2013 3 Soneri Bank Limited Branch Main Branch Peshawar Peshawar Tehsil Peshawar KPK Property No: Ca/457/3/2/87, Saddar Road, Peshawar Cantt., (Duplicate) BRL-20117 dt: 19.02.2013 4 Soneri Bank Limited Branch Main Br. Quetta-0004 Quetta City Tehsil Quetta Balochistan Ground Floor, Al-Shams Hotel, M.A. Jinnah Road, Quetta. (Duplicate) BRL-17606 dt: 03.03.2009 5 Soneri Bank Limited Branch Main Branch Mirpur Mirpur Mirpur AJK Plot No: 35/A, Munshi Sher Plaza, Allama Iqbal Road, New Mirpur Town, Mirpur (Ak) (Duplicate) Main Branch, Hyderabad.- 6 Soneri Bank Limited Branch Hyderabad City Taluka Hyderabad Sindh Shop No: 6, 7 & 8, Plot No: 475, Dr. Ziauddin Road, Hyderabad BRL-13188 dt: 04.04.1993 0006 7 Soneri Bank Limited Branch Main Guj-0007 Gujranwala City Tehsil Gujranwala Punjab Khewat & Khatooni: 78 Khasra No: 393 Near Din Plaza G. T. Road Gujranwala BRL-13192 dt: 14.07.1993 8 Soneri Bank Limited Branch Main Fsd-0008 Faisalabad City Tehsil Faisalabad Punjab Chiniot Bazar, Faisalabad BRL-13196 dt: 30.09.1993 9 Soneri Bank Limited Branch Sie Br. -

Crop Damage Assessment Along the Indus River
0 1 0 2 K t A 0 s -P . u 1 2 g 4 n 1 u 0 io A 0 rs 0 -0 e 2 0 V 1 0 -2 L F " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " "" " " " " " " " " " " " " " " " " " " " " " " " " !( " " " " " " " " " " " " " " " " " " " !(" " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " "" " " " " " " " " " " " " " " " " " " " " " " " p " " " " " " " p " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " "" " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " : " " " " " " " !( " " " " " " " " " " " y " " " " " " " " " " " " " " " " " " " " " " " " " b " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " " d " " " " " " " " " " " " " !( " " e " " " " " " " " " " t " "" " "p " " " " " " " " " " r " !( " " " " !( " " " " !( " " " p " " " " " " " o " " " " " " " " " " " " " " " " " " " " " " " " " p " " " " " " " " " " " " " " " " " " " " p " " " " " "" " " " " " " " " " " " " " " " " " " u " " " " " " " " " " t " " " !( " " " S " " " . " " " " " " " " " " o " " " " " " n " " " " " " " " " " " " " " D" " p " " " nn " " " " " " " " " !( " " " " e " " " " " " " " " " " " r O " " " " " " " " " " " " " " " " " " a M " " " " " " " " " " I " " " " " " " " " " " " " " " " " " " e " " " " " " " " " aa " " " !( !(r C " " " " " " " " I " " " " " " " " " " " " " " " e " " " " " " " " " e L " " " p" " " " " " " " h I " " " " " " " " " tt "" -

Spatio-Temporal Flood Analysis Along the Indus River, Sindh, Punjab
p !( !( 23 August 2010 !( FL-2010-000141-PAK S p a t i o - Te m p o r a l F!( lo o d A n a l y s i s a l o n g t h e I n d u s R i v e r, S i n d h , P u n j a b , K P K a n d B a l o c h i s t a n P r o v i n c e s , P a k i s t a n p Version 1.0 !( This map shows daily variation in flo!(od water extent along the Indus rivers in Sindph, Punjab, Balochistan and KPK Index map CHINA p Crisis Satellite data : MODIS Terra / Aqua Map Scale for 1:1,000,000 Map prepared by: Supported by: provinces based on time-series MODIS Terra and Aqua datasets from August 17 to August 21, 2010. Resolution : 250m Legend 0 25 50 100 AFGHANISTAN !( Image date : August 18-22, 2010 Result show that the flood extent isq® continously increasing during the last 5 days as observed in Shahdad Kot Tehsil p Source : NASA Pre-Flood River Line (2009) Kilometres of Sindh and Balochistan provinces covering villages of Shahdad, Jamali, Rahoja, Silra. In the Punjab provinces flood has q® Airport p Pre-flood Image : MODIS Terra / Aqua Map layout designed for A1 Printing (36 x 24 inch) !( partially increased further in Shujabad Tehsil villages of Bajuwala Ti!(bba, Faizpur, Isanwali, Mulana)as. Over 1000 villages !( ® Resolution : 250m Flood Water extent (Aug 18) p and 100 towns were identified as severly affepcted by flood waters and vanalysis was performed using geospatial database ® Heliport !( Image date : September 19, 2009 !( v !( Flood Water extent (Aug 19) ! received from University of Georgia, google earth and GIS data of NIMA (USGS). -
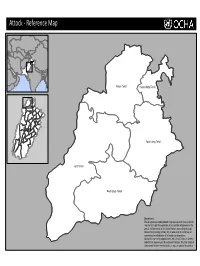
Reference Map
Attock ‐ Reference Map Attock Tehsil Hasan Abdal Tehsil Punjab Fateh Jang Tehsil Jand Tehsil Pindi Gheb Tehsil Disclaimers: The designations employed and the presentation of material on this map do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted line represents approximately the Line of Control in Jammu and Kashmir agreed upon by India and Pakistan. The final status of Jammu and Kashmir has not yet been agreed upon by the parties. Bahawalnagar‐ Reference Map Minchinabad Tehsil Bahawalnagar Tehsil Chishtian Tehsil Punjab Haroonabad Tehsil Fortabbas Tehsil Disclaimers: The designations employed and the presentation of material on this map do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted line represents approximately the Line of Control in Jammu and Kashmir agreed upon by India and Pakistan. The final status of Jammu and Kashmir has not yet been agreed upon by the parties. p Bahawalpur‐ Reference Map Hasilpur Tehsil Khairpur Tamewali Tehsil Bahawalpur Tehsil Ahmadpur East Tehsil Punjab Yazman Tehsil Disclaimers: The designations employed and the presentation of material on this map do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

Jhang: Annual Development Program and Its Implementation (2008-09)
April 2009 CPDI District Jhang: Annual Development Program and its Implementation (2008-09) Table of Contents 1. Background 2. Annual Development Program (2008-09) 3. Implementation of Annual Development Program (2008-09): Issues and Concerns 4. Recommendations Centre for Peace and Development Initiatives (CPDI) 1 District Jhang: Annual Development Program and its Implementation (2008-09) 1. Background Jhang district is located in the Punjab province. Total area of the district is 8,809 square kilometers. It is bounded on the north by Sargodha and Hafizabad districts, on the south by Khanewal district, on the west by Layyah, Bhakkar and Khushab districts, on the east by Faisalabad and Toba Tek Singh districts and on the south-west by Muzaffargarh district. According to the census conducted in 1998, the total population of the district was 2.8 million, as compared to about 2 million in 1981. It is largerly a rural district as only around 23% people live in the urban areas. According to a 2008 estimate, the population of the district has risen to about 3.5 million. Table 1: Population Profile of Jhang District 1951 1961 1972 1981 1998 Total 8,63,000 10,65,000 15,55,000 19,71,000 28,34,545 Rural - - - - 21,71,555 Urban - - - - 6,62,990 Urban population as %age of Total - - - - 23.4% Source: Population Census Organization, Statistics Division, Government of Pakistan , District Census Report of Jhang, Islamabad, August 2000. Jhang is one of the oldest districts of the Punjab province. Currently, the district consists of 4 tehsils: Ahmad Pur Sial, Chiniot, Jhang and Shorkot. -

1951-81 Population Administrative . Units
1951- 81 POPULATION OF ADMINISTRATIVE . UNITS (AS ON 4th FEBRUARY. 1986 ) - POPULATION CENSUS ORGANISATION ST ATIS TICS DIVISION GOVERNMENT OF PAKISTAN PREFACE The census data is presented in publica tions of each census according to the boundaries of districts, sub-divisions and tehsils/talukas at the t ime of the respective census. But when the data over a period of time is to be examined and analysed it requires to be adjusted fo r the present boundaries, in case of changes in these. It ha s been observed that over the period of last censuses there have been certain c hanges in the boundaries of so me administrative units. It was, therefore, considered advisable that the ce nsus data may be presented according to the boundary position of these areas of some recent date. The census data of all the four censuses of Pakistan have, therefore, been adjusted according to the administ rative units as on 4th February, 1986. The details of these changes have been given at Annexu re- A. Though it would have been preferable to tabulate the whole census data, i.e., population by age , sex, etc., accordingly, yet in view of the very huge work involved even for the 1981 Census and in the absence of availability of source data from the previous three ce nsuses, only population figures have been adjusted. 2. The population of some of the district s and tehsils could no t be worked out clue to non-availability of comparable data of mauzas/dehs/villages comprising these areas. Consequently, their population has been shown against t he district out of which new districts or rehsils were created. -

Punjab Health Statistics 2019-2020.Pdf
Calendar Year 2020 Punjab Health Statistics HOSPITALS, DISPENSARIES, RURAL HEALTH CENTERS, SUB-HEALTH CENTERS, BASIC HEALTH UNITS T.B CLINICS AND MATERNAL & CHILD HEALTH CENTERS AS ON 01.01.2020 BUREAU OF STATISTICS PLANNING AND DEVELOPMENT BOARD GOVERNMENT OF THE PUNJAB, LAHORE www.bos.gop.pk Content P a g e Sr. No. T i t l e No. 1 Preface I 2 List of Acronym II 3 Introduction III 4 Data Collection System IV 5 Definitions V 6 List of Tables VI 7 List of Figures VII Preface It is a matter of pleasure, that Bureau of Statistics, Planning & Development Board, Government of the Punjab has took initiate to publish "Punjab Health Statistics 2020". This is the first edition and a valuable increase in the list of Bureau's publication. This report would be helpful to the decision makers at District/Tehsil as well as provincial level of the concern sector. The publication has been formulated on the basis of information received from Director General Health Services, Chief Executive Officers (CEO’s), Inspector General (I.G) Prison, Auqaf Department, Punjab Employees Social Security, Pakistan Railways, Director General Medical Services WAPDA, Pakistan Nursing Council and Pakistan Medical and Dental Council. To meet the data requirements for health planning, evaluation and research this publication contain detailed information on Health Statistics at the Tehsil/District/Division level regarding: I. Number of Health Institutions and their beds’ strength II. In-door & Out-door patients treated in the Health Institutions III. Registered Medical & Para-Medical Personnel It is hoped that this publication would prove a useful reference for Government departments, private institutions, academia and researchers. -
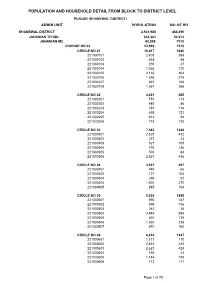
Population and Household Detail from Block to District Level
POPULATION AND HOUSEHOLD DETAIL FROM BLOCK TO DISTRICT LEVEL PUNJAB (KHANEWAL DISTRICT) ADMIN UNIT POPULATION NO OF HH KHANEWAL DISTRICT 2,921,986 466,390 JAHANIAN TEHSIL 343,361 52,613 JAHANIAN MC 43,598 7010 CHARGE NO 03 43,598 7010 CIRCLE NO 01 10,417 1640 221030101 2,403 388 221030102 614 84 221030103 250 47 221030104 1,065 170 221030105 2,135 304 221030106 1,596 275 221030107 697 106 221030108 1,657 266 CIRCLE NO 02 4,001 655 221030201 751 113 221030202 480 86 221030203 781 116 221030204 658 121 221030205 613 94 221030206 718 125 CIRCLE NO 03 7,583 1226 221030301 2,625 432 221030302 237 43 221030303 521 105 221030304 776 126 221030305 503 84 221030306 2,921 436 CIRCLE NO 04 3,947 657 221030401 440 66 221030402 727 104 221030403 295 52 221030404 1,600 272 221030405 885 163 CIRCLE NO 05 9,034 1485 221030501 990 187 221030502 898 156 221030503 262 38 221030504 3,844 583 221030505 810 135 221030506 1,360 226 221030507 870 160 CIRCLE NO 06 8,616 1347 221030601 1,111 170 221030602 2,812 425 221030603 2,621 424 221030604 156 23 221030605 1,144 188 221030606 772 117 Page 1 of 74 POPULATION AND HOUSEHOLD DETAIL FROM BLOCK TO DISTRICT LEVEL PUNJAB (KHANEWAL DISTRICT) ADMIN UNIT POPULATION NO OF HH JAHANIAN QH 169,785 25814 055/10-R PC 5,480 875 CHAK NO 053/10-R 1,932 337 221011403 1,124 197 221011404 700 124 221011405 108 16 CHAK NO 054/10-R 2,037 318 221011402 1,133 188 221011406 904 130 CHAK NO 055/10-R 1,511 220 221011401 1,511 220 056/10-R PC 6,093 890 CHAK NO 056/10-R 2,028 307 221011501 1,059 157 221011502 969 150 CHAK NO 057/10-R 2,786 -

Microbiological and Physicochemical Assessments of Groundwater Quality at Punjab, Pakistan
Vol. 8(28), pp. 2672-2681, 9 July, 2014 DOI: 10.5897/AJMR2014.6701 Article Number: 852257345925 ISSN 1996-0808 African Journal of Microbiology Research Copyright © 2014 Author(s) retain the copyright of this article http://www.academicjournals.org/AJMR Full Length Research Paper Microbiological and physicochemical assessments of groundwater quality at Punjab, Pakistan Ammara Hassan1* and M. Nawaz2 1Pakistan Council of Scientific and Industrial Research, Lahore, Pakistan. 2College of Earth and Environmental Sciences, University of the Punjab, Lahore, Pakistan. Received 10 February, 2014; Accepted 23 June, 2014 The assessment of groundwater is essential for the estimation of suitability of water for safe use. An attempt has been made to study the groundwater at the district level of Punjab, Pakistan. These samples were analyzed for various water quality parameters like pH, color, odor, conductance, total suspended solids, trace metals (Fe, cu, B, Ba, Al, Cr, Cd, Ni, Mn and Se), ionic concentration (HCO3, CO3, Cl, SO4, Na, K, Ca, Mg, NO3, NO2, NH4, F, PO4 and CN) and for microbiological enumeration (total viable count, total and fecal coliforms Escherichia coli, Salmonella spp. and Pseudomonas spp.). The data was analyzed with WHO guidelines/ recommendations. The results of physical analysis indicated that all samples are safe except the groundwater of Kasur and Khanewal District. About 66.67% samples are out of total suspended solids (TSS) limit. Microbiologically, only six groundwater of Punjab districts are found potable according to WHO limits. In the trace metals analysis, highest level of iron was detected in Jhang while the groundwater of three districts were not potable due to high level of boron and nickel but the groundwater of all districts was found safe with respect to Ba, Al and Cr.