Provisional Peer-Reviewed Toxicity Values For
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Inventory Size (Ml Or G) 103220 Dimethyl Sulfate 77-78-1 500 Ml
Inventory Bottle Size Number Name CAS# (mL or g) Room # Location 103220 Dimethyl sulfate 77-78-1 500 ml 3222 A-1 Benzonitrile 100-47-0 100ml 3222 A-1 Tin(IV)chloride 1.0 M in DCM 7676-78-8 100ml 3222 A-1 103713 Acetic Anhydride 108-24-7 500ml 3222 A2 103714 Sulfuric acid, fuming 9014-95-7 500g 3222 A2 103723 Phosphorus tribromide 7789-60-8 100g 3222 A2 103724 Trifluoroacetic acid 76-05-1 100g 3222 A2 101342 Succinyl chloride 543-20-4 3222 A2 100069 Chloroacetyl chloride 79-04-9 100ml 3222 A2 10002 Chloroacetyl chloride 79-04-9 100ml 3222 A2 101134 Acetyl chloride 75-36-5 500g 3222 A2 103721 Ethyl chlorooxoacetate 4755-77-5 100g 3222 A2 100423 Titanium(IV) chloride solution 7550-45-0 100ml 3222 A2 103877 Acetic Anhydride 108-24-7 1L 3222 A3 103874 Polyphosphoric acid 8017-16-1 1kg 3222 A3 103695 Chlorosulfonic acid 7790-94-5 100g 3222 A3 103694 Chlorosulfonic acid 7790-94-5 100g 3222 A3 103880 Methanesulfonic acid 75-75-2 500ml 3222 A3 103883 Oxalyl chloride 79-37-8 100ml 3222 A3 103889 Thiodiglycolic acid 123-93-3 500g 3222 A3 103888 Tetrafluoroboric acid 50% 16872-11-0 1L 3222 A3 103886 Tetrafluoroboric acid 50% 16872-11-0 1L 3222 A3 102969 sulfuric acid 7664-93-9 500 mL 2428 A7 102970 hydrochloric acid (37%) 7647-01-0 500 mL 2428 A7 102971 hydrochloric acid (37%) 7647-01-0 500 mL 2428 A7 102973 formic acid (88%) 64-18-6 500 mL 2428 A7 102974 hydrofloric acid (49%) 7664-39-3 500 mL 2428 A7 103320 Ammonium Hydroxide conc. -

Synthesis of New Thiazole and Thiazolyl Derivatives of Medicinal Significant-A Short Review
MOJ Bioorganic & Organic Chemistry Mini Review Open Access Synthesis of new thiazole and thiazolyl derivatives of medicinal significant-a short review Abstract Volume 2 Issue 2 - 2018 In the field of therapeutic science, thiazoles are of extraordinary importance, because of their potent and significant biological activities. Likewise thiazole and their Weiam Hussein,1 Gülhan Turan- derivatives are found in various powerful naturally and biologically active compounds Zitouni2 which possess a broad spectrum of biological activity therefore, synthesis of this 1Department of Pharmaceutical Chemistry, Aden University, compound is of remarkable concern. This review primarily focuses on the updated Yemen research papers reported in literature for the synthesis of thiazole and thiazolyl 2Department of Pharmaceutical Chemistry, Anadolu University, compounds. Turkey Keywords: thiazoles, thiazolyl, synthetic procedures, biological activity Correspondence: Weiam Hussein, Anadolu University, Faculty of Pharmacy, Department of Pharmaceutical Chemistry, Eskişehir, Turkey, Tel +905074929053, Email [email protected] Received: February 23, 2018| Published: March 12, 2018 Introduction Kaplancikli et al. 11 reported a simple and three steps-reaction procedure for the synthesis of new benzimidazole-thiazole derivatives. The synthesis of heterocyclic rings has been a fascinating field 4-(1H-benzimidazol-1-yl)benzaldehyde was prepared by reacting in therapeutic science. Various heterocyclic compounds containing 1H-benzimidazole and 4-fluorobenzaldehyde under microwave nitrogen and sulfur have flexible frameworks for drugs development irradiation, then, the reaction between 4-(1H-benzimidazol- and design.1 Thiazole is one of the most intensively studied classes of 1-yl)benzaldehyde and hydrazine carbothioamide gave as a aromatic five-membered heterocyclics. It was first defined by Hantzschresult 2-(4-(1H-benzimidazol-1-yl)benzylidene)hydrazine-1- and Weber in 1887. -
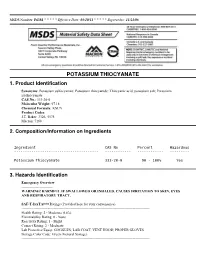
Potassium Thiocyanate 1
MSDS Number: P6181 * * * * * Effective Date: 03/10/11 * * * * * Supersedes: 11/21/08 POTASSIUM THIOCYANATE 1. Product Identification Synonyms: Potassium sulfocyanate; Potassium thiocyanide; Thiocyanic acid, potassium salt; Potassium isothiocyanate CAS No.: 333-20-0 Molecular Weight: 97.18 Chemical Formula: KSCN Product Codes: J.T. Baker: 3326, 5578 Macron: 7168 2. Composition/Information on Ingredients Ingredient CAS No Percent Hazardous --------------------------------------- ------------ ------------ --------- Potassium Thiocyanate 333-20-0 90 - 100% Yes 3. Hazards Identification Emergency Overview -------------------------- WARNING! HARMFUL IF SWALLOWED OR INHALED. CAUSES IRRITATION TO SKIN, EYES AND RESPIRATORY TRACT. SAF-T-DATA(tm) Ratings (Provided here for your convenience) ----------------------------------------------------------------------------------------------------------- Health Rating: 2 - Moderate (Life) Flammability Rating: 0 - None Reactivity Rating: 1 - Slight Contact Rating: 2 - Moderate Lab Protective Equip: GOGGLES; LAB COAT; VENT HOOD; PROPER GLOVES Storage Color Code: Green (General Storage) ----------------------------------------------------------------------------------------------------------- Potential Health Effects ---------------------------------- Inhalation: Causes irritation to the respiratory tract. Symptoms may include coughing, shortness of breath. Ingestion: May cause psychosis, vomiting, disorientation, weakness, low blood pressure, convulsions and death which may be delayed. The probable lethal -

1 Abietic Acid R Abrasive Silica for Polishing DR Acenaphthene M (LC
1 abietic acid R abrasive silica for polishing DR acenaphthene M (LC) acenaphthene quinone R acenaphthylene R acetal (see 1,1-diethoxyethane) acetaldehyde M (FC) acetaldehyde-d (CH3CDO) R acetaldehyde dimethyl acetal CH acetaldoxime R acetamide M (LC) acetamidinium chloride R acetamidoacrylic acid 2- NB acetamidobenzaldehyde p- R acetamidobenzenesulfonyl chloride 4- R acetamidodeoxythioglucopyranose triacetate 2- -2- -1- -β-D- 3,4,6- AB acetamidomethylthiazole 2- -4- PB acetanilide M (LC) acetazolamide R acetdimethylamide see dimethylacetamide, N,N- acethydrazide R acetic acid M (solv) acetic anhydride M (FC) acetmethylamide see methylacetamide, N- acetoacetamide R acetoacetanilide R acetoacetic acid, lithium salt R acetobromoglucose -α-D- NB acetohydroxamic acid R acetoin R acetol (hydroxyacetone) R acetonaphthalide (α)R acetone M (solv) acetone ,A.R. M (solv) acetone-d6 RM acetone cyanohydrin R acetonedicarboxylic acid ,dimethyl ester R acetonedicarboxylic acid -1,3- R acetone dimethyl acetal see dimethoxypropane 2,2- acetonitrile M (solv) acetonitrile-d3 RM acetonylacetone see hexanedione 2,5- acetonylbenzylhydroxycoumarin (3-(α- -4- R acetophenone M (LC) acetophenone oxime R acetophenone trimethylsilyl enol ether see phenyltrimethylsilyl... acetoxyacetone (oxopropyl acetate 2-) R acetoxybenzoic acid 4- DS acetoxynaphthoic acid 6- -2- R 2 acetylacetaldehyde dimethylacetal R acetylacetone (pentanedione -2,4-) M (C) acetylbenzonitrile p- R acetylbiphenyl 4- see phenylacetophenone, p- acetyl bromide M (FC) acetylbromothiophene 2- -5- -

United States Patent Office Patented Jan
3,071,593 United States Patent Office Patented Jan. 1, 1963 2 3,071,593 O PREPARATION OF AELKENE SULFES Paul F. Warner, Philips, Tex., assignor to Philips Petroleum Company, a corporation of Delaware wherein each R is selected from the group consisting of No Drawing. Filed July 27, 1959, Ser. No. 829,518 5 hydrogen, alkyl, aryl, alkaryl, aralkyl and cycloalkyl 8 Claims. (C. 260-327) groups having 1 to 8 carbon atoms, the combined R groups having up to 12 carbon atoms. Examples of Suit This invention relates to a method of preparing alkene able compounds are ethylene oxide, propylene oxide, iso sulfides. Another aspect relates to a method of convert butylene oxide, a-amylene oxide, styrene oxide, isopropyl ing an alkene oxide to the corresponding sulfide at rela O ethylene oxide, methylethylethylene oxide, 3-phenyl-1, tively high yields without refrigeration. 2-propylene oxide, (3-methylphenyl) ethylene oxide, By the term "alkene sulfide' as used in this specifica cyclohexylethylene oxide, 1-phenyl-3,4-epoxyhexane, and tion and in the claims, I mean to include not only un the like. substituted alkene sulfides such as ethylene sulfide, propyl The salts of thiocyanic acid which I prefer to use are ene sulfide, isobutylene sulfide, and the like, but also 5 the salts of the alkali metals or ammonium. I especially hydrocarbon-substituted alkene sulfides such as styrene prefer ammonium thiocyanate, sodium thiocyanate, and oxide, and in general all compounds conforming to the potassium thiocyanate. These compounds can be reacted formula with ethylene oxide in a cycloparaffin diluent to produce 20 substantial yields of ethylene sulfide and with little or S no polymer formation. -

Step-By-Step Guide to Better Laboratory Management Practices
Step-by-Step Guide to Better Laboratory Management Practices Prepared by The Washington State Department of Ecology Hazardous Waste and Toxics Reduction Program Publication No. 97- 431 Revised January 2003 Printed on recycled paper For additional copies of this document, contact: Department of Ecology Publications Distribution Center PO Box 47600 Olympia, WA 98504-7600 (360) 407-7472 or 1 (800) 633-7585 or contact your regional office: Department of Ecology’s Regional Offices (425) 649-7000 (509) 575-2490 (509) 329-3400 (360) 407-6300 The Department of Ecology is an equal opportunity agency and does not discriminate on the basis of race, creed, color, disability, age, religion, national origin, sex, marital status, disabled veteran’s status, Vietnam Era veteran’s status or sexual orientation. If you have special accommodation needs, or require this document in an alternate format, contact the Hazardous Waste and Toxics Reduction Program at (360)407-6700 (voice) or 711 or (800) 833-6388 (TTY). Table of Contents Introduction ....................................................................................................................................iii Section 1 Laboratory Hazardous Waste Management ...........................................................1 Designating Dangerous Waste................................................................................................1 Counting Wastes .......................................................................................................................8 Treatment by Generator...........................................................................................................12 -

Potassium Thiocyanate: a Rare Case Report
Case Report J Forensic Sci & Criminal Inves Volume 13 Issue 2 - November 2019 Copyright © All rights are reserved by R Rajiv DOI: 10.19080/JFSCI.2019.13.555857 A Homicidal Attempt - Potassium Thiocyanate: A Rare Case Report R Rajiv1*, GThirunavukkarasu2 and D Shanmugam3 1Scientific Officer, Regional Forensic Science Laboratory, India 2Deputy Director, Forensic Sciences Département, India 3Deputy Director, Regional Forensic Science Laboratory, India Submission: November 19, 2019, Published: November 26, 2019 *Corresponding author: R Rajiv, Scientific Officer, Regional Forensic Science Laboratory, Villupuram, India Abstract Forensic Toxicologist does tremendous work to find out various poisonous substances from Viscera to other materials pertaining to the crime cases. Potassium Thiocyanate (CAS number 333-20-0) is the chemical compound with the molecular formula KSCN. It is a colourless deliquescent crystals. In this case, one borrower offered a packed Gulab Jamun (Sweet) box to the money lender while returning the borrowed money. While the lender was tasting the sweet, he found some different taste, so he spat and subsequently he rushed to hospital. A criminal case has been registered in this regard, and the case article (Gulab jamun) was forwarded to our Forensic Science Laboratory by the investigating agency.Keywords: After the scrupulous analysis, Potassium Thiocyanate was detected in the content of the said item. Forensic science; Toxicological analysis; Potassium thiocyanate; Gulab jamun Introduction home to return some money and offered a sweet box full of The role of Forensic Toxicologist is to find out various Gulab jamun after a long chat. The lender happily accepted the poisonous substances from viscera and other materials offer as the borrower appealed to him to take some pieces as pertaining to the crime cases. -

House Fly Attractants and Arrestante: Screening of Chemicals Possessing Cyanide, Thiocyanate, Or Isothiocyanate Radicals
House Fly Attractants and Arrestante: Screening of Chemicals Possessing Cyanide, Thiocyanate, or Isothiocyanate Radicals Agriculture Handbook No. 403 Agricultural Research Service UNITED STATES DEPARTMENT OF AGRICULTURE Contents Page Methods 1 Results and discussion 3 Thiocyanic acid esters 8 Straight-chain nitriles 10 Propionitrile derivatives 10 Conclusions 24 Summary 25 Literature cited 26 This publication reports research involving pesticides. It does not contain recommendations for their use, nor does it imply that the uses discussed here have been registered. All uses of pesticides must be registered by appropriate State and Federal agencies before they can be recommended. CAUTION: Pesticides can be injurious to humans, domestic animals, desirable plants, and fish or other wildlife—if they are not handled or applied properly. Use all pesticides selectively and carefully. Follow recommended practices for the disposal of surplus pesticides and pesticide containers. ¿/áepé4áaUÁí^a¡eé —' ■ -"" TMK LABIL Mention of a proprietary product in this publication does not constitute a guarantee or warranty by the U.S. Department of Agriculture over other products not mentioned. Washington, D.C. Issued July 1971 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, D.C. 20402 - Price 25 cents House Fly Attractants and Arrestants: Screening of Chemicals Possessing Cyanide, Thiocyanate, or Isothiocyanate Radicals BY M. S. MAYER, Entomology Research Division, Agricultural Research Service ^ Few chemicals possessing cyanide (-CN), thio- cyanate was slightly attractive to Musca domes- eyanate (-SCN), or isothiocyanate (~NCS) radi- tica, but it was considered to be one of the better cals have been tested as attractants for the house repellents for Phormia regina (Meigen). -
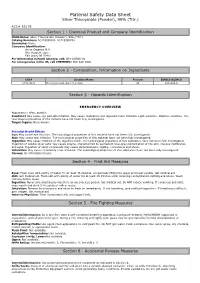
Material Safety Data Sheet
Material Safety Data Sheet Silver Thiocyanate (Powder), 99% (Titr.) ACC# 55179 Section 1 - Chemical Product and Company Identification MSDS Name: Silver Thiocyanate (Powder), 99% (Titr.) Catalog Numbers: AC419390000, AC419390250 Synonyms: None. Company Identification: Acros Organics N.V. One Reagent Lane Fair Lawn, NJ 07410 For information in North America, call: 800-ACROS-01 For emergencies in the US, call CHEMTREC: 800-424-9300 Section 2 - Composition, Information on Ingredients CAS# Chemical Name Percent EINECS/ELINCS 1701-93-5 Thiocyanic Acid, Silver(1+) Salt 99 216-934-9 Section 3 - Hazards Identification EMERGENCY OVERVIEW Appearance: white powder. Caution! May cause eye and skin irritation. May cause respiratory and digestive tract irritation. Light sensitive. Moisture sensitive. The toxicological properties of this material have not been fully investigated. Target Organs: None known. Potential Health Effects Eye: May cause eye irritation. The toxicological properties of this material have not been fully investigated. Skin: May cause skin irritation. The toxicological properties of this material have not been fully investigated. Ingestion: May cause irritation of the digestive tract. The toxicological properties of this substance have not been fully investigated. Ingestion of soluble silver salts may cause argyria, characterized by permanent blue-gray pigmentation of the skin, mucous membranes, and eyes. Ingestion of silver compounds may cause abdominal pain, rigidity, convulsions and shock. Inhalation: May cause respiratory tract irritation. The toxicological properties of this substance have not been fully investigated. Chronic: No information found. Section 4 - First Aid Measures Eyes: Flush eyes with plenty of water for at least 15 minutes, occasionally lifting the upper and lower eyelids. -
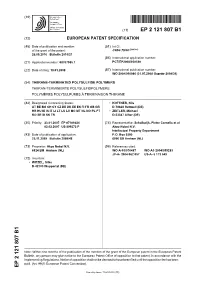
Thiirane-Terminated Polysulfide Polymers Thiiran-Terminierte Polysulfidpolymere Polymères Polysulfures À Terminaison Thiirane
(19) & (11) EP 2 121 807 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: C08G 75/00 (2006.01) 26.05.2010 Bulletin 2010/21 (86) International application number: (21) Application number: 08707985.1 PCT/EP2008/050540 (22) Date of filing: 18.01.2008 (87) International publication number: WO 2008/090086 (31.07.2008 Gazette 2008/31) (54) THIIRANE-TERMINATED POLYSULFIDE POLYMERS THIIRAN-TERMINIERTE POLYSULFIDPOLYMERE POLYMÈRES POLYSULFURES À TERMINAISON THIIRANE (84) Designated Contracting States: • KOTTNER, Nils AT BE BG CH CY CZ DE DK EE ES FI FR GB GR D-78628 Rottweil (DE) HR HU IE IS IT LI LT LU LV MC MT NL NO PL PT • ZEITLER, Michael RO SE SI SK TR D-53347 Alfter (DE) (30) Priority: 23.01.2007 EP 07101024 (74) Representative: Schalkwijk, Pieter Cornelis et al 02.02.2007 US 899273 P Akzo Nobel N.V. Intellectual Property Department (43) Date of publication of application: P.O. Box 9300 25.11.2009 Bulletin 2009/48 6800 SB Arnhem (NL) (73) Proprietor: Akzo Nobel N.V. (56) References cited: 6824 BM Arnhem (NL) WO-A-03/076487 WO-A1-2004/099283 JP-A- 2004 062 057 US-A- 5 173 549 (72) Inventors: • WITZEL, Silke D-42103 Wuppertal (DE) Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -

Thiocyanate Reagent Product Code R-1305K Recommended Use Use As Directed by Manufacturer for Purposes Directly Related to Water Testing
SAFETY DATA SHEET 1. Identification Product identifier Thiocyanate Reagent Product code R-1305K Recommended use Use as directed by manufacturer for purposes directly related to water testing. Recommended restrictions None known Manufacturer/Importer/Supplier/Distributor information Manufacturer Company name Anderson Chemical Company Address 325 South Davis Avenue Litchfield, MN 55355 United States Telephone (320) 693-2477 Monday─Friday, 8:00 a.m.–4:30 p.m. Website www.accomn.com E-mail [email protected] Emergency phone number (800) 424-9300 2. Hazard(s) identification Physical hazards This mixture does not meet the classification criteria according to OSHA HazCom 2012. Health hazards This mixture does not meet the classification criteria according to OSHA HazCom 2012. Environmental hazards Not currently regulated by OSHA. For additional information, refer to section 12 of the SDS. Label elements None required Signal word None required Hazard statement None required Precautionary statement Prevention None required Response None required Storage None required Disposal None required Hazard(s) not otherwise classified None Supplemental information None 3. Composition/information on ingredients Mixtures Chemical name Common name and synonyms CAS number % Deionized water Dihydrogen oxide 7732-18-5 95–99 Potassium thiocyanate Thiocyanic acid, potassium salt 333-20-0 0.1–5 4. First-aid measures Inhalation Move to fresh air. Give oxygen or artificial respiration if needed. Get medical attention immediately. Skin contact Immediately wash skin with soap and water. If symptoms persist or in all cases of concern, seek medical advice. Material name: Thiocyanate Reagent; R-1305K SDS U.S. Page 1 of 8 Eye contact Immediately flush eyes with plenty of water for at least 20 minutes. -

Ammonium Thiocyanate
AMMONIUM THIOCYANATE PRODUCT IDENTIFICATION CAS NO. 1762-95-4 EINECS NO. 217-175-6 FORMULA NH 4SCN MOL WT. 76.12 H.S. CODE 2838.00 TOXICITY Oral Rat LD50: 750 mg/kg SYNONYMS Thiocyanic acid, ammonium salt; Amthio; ammonium sulfocanide; ammonium sulphocyanide; ammonium rhodanide; ammonium sulphocyanate; Ammonium Rhodonide; Amthio; Ammonium sulfocyanate; DERIVATION CLASSIFICATION PHYSICAL AND CHEMICAL PROPERTIES PHYSICAL STATE Colorless, deliquescent crystals MELTING POINT 150 C BOILING POINT SPECIFIC GRAVITY 1.31 SOLUBILITY IN WATER Soluble SOLVENT SOLUBILITY Soluble : acetone, alcohol, and ammonia pH 4.5-6.0 (5% sol) VAPOR DENSITY AUTOIGNITION NFPA RATINGS Health: 2 Flammability: 1 Reactivity: 1 REFRACTIVE INDEX FLASH POINT 190 C STABILITY Stable under ordinary conditions APPLICATIONS Cyanic acid (the isomer of fulminic acid) is an unstable (explosive), poisonous, volatile, clear liquid with the structure of H-O-C¡ÕN (the oxoacid formed from the pseudohalogen cyanide), which is readily converted to cyamelide and fulminic acid. There is another isomeric cyanic acid with the structure of H-N=C=O, called isocyanic acid. Cyanate group (and isocyanate group) can react with itself. Cyanuric acid (also called pyrolithic acid), white monoclinic crystal with the structure of [HOC(NCOH) 2N], is the trimer of cyanic acid. The trimer of isocyanic acid is called biuret. • Cyanic acid: H-N=C=O or H-O-C¡ÕN • Fulminic acid: (H-C=N-O) or H-C¡ÕN-O • Isocyanic acid: H-N=C=O • Cyanuric acid: HOC(NCOH) 2N • Biuret: (NH 2)CO) 2 NH Cyanic acid hydrolyses to ammonia and carbon dioxide in water. The salts and esters of cyanic acid are cyanates.