Policy for COVID-19 Testing of Patients with Pre-Existing Tracheostomes (Tracheostomy/Laryngectomy)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

COVID-19 and Neonatal Respiratory Care: Current Evidence and Practical Approach
Published online: 2020-05-02 780 Review Article COVID-19 and Neonatal Respiratory Care: Current Evidence and Practical Approach Wissam Shalish, MD1 Satyanarayana Lakshminrusimha, MD2 Paolo Manzoni, MD3 Martin Keszler, MD4 Guilherme M. Sant’Anna, MD, PhD, FRCPC1 1 Neonatal Division, Department of Pediatrics, McGill University Address for correspondence Guilherme M. Sant’Anna, MD, PhD, Health Center, Montreal, Quebec, Canada FRCPC, Neonatal Division, Department of Pediatrics, McGill University 2 Department of Pediatrics, UC Davis, Sacramento, California Health Center, 1001 Décarie Boulevard, Room 05.2711, 3 Department of Pediatrics and Neonatology, University Hospital Montreal H4A 3J1, Canada (e-mail: [email protected]). Degli Infermi, Biella, Italy 4 Department of Pediatrics, Women and Infants Hospital, Brown University, Providence, Rhode Island Am J Perinatol 2020;37:780–791. Abstract The novel coronavirus disease 2019 (COVID-19) pandemic has urged the development and implementation of guidelines and protocols on diagnosis, management, infection control strategies, and discharge planning. However, very little is currently known about neonatal COVID-19 and severe acute respiratory syndrome–coronavirus-2 (SARS-CoV-2) infections. Thus, many questions arise with regard to respiratory care after birth, necessary protection to health care workers (HCW) in the delivery room and neonatal intensive care unit (NICU), and safety of bag and mask ventilation, noninvasive respiratory support, deep suctioning, endotracheal intubation, and mechanical ventilation. Indeed, these questions have created tremendous confusion amongst neonatal HCW. In this manuscript, we comprehensively reviewed the current evidence regarding COVID-19 perinatal transmission, respiratory outcomes of neonates born to mothers with COVID-19 and infants with documented SARS- CoV-2 infection, and the evidence for using different respiratory support modalities and aerosol-generating procedures in this specific population. -

COVID-19 and Total Laryngectomy—A Report of Two Cases
AORXXX10.1177/0003489420935500Annals of Otology, Rhinology & LaryngologyPaderno et al 935500case-report2020 Case Report Annals of Otology, Rhinology & Laryngology 1 –4 COVID-19 and Total Laryngectomy © The Author(s) 2020 Article reuse guidelines: sagepub.com/journals-permissions —A Report of Two Cases DOI:https://doi.org/10.1177/0003489420935500 10.1177/0003489420935500 journals.sagepub.com/home/aor Alberto Paderno, MD1 , Milena Fior, MD1, Giulia Berretti, MD1, Francesca Del Bon, MD1, Alberto Schreiber, MD, PhD1, Alberto Grammatica, MD1, Davide Mattavelli, MD1, and Alberto Deganello, MD, PhD1 Abstract Objective: To date, no cases have been reported on the effects of COVID-19 in laryngectomees. Case Presentation: We herein presented two clinical cases of laryngectomized patients affected by COVID-19, detailing their clinical course and complications. Discussion: In our experience, permanent tracheostomy did not significantly affect the choice of treatment. However, dedicated devices and repeated tracheal toilettes may be needed to deal with oxygen-therapy-related tracheal crusting. Conclusion: In conclusion, laryngectomees should be considered a vulnerable population that may be at risk for worse outcomes of COVID-19 due to anatomical changes in their airways. The role of the ENT specialist is to guide airway management and inform the support-staff regarding specific needs of these patients. Keywords COVID-19, coronavirus, SARS-CoV-2, laryngectomy, management Introduction At admission (March 9, 2020), the most relevant clinical findings included severe oxygen desaturation (76%), tachy- To date, the effects of COVID-19 on laryngectomized pnea, cyanosis, lymphocytopenia, and C reactive protein patients is unknown, with no cases reported so far. After (CRP; 185 mg/L). -

Effectiveness and Superiority of Ventilation with Laryngeal Mask
a & hesi C st lin e ic n a A l f R o e l s Journal of Anesthesia & Clinical e a a n r r Wu et al., J Anesth Clin Res 2017, 8:7 c u h o J DOI: 10.4172/2155-6148.1000738 ISSN: 2155-6148 Research Research Article Open Access Effectiveness and Superiority of Ventilation with Laryngeal Mask Airway in Partial Laryngectomy Jinhong Wu, Weixing Li and Wenxian Li* Department of Anesthesiology, Eye, Ear, Nose and Throat Hospital, Fudan University, China *Corresponding author: Wenxian Li, Department of Anesthesiology, Eye, Ear, Nose and Throat Hospital, Fudan University, 83 Fenyang Road, Xuhui District, Shanghai 200031, China, Tel: +86-21-64377134; Fax: +86-21-64377151; E-mail: [email protected] Received date: Jun 06, 2017; Accepted date: Jul 01, 2017; Published date: Jul 04, 2017 Copyright: © 2017 Wu J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Background: Laryngeal carcinoma occupies the space of glottis. It may lead to difficult airway, and is prone to bleed if intubated with endotracheal tube (ETI). Intubation can also result in the possibility of tumor cultivation in the lung. Use of laryngeal mask airway (LMA) could avoid the disadvantages of endotracheal intubation, which would benefit patients undergoing partial laryngectomy. Methods: This was a randomized controlled clinical trial. Thirty adult patients scheduled to receive partial laryngectomy were enrolled. All study subjects received an ASA rating of grade III. -

Gemstone Spectral Imaging Technique
Gemstone Spectral Imaging HANDBOOK OF CLINICAL EVIDENCE for Radiologists and Radiographers Vascular Performance Artefact Innovation Reduction Technology Material Decomposition Oncology gehealthcare.com Introduction Diagnostic Imaging is a fast-moving field harvesting the latest technologies from the newest in hardware capabilities to the first artificial intelligence applications in radiology. The objective is improving patient clinical outcomes and we are now expecting to go beyond by improving the patient pathway, reducing the number of exams and giving access to the right diagnosis, effortlessly. CT imaging has quickly become the cornerstone of imaging departments, not only providing more and more anatomical information by improving image quality, but also taking the lead in functional information to really assess the impact of disease. Gemstone™ Spectral Imaging (GSI) is the avenue to answer challenging clinical questions by using a single scan to provide both anatomical and functional information in one study thereby reducing the number of exams needed to deliver a diagnosis. This technique is widely accepted by clinical societies and peer reviewed publications show patient & clinical outcomes. Through this handbook, you will find the latest uses of our GSI technology, its outcomes and real testimonials from our users. We truly want to help you integrate this into your daily clinical practice in multiple clinical applications to further add value to your patient care pathway in CT. We have gathered infographics illustrating the use of GSI, clinical examples from all over Europe and a brief literature review. This handbook is for your patients, for your team and for you. We hope you find it valuable and as always contact your GE Healthcare representative if you have any questions. -

ACR Manual on Contrast Media
ACR Manual On Contrast Media 2021 ACR Committee on Drugs and Contrast Media Preface 2 ACR Manual on Contrast Media 2021 ACR Committee on Drugs and Contrast Media © Copyright 2021 American College of Radiology ISBN: 978-1-55903-012-0 TABLE OF CONTENTS Topic Page 1. Preface 1 2. Version History 2 3. Introduction 4 4. Patient Selection and Preparation Strategies Before Contrast 5 Medium Administration 5. Fasting Prior to Intravascular Contrast Media Administration 14 6. Safe Injection of Contrast Media 15 7. Extravasation of Contrast Media 18 8. Allergic-Like And Physiologic Reactions to Intravascular 22 Iodinated Contrast Media 9. Contrast Media Warming 29 10. Contrast-Associated Acute Kidney Injury and Contrast 33 Induced Acute Kidney Injury in Adults 11. Metformin 45 12. Contrast Media in Children 48 13. Gastrointestinal (GI) Contrast Media in Adults: Indications and 57 Guidelines 14. ACR–ASNR Position Statement On the Use of Gadolinium 78 Contrast Agents 15. Adverse Reactions To Gadolinium-Based Contrast Media 79 16. Nephrogenic Systemic Fibrosis (NSF) 83 17. Ultrasound Contrast Media 92 18. Treatment of Contrast Reactions 95 19. Administration of Contrast Media to Pregnant or Potentially 97 Pregnant Patients 20. Administration of Contrast Media to Women Who are Breast- 101 Feeding Table 1 – Categories Of Acute Reactions 103 Table 2 – Treatment Of Acute Reactions To Contrast Media In 105 Children Table 3 – Management Of Acute Reactions To Contrast Media In 114 Adults Table 4 – Equipment For Contrast Reaction Kits In Radiology 122 Appendix A – Contrast Media Specifications 124 PREFACE This edition of the ACR Manual on Contrast Media replaces all earlier editions. -

Closed Rhinoplasty: Effects and Changes on Voice - a Preliminary Report
Topic: EuRePS Meeting 2015: best five papers Closed rhinoplasty: effects and changes on voice - a preliminary report Giuseppe Guarro, Romano Maffia, Barbara Rasile, Carmine Alfano Department of Plastic and Reconstructive Surgery, University of Perugia, 06156 Perugia, Italy. Address for correspondence: Dr. Giuseppe Guarro, Department of Plastic and Reconstructive Surgery, University of Perugia, S. Andrea delle Fratte, 06156 Perugia, Italy. E-mail: [email protected] ABSTRACT Aim: Effects of rhinoplasty were already studied from many points of view: otherwise poor is scientific production focused on changes of voice after rhinoplasty. This preliminary study analyzed objectively and subjectively these potential effects on 19 patients who underwent exclusively closed rhinoplasty. Methods: This preliminary evaluation was conducted from September 2012 to May 2013 and 19 patients have undergone primary rhinoplasty with exclusively closed approach (7 males, 12 females). All patients were evaluated before and 6 months after surgery. Each of them answered to a questionnaire (Voice Handicap Index Score) and the voice was recorded for spectrographic analysis: this system allowed to perform the measurement of the intensity and frequency of vowels (“A” and “E”) and nasal consonants (“N” and “M”) before and after surgery. Data were analysed with the Mann-Whitney test. Results: Sixteen patients showed statistically significant differences after surgery. It was detected in 69% of cases an increased frequency of emission of the consonant sounds (P = 0.046), while in 74% of cases the same phenomenon was noticed for vowel sounds (P = 0.048). Conclusion: Many patients who undergo rhinoplasty think that the intervention only leads to anatomical changes and improvement of respiratory function. -

COVID 19 Inpatient Testing Guidelines
COVID-19 Inpatient COVID-19 Testing Protocol, Version 7, 20210714 Owners: T. Bouton, J. Hudspeth Inpatient COVID-19 Testing Protocol A. Who to test? BMC tests all patients being admitted to the hospital, with the exception of COVID- recovered patients who are within 9 months of their initial positive COVID test and remain asymptomatic (for outpatient testing algorithms, please refer to the outpatient testing protocol). o Refer to COVID-Flu Testing Winter 2020 for guidance on testing patients admitted with flu-like febrile respiratory illness and sepsis-like syndrome requiring hospitalization. If a patient who is already admitted develops symptoms potentially attributable to COVID- 19 and warrants testing per your clinical opinion, they should be retested (even if their admission test was negative). Note: For COVID-recovered patients who have new symptoms of COVID-19 within 9 months of initial positive test AND for whom an alternate etiology cannot be identified, also consider retesting. o Promptly alert the nurse of your concern so precautions are instituted o There are a wide range of symptoms and presentations potentially compatible with COVID including: Fever, cough, shortness of breath, new anosmia, unexplained hypoxia, diarrhea (more than 3 watery bowel movements per day), nausea or vomiting, dizziness, headache, muscle aches, throat pain, rhinorrhea, fatigue and others. o In accordance with guidelines, testing should be conducted for patients with: . ST elevation MI . Unprovoked venous thromboembolism . Multifocal PNA or ground glass opacities on CT without clear alternative diagnosis o Diagnoses for which one should consider testing for COVID: . New seizure . New stroke . Myocarditis, stress cardiomyopathy, coronary spasm, right heart failure Direct admissions to BMC should be assessed for symptoms of COVID (or results of prior COVID testing) by the accepting physician prior to accepting the patient. -

Laryngectomy
The Head+Neck Center John U. Coniglio, MD, LLC 1065 Senator Keating Blvd. Suite 240 Rochester, NY 14618 Office Hours: 8-4 Monday-Friday t 585.256.3550 f 585.256.3554 www.RochesterHNC.com Laryngectomy SINUS Voice change, difficulty swallowing, unexplained weight loss, ear or ENDOCRINE HEAD AND NECK CANCER throat pain and a lump in the throat, smoking and alcohol use are all VOICE DISORDERS SALIVARY GLANDS indications for further evaluation. Smoking and alcohol can contribute TONSILS AND ADENOIDS to these symptoms. A direct laryngoscopy – an exam of larynx (voice EARS PEDIATRICS box), with biopsy – will help determine if a laryngectomy is indicated. SNORING / SLEEP APNEA Laryngectomy may involve partial or total removal of one or more or both vocal cords. Alteration of voice will occur with either total or partial laryngectomy. Postoperative rehabilitation is usually successful in helping the patient recover a voice that can be understood. The degree of alteration in voice depends on the extent of the disease. Partial or total laryngectomy has been a highly successful method to remove cancer of the larynx. The extent of the tumor invasion, and therefore the extent of surgery, determines the way you will communicate following surgery. The choice of surgery over other forms of treatment such as radiation or chemotherapy is determined by the site of the tumor. It is quite likely that there has been spread of the tumor to the neck; a neck or lymph node dissection may also be recommended. Complete neck dissection (exploration of the neck tissues) is performed in order to remove known or suspected lymph nodes containing cancer that has spread from the primary tumor site. -

Laryngectomy
LARYNGECTOMY Definitlon Laryngectomy is the partial or complete surgical removal of the larynx, usually as a treatment for cancer of the larynx. Purpose Normally a laryngectomy is performed to remove tumors or cancerous tissue. In rare cases, it may be done when the larynx is badly damaged by gunshot, automobile injuries, or similar violent accidents. Laryngectomies can be total or partial. Total laryngectomies are done when cancer is advanced. The entire larynx is removed. Often if the cancer has spread, other surrounding structures in the neck, such as lymph nodes, are removed at the same time. Partial laryngectomies are done when cancer is limited to one spot. Only the area with the tumor Is removed. Laryngectomies may also be performed when other cancer treatment options, such as radiation or chemotherapy. fail. Precautions Laryngectomy is done only after cancer of the larynx has been diagnosed by a series of tests that allow the otolaryngologist (a specialist often called an ear, nose, and throat doctor) to look into the throat and take tissue samples (biopsies) to confirm and stage the cancer. People need to be in good general health to undergo a laryngectomy, and will have standard pre-operative blood work and tests to make sure they are able to safely withstand the operation. Description The larynx is located slightly below the point where the throat divides into the esophagus, which takes food to the stomach, and the trachea (windpipe), which takes air to the lungs. Because of its location, the larynx plays a critical role in normal breathing, swallowing, and speaking. -

Disparate Nasopharyngeal and Tracheal COVID-19 Diagnostic Test
Revised complete Manuscript Click here to access/download;Complete Manuscript;laryngectomy Testing manuscript plaintext.docx This manuscript has been accepted for publication in Otolaryngology-Head and Neck Surgery. 1 1 Disparate Nasopharyngeal and Tracheal COVID-19 Diagnostic Test 2 Results in a Patient with Total Laryngectomy 3 Running Title: “COVID-19 Testing with Total Laryngectomy” 4 5 Tirth R. Patel, MD1; Joshua E. Teitcher, CCC-SLP2; Bobby A. Tajudeen, MD1; Peter C. 6 Revenaugh, MD1 7 8 1. Department of Otolaryngology—Head and Neck Surgery, Rush University Medical 9 Center, Chicago, Illinois 10 2. Department of Hematology/Oncology, Rush University Medical Center, Chicago, Illinois 11 12 Corresponding Author: 13 Tirth R. Patel, MD 14 Department of Otolaryngology—Head and Neck Surgery 15 Rush University Medical Center 16 1650 West Harrison Street, Suite 550 17 Chicago, Illinois 60612 18 Phone: 312-942-6100 19 Email: [email protected] 20 21 22 Keywords: COVID-19, coronavirus, laryngectomy 23 Sponsor or Funding Source: None 24 Conflicts of Interest: None 25 26 Author Contributions: 27 T.R.P.: Conception and design; data acquisition; drafting, revision, final approval of article 28 J.E.T.: Conception and design; data acquisition; drafting, revision, final approval of article 29 B.A.T.: Conception and design; drafting, revision, final approval of article 30 P.C.R.: Conception and design; drafting, revision, final approval of article 31 32 This manuscript has been accepted for publication in Otolaryngology-Head and Neck Surgery. This manuscript has been accepted for publication in Otolaryngology-Head and Neck Surgery. 2 33 Introduction 34 Coronavirus disease 2019 (COVID-19), caused by SARS-CoV-2 virus, has been declared 35 a pandemic by the World Health Organization1. -

Microbiology Specimen Collection
Martin Health System Stuart, Florida Laboratory Services Microbiology Specimen Collection The recovery of pathogenic organisms responsible for an infectious process is dependent on proper collection and transportation of a specimen. An improperly collected or transported specimen may lead to failure to isolate the causative organism(s) of an infectious disease or may result in the recovery and subsequent treatment of contaminating organisms. Improper handling of specimens may also lead to accidental exposure to infectious material. GENERAL GUIDELINES FOR COLLECTION: 1. Follow universal precaution guidelines, treating all specimens as potentially hazardous. 2. Whenever possible, collect specimen before antibiotics are administered. 3. Collect the specimen from the actual site of infection, avoiding contamination from adjacent tissues or secretions. 4. Collect the specimen at optimal time i.e. Early morning sputum for AFB First voided specimen for urine culture Specimens ordered x 3 should be 24 hours apart (exception: Blood cultures which are collected as indicated by the physician) 5. Collect sufficient quantity of material for tests requested. 6. Use appropriate collection and transport container. Refer to the Microbiology Quick Reference Chart or to the specific source guidelines. Containers should always be tightly sealed and leak-proof 7. Label the specimen with the Patient’s First and Last Name Date of Birth Collection Date and Time Collector’s First and Last Name Source 8. Submit specimen in the sealed portion of a Biohazard specimen bag. 9. Place signed laboratory order in the outside pocket of the specimen bag. 10. Include any pertinent information i.e. recent travel or relocation, previous antibiotic therapy, unusual suspected organisms, method or environment of wound infliction 11. -
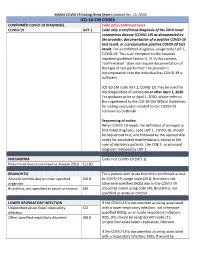
Icd-10-Cm Codes
MGMA COVID-19 Coding Cheat Sheet (Updated Dec. 23, 2020) ICD-10-CM CODES CONFIRMED COVID-19 DIAGNOSIS Code only confirmed cases COVID-19 U07.1 Code only a confirmed diagnosis of the 2019 novel coronavirus disease (COVID-19) as documented by the provider, documentation of a positive COVID-19 test result, or a presumptive positive COVID-19 test result. For a confirmed diagnosis, assign code U07.1, COVID-19. This is an exception to the hospital inpatient guideline Section II, H. In this context, “confirmation” does not require documentation of the type of test performed; the provider’s documentation that the individual has COVID-19 is sufficient. ICD-10-CM code U07.1, COVID-19, may be used for discharges/date of service on or after April 1, 2020. For guidance prior to April 1, 2020, please refer to the supplement to the ICD-10-CM Official Guidelines for coding encounters related to the COVID-19 coronavirus outbreak. Sequencing of codes: When COVID-19 meets the definition of principal or first-listed diagnosis, code U07.1, COVID-19, should be sequenced first, and followed by the appropriate codes for associated manifestations, except in the case of obstetrics patients. Use O98.5- as principal diagnosis followed by U07.1. PNEUMONIA Code first COVID-19 (U07.1) Pneumonia due to coronavirus disease 2019 J12.82 BRONCHITIS For a patient with acute bronchitis confirmed as due Acute bronchitis due to other specified J20.8 to COVID-19, assign code J20.8. Bronchitis not organism otherwise specified (NOS) due to the COVID-19 Bronchitis, not specified as acute or chronic J40 should be coded using code J40, Bronchitis, not specified as acute or chronic.