Annual Report 2018 –2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Property Interest Report 4 Smith St, Midland 6056
Property Interest Report 4 Smith St, Midland 6056 landgate.wa.gov.au Contents 2 Property information Summary of interests that AFFECT This section includes an aerial this property 1. photograph and details of this 2. This section helps you to see at a glance property. interests pertaining to this property. Summary of interests that Details of interests that AFFECT this DO NOT AFFECT this property property 3. This section helps you to see at a 4. This section provides details of how an glance interests that do not affect interest specifically relates to this property. this property. What is a property interest? It is recommended that a copy of the Certificate of Title A property interest gives rights to a land owner but is obtained to identify any registered interests and/or also, could imply restrictions or impose information. Visit landgate.wa.gov.au to order a copy of responsibilities which may impact on their use or the Certificate of Title. enjoyment of the land. Most interests are created by government legislation, policies and guidelines. How do I find out more information? For further information about interests including Where does property interest information come from? information, contact details and relevant legislation on This service gathers interest information from multiple any interests in this report, see government bodies and private organisations in www0.landgate.wa.gov.au/interestdictionary. Western Australia and consolidates that information into the Property Interest Report. This report will If you have any queries or concerns, please contact the show interests that do and do not affect the responsible agency of the interest property. -

Western Australian State Government Agencies
FACT SHEET Jobs and Skills WA Employer Incentive eligibility: Western Australian State Government Agencies Out of scope of the incentive The following list of approved Western Australian State Government Agencies are ineligible for the Jobs and Skills WA Employer Incentive. Western Australian State Government agencies Agency name Government SES Non-SES department organisations organisations Agricultural Produce Commission √ Animal Resources Authority √ Architects Board of Western Australia √ Botanical Gardens and Parks √ Authority Building and Construction Industry √ Training Board Burswood Park Board √ Central Regional TAFE √ Chemistry Centre (WA) √ Child and Adolescent Health Service √ Combat Sports Commission √ Commission for Occupational Safety √ and Health (Worksafe) Commissioner for Children and √ Young People Commissioner for Equal Opportunity √ Commissioner of Main Roads √ Conservation Commission of Western √ Australia Construction Industry Long Service √ Leave Payments Board Corruption and Crime Commission √ Country Housing Authority √ Department of Biodiversity, √ Conservation and Attractions Department of Communities √ Department of Education √ Department of Finance √ 7 November 2019 | Page 1 Western Australian State Government agencies Agency name Government SES Non-SES department organisations organisations Department of Fire and Emergency √ Services Department of Health √ Department of Jobs, Tourism, √ Science and Innovation Department of Justice √ Department of Local Government, √ Sport and Cultural Industries Department -

ANNUAL REPORT REPORT 2020 20203 COMMISSIONER’S FOREWORD Thank You for Your Interest in the Western Australia Police Force Annual Report of 2020
CONTENTS COMMISSIONER’S FOREWORD .................................................................................... 4 AWARDS AND RECOGNITION ................................................................................................................................... 43 EXECUTIVE SUMMARY .................................................................................................... 6 ROAD SAFETY COMMISSION ......................................................................................................................................44 OVERVIEW OF THE AGENCY ......................................................................................... 8 SUMMARY OF RESULTS AGAINST FINANCIAL TARGETS .........................................................51 AGENCY AT A GLANCE .............................................................................................................................................................8 SUMMARY OF RESULTS AGAINST PERFORMANCE TARGETS ........................................ 52 OPERATIONAL STRUCTURE ..............................................................................................................................................9 SUMMARY OF VARIATION AGAINST PERFORMANCE TARGETS ................................. 53 REGIONS AND DISTRICTS ................................................................................................................................................ 10 SIGNIFICANT ISSUES IMPACTING THE AGENCY ....................................................54 -

Landgate a N N U a L R E P O R T 2 0 0 7 Landgate Postal Address Midland Square PO Box 2222 MIDLAND WA 6056 MIDLAND WA 6936
40 75 75 60 75 85 40 105 95 95 60 95 110 70 80 130 130 60 110 90 landgate ANNU A L R E P O R T 2 0 0 7 LANDGATE POSTAL ADDRESS Midland Square PO Box 2222 MIDLAND WA 6056 MIDLAND WA 6936 Telephone: (08) 9273 7373 Landgate website: www.landgate.wa.gov.au Facsimile: (08) 9273 7666 WALIS website: www.walis.wa.gov.au [email protected] WALIS email: [email protected] TTY (telephone for people with hearing impairment): (08) 9273 7571 VALUATION SERVICES BUNBURY REGIONAL OFFICE AND 18 Mount Street VALUATION SERVICES PERTH WA 6000 61 Victoria Street Postal Address: BUNBURY 6230 PO Box 7201 Telephone: (08) 9791 0836 Cloisters Square Facsimile: (08) 9791 0835 PERTH 6850 Valuation Services Telephone: (08) 9429 8400 Telephone: (08) 9721 0800 Facsimile: (08) 9429 8500 Facsimile: (08) 9721 4465 [email protected] [email protected] PERTH BRANCH OFFICE Mount Newman House VALUATION SERVICES ALBANY Cloisters Square DISTRICT OFFICE 220 St Georges Terrace (Limited service to the public available) PERTH 6000 58 Serpentine Road ALBANY 6330 SATELLITE REMOTE SENSING Telephone: (08) 9841 4532 SERVICES Facsimile: (08) 9841 2311 Leeuwin Centre for Earth Sensing [email protected] Technologies 65 Brockway Road FLOREAT 6014 Telephone: (08) 9387 0330 Facsimile: (08) 9383 7142 [email protected] PUBLICATIONS Landgate produces a vast range of published material Including the StreetSmart Street Directory, WA Travellers Atlas, Touring Map Series, Landmarks magazine, aerial photography and satellite imagery. Many of the Agency’s publications are available online. -

Landgate Received on 31 Jul 2019
Office of the Chief Executive Your Ref: A761673 Our Ref:3977-2019 Enquiries: Graeme Gammie Tel: 9273 7003 Email: [email protected] The Committee Clerk Standing Committee on Public Administration Legislative Council Parliament House Attention: Ms Kristina Crichton PERTH WA 6000 BY EMAIL: [email protected] Dear Ms Crichton, INQUIRY INTO PRIVATE PROPERTY RIGHTS – SUBMISSION Thank you for your letter dated 5 July 2019 inviting submissions on the following Terms of Reference referred by the Legislative Council to the Standing Committee on Public Administration (the Committee) for Inquiry: “That the House — (a) recognises the fundamental proprietary right of private property ownership that underpins the social and economic security of the community; (b) recognises the threat to the probity of the Torrens Title system, that guarantees disclosure, and re-establish the necessity for registration of all encumbrances that affect land including Environmentally Sensitive Areas (ESAs), bushfire prone areas and implied easements for Western Power which currently sit behind the certificate of title; (c) recognises the property rights of government issued licenses and authorities including commercial fishing; (d) asserts that fair and reasonable compensation must be paid to the owner of private property if the value of the property is diminished by a government encumbrance or resumption in order to derive a public benefit; and (e) directs the Public Administration Committee to conduct an enquiry into the matters described above -
“Reframing Rural Fire Management” I Nqui R Y
R EPO R T OF THE S PECIAL “Reframing Rural Fire Management” I NQUI R Y INTO THE J REPORT OF THE SPECIAL INQUIRY ANUA R INTO THE Y 2016 W 2016 JANUARY 2016 WAROONA FIRE A R OONA F I R E : A PPENDICE S VOLUME 2: APPENDICES Waroona Fires 2016 Cover.indd 2 5/3/2016 2:47:40 PM Schedule A PUBLIC INQUIRY INTO JANUARY 2016 WAROONA FIRE TERMS OF REFERENCE Preamble The January 2016 Waroona Fire has caused significant damage, particularly to the town of Yarloop, and the tragic loss of life. The Government of Western Australia is committed to managing bushfire-related risk and continuously improving the State’s capabilities to prevent, mitigate and respond to major bushfires to protect the Western Australian community and the assets it values. For this purpose, the Government has committed to the establishment of an open and independent review of the management of the fire, with broad terms of reference that will allow for consideration of what has been learned from previous major bushfires, what can be learned from the Waroona Fire, and strategies for future reforms and capability enhancements to efficiently and effectively manage bushfire-related risk. Terms of Reference The terms of reference for the Inquiry are to examine and report on: 1. The response to the January 2016 Waroona Fire (a) The effectiveness of pre-incident bushfire prevention and mitigation activities; (b) The effectiveness of emergency management plans and procedures; (c) The effectiveness of the suppression strategies and tactics used during the fire; (d) The effectiveness of -

Inquest Finding
Coroners Act 1996 [Section 26(1)] Coroner’s Court of Western Australia RECORD OF INVESTIGATION INTO DEATH Ref: 13/19 I, Sarah Helen Linton, Coroner, having investigated the deaths of Kym Brett CURNOW, Thomas Leslie BUTCHER, Julia KOHRS-LICHTE and Anna Sushchova WINTHER, with an inquest held at the Esperance Courthouse on 25 to 29 March 2019, find that the identities of the deceased persons were Kym Brett CURNOW, Thomas Leslie BUTCHER, Julia KOHRS-LICHTE and Anna Sushchova WINTHER and that the deaths occurred on 17 November 2015 at Grigg Road, Scaddan, in the following circumstances: Counsel Appearing: Sgt L Housiaux assisting the Coroner. Ms R Hartley (State Solicitor’s Office) appearing on behalf of the Department of Biodiversity, Conservation and Attractions (and specifically the Parks and Wildlife Service) and the Department of Fire and Emergency Services as well as the witnesses Gregory Mair, Robert Blok, Andrew Duckworth, Gavin Wornes, Trevor Tasker and Gary Gifford. Mr M Trowell QC and Ms Crosby (DLA Piper) appearing on behalf of the Shire of Esperance. Mr T Nolan appearing on behalf of the United Professional Firefighters Union of Western Australia. Inquest into the deaths of Kym CURNOW, Thomas BUTCHER, Julia KOHRS-LICHTE 1 and Anna WINTHER (8059/15, 8060/15, 8062/15, 8063/15) TABLE OF CONTENTS INTRODUCTION ...................................................................................................... 3 THE DECEASED ..................................................................................................... 5 Thomas -

WA Marine Oil Pollution Risk Assessment: Protection Priorities
DOT307215 Provision of Western Australian Marine Oil Pollution Risk Assessment - Protection Priorities Protection Priority Assessment for Zone 1: Kimberley - Draft Report 18 May 2018 QV1 Building 250 St Georges Terrace Perth WA 6000 Australia 301320-09591-EN-REP-0003 www.advisian.com DOT307215 Provision of Western Australian Marine Oil Pollution Risk Assessment - Protection Priorities Protection Priority Assessment for Zone 1: Kimberley - Draft Report Disclaimer This report has been prepared on behalf of and for the exclusive use of Department of Transport, and is subject to and issued in accordance with the agreement between Department of Transport and Advisian. Advisian accepts no liability or responsibility whatsoever for it in respect of any use of or reliance upon this report by any third party. Copying this report without the permission of Department of Transport and Advisian is not permitted. Report No: 301320-09591-EN-REP-0003 – DOT307215 Provision of Western Australian Marine Oil Pollution Risk Assessment - Protection Priorities: Protection Priority Assessment for Zone 1: Kimberley - Draft Report Rev Description Author Review Approved Date A Issued for Internal Review 10-Apr-2018 R Morgan L Laver B Issued for Client Review 16-Apr-2018 R Morgan L Laver R Morgan 0 Final to client 18-May-2018 R Morgan L Laver R Morgan Advisian ii DOT307215 Provision of Western Australian Marine Oil Pollution Risk Assessment - Protection Priorities Protection Priority Assessment for Zone 1: Kimberley - Draft Report Executive Summary The Western Australian Department of Transport (DoT) is the Hazard Management Agency (HMA) for marine oil pollution in Western Australia (WA). As the HMA, DoT ensures the capacity of the State to respond to an oil spill is commensurate with the risk. -
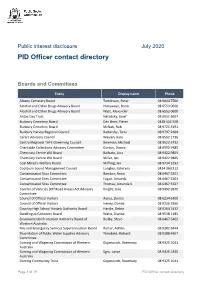
PID Officer Contact Directory
Public interest disclosure July 2020 PID Officer contact directory Boards and Committees Entity Display name Phone Albany Cemetery Board Tomlinson, Peter 08 9844 7766 Alcohol and Other Drugs Advisory Board Hlatywayo, Brian 08 6553 0600 Alcohol and Other Drugs Advisory Board Watt, Alexander 08 6553 0600 Anzac Day Trust Netolicky, Josef 08 6551 2607 Bunbury Cemetery Board Den Boer, Pieter 0438 424 558 Bunbury Cemetery Board McNab, Rob 08 9721 3191 Bunbury Harvey Regional Council Battersby, Tony 08 9797 2404 Carers Advisory Council Waylen, Kate 08 6552 1736 Central Regional TAFE Governing Council Bowman, Michael 08 9622 6792 Charitable Collections Advisory Committee Gorton, Donna 08 6552 9385 Chemistry Centre WA Board Barbato, Lina 08 9422 9803 Chemistry Centre WA Board Miller, Ian 08 9422 9805 Coal Miner's Welfare Board Miffling, Ian 08 9734 3293 Cockburn Sound Management Council Longley, Kateryna 0414 360 212 Contaminated Sites Committee Bamber, Anna 08 6467 5201 Contaminated Sites Committee Fagan, Amanda 08 6467 5201 Contaminated Sites Committee Thomas, Amanda K 08 6467 5327 Control of Vehicles (Off Road Areas) Act Advisory Knight, Julie 08 9492 9870 Committee Council of Official Visitors Ayriss, Donna 08 6234 6300 Council of Official Visitors Haney, Donna 08 9226 3266 Country High School Hostels Authority Board Hardie, Debra 08 9264 5432 Dwellingup Cemetery Board Watts, Dianne 08 9538 1185 Environmental Protection Authority Board of Beilby, Steve 08 6467 5402 Western Australia Fire and Emergency Services Superannuation Board Rutter, -

Description of Land Type Categories TENGRAPH Preamble
Description of Land Type Categories TENGRAPH Preamble This manual has been created to assist in the understanding of the different land types displayed in TENGRAPH. It contains descriptions for each of the types of land categories that may affect access for mineral exploration and mining in Western Australia. Terms Code The code is an abbreviation of the land type and is followed by an identifying number for administration purposes. It should be noted that not all Land Types are assigned a code abbreviation. Land Type The name of the land type being described. Category For departmental and customer assistance, the land types have been placed into one of the following four categories; • Administrative - Land Types that are defined for legislative jurisdictions and regulatory purposes. • Crown and Other Reserves - Land set aside on behalf of the community - generally for public purposes. • Special Category - Land Types of a special nature which are identified to help ensure the appropriate processing of tenements under the Mining Act. • Proposal - Proposed change to either create a new, or modify existing land tenure. Management Authority The Agency responsible for the management of the land type. Description A short account and general information about the land type. Land Type Index Land Type Pg Land Type Pg Land Type Pg 2015 Pastoral Lease Exclusion Areas 1 CTR – Timber Reserve (Calm Act ) 8 MZ – Mineralisation Zone 17 Perth Urban Area 1 DA – Designated Area (Diamond Agreement Act) 9 NHL – National Heritage List 17 Territorial Sea Baseline -

“Reframing Rural Fire Management” I Nqui R Y
R EPO R T OF THE S PECIAL “Reframing Rural Fire Management” I NQUI R Y INTO THE REPORT OF THE SPECIAL INQUIRY J ANUA INTO THE R Y 2016 W 2016 JANUARY 2016 WAROONA FIRE A R OONA F I R E : R EPO R T VOLUME 1: REPORT Waroona Fires 2016 Cover.indd 1 5/3/2016 12:39:26 PM Government Of Western Australia “REFRAMING RURAL FIRE MANAGEMENT” REPORT OF THE SPECIAL INQUIRY INTO THE JANUARY 2016 WAROONA FIRE Waroona Fire Special Inquiry 29 April 2016 Mr M C Wauchope Commissioner Public Sector Commission Locked Bag 3002 WEST PERTH WA 6827 Dear Mr Wauchope, SPECIAL INQUIRY INTO JANUARY 2016 WAROONA FIRE I am pleased to submit the Report of the Special Inquiry into the January 2016 Waroona Fire. The Special Inquiry has been conducted in accordance with the provisions of the Public Sector Management Act 1994 and the Terms of Reference. The Special Inquiry started in early February, ran for 13 weeks and held formal hearings on 22 days. The Special Inquiry has evoked a significant response. One hundred and sixty five written submissions have been received. One hundred people appeared at formal hearings and five people gave evidence via telephone. We have met and interacted with 42 organisations and interest groups. My gratitude goes to all those who contributed their wisdom, knowledge and experience to this Special Inquiry. The Special Inquiry team has worked diligently to inquire against the Terms of Reference and to analyse the matters presented in submissions and in formal hearings. The Special Inquiry has endeavoured to meet with and listen to all who registered an interest. -

Chart of the Western Australian Government Produced on 20 December 2019 [email protected]
Chart of the Western Australian Government Produced on 20 December 2019 www.publicsector.wa.gov.au [email protected] Premier; Minister for Public Sector Management; Minister for Education and Training Minister for Tourism; Racing and Gaming; Small Business; State Development, Jobs and Trade; Federal-State Department of Education 1 Defence Issues; Citizenship and Multicultural Interests Relations Department of Training and Workforce Development 1 Department of the Premier and Cabinet 1 Department of Local Government, Sport and Cultural Industries 1 School Curriculum and Standards Authority 8 1 Department of Jobs, Tourism, Science and Innovation 1 Department of Jobs, Tourism, Science and Innovation 1 Public Sector Commission 1 Colleges est. under Vocational Education and Training Act 1996 (5) 1 Western Australian Tourism Commission 8 1 Lotteries Commission (Lotterywest) 1 Trustees of Public Education Endowment 1 Infrastructure WA 1 Building and Construction Industry Training Board 3 Rottnest Island Authority 8 1,2 Office of Director of Equal Opportunity in Public Employment Universities (5) 1 Small Business Development Corporation 1 Parliamentary Commissioner for 1,3 Administrative Investigations (State Ombudsman) Minister for Emergency Services; Corrective Services Burswood Park Board 1 Salaries and Allowances Tribunal 3 Department of Fire and Emergency Services 1 Liquor Commission Gold Corporation 1 Department of Justice 1 Racing Penalties Appeal Tribunal 1 Governor’s Establishment Office of the Inspector of Custodial Services