CONJUNCTIVA: Inflammatory and Degenerative Lesions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tear Film Break-Up Time and Dry Eye Disease Severity in a Large Norwegian Cohort
Journal of Clinical Medicine Article Tear Film Break-Up Time and Dry Eye Disease Severity in a Large Norwegian Cohort Mazyar Yazdani 1,2,* , Jørgen Fiskådal 1, Xiangjun Chen 1,3,4, Øygunn A. Utheim 1,2,5, Sten Ræder 1, Valeria Vitelli 6 and Tor P. Utheim 1,2,3,4,5,7,8 1 The Norwegian Dry Eye Clinic, 0366 Oslo, Norway; jorgen_fi[email protected] (J.F.); [email protected] (X.C.); [email protected] (Ø.A.U.); [email protected] (S.R.); [email protected] (T.P.U.) 2 Department of Medical Biochemistry, Oslo University Hospital, 0450 Oslo, Norway 3 Department of Oral Surgery and Oral Medicine, University of Oslo, 0317 Oslo, Norway 4 Department of Ophthalmology, Sørlandet Hospital Arendal, 4604 Arendal, Norway 5 Department of Ophthalmology, Oslo University Hospital, 0450 Oslo, Norway 6 Oslo Center for Biostatistics and Epidemiology, Department of Biostatistics, University of Oslo, Sognsvannsveien 9, 0372 Oslo, Norway; [email protected] 7 Department of Ophthalmology, Stavanger University Hospital, 4011 Stavanger, Norway 8 Department of Plastic and Reconstructive Surgery, Oslo University Hospital, 0450 Oslo, Norway * Correspondence: [email protected] Abstract: This study evaluated to what extent tear film break-up time (TFBUT) could discriminate pathological scores for other clinical tests and explore the associations between them. Dry eye patients (n = 2094) were examined for ocular surface disease index (OSDI), tear film osmolarity (Osm), TFBUT, blink interval, ocular protection index (OPI), ocular surface staining (OSS), Schirmer I test, meibomian expressibility, meibomian quality, and meibomian gland dysfunction. The results were grouped into eight levels of break-up time (≤2, ≥3, ≤5, ≥6, ≤10, ≥11, ≤15, and ≥16) with or without sex stratification. -

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -

Spontaneous and Reflex Activity of Facial Muscles in Dystonia
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.64.3.320 on 1 March 1998. Downloaded from 320 J Neurol Neurosurg Psychiatry 1998;64:320–324 Spontaneous and reflex activity of facial muscles in dystonia, Parkinson’s disease, and in normal subjects Günther Deuschl, Christof Goddemeier Abstract darkness or blindness change blink rate only to Objective—The blink rate is an index a limited extent.1 However, physiological fac- which can be easily obtained during the tors related to the subjects’ general status clinical examination, but it has not yet including attention seem to be much more been properly standardised. The present important.12 study was undertaken to collect data on From the neurological point of view central the age dependent development of this regulation of the blink rate is of special interest index and on possible abnormalities in as diVerent pathological conditions can modu- Parkinson’s disease and dystonia. late the blink rate. Reduction of the blink rate Methods—The blink rate and the rate of has been found in Parkinson’s disease,3 in pro- perioral movements were measured in 156 gressive supranuclear palsy,4 and in subjects normal controls, 51 patients with Parkin- taking dopamine receptor blockers.5 This son’s disease, 48 patients with spasmodic reduction is considered to be such a well torticollis, 14 patients with generalised defined feature of Parkinson’s disease that it is dystonia, and 12 patients with focal hand even part of an item of the unified Parkinson’s or leg dystonias and have been correlated disease rating scale.6 An increase of the blink with the results of testing the orbicularis rate has not yet been established as a diagnos- oculi reflex, the palmomental reflex, and tic sign although it has been found in some the perioral reflex. -

Evaluation of the Eyebrow Position After External Müller's Muscle
Journal of Plastic, Reconstructive & Aesthetic Surgery (2019) 72, 662–668 Evaluation of the eyebrow position after external Müller’s muscle tucking: A new technique for ptosis repair a , ∗ b c Kenichi Kokubo , Nobutada Katori , Kengo Hayashi , d e f a Jun Sugawara , Seiko Kou , Akiko Fujii , Shoko Haga , f Jiro Maegawa a Department of Plastic Surgery, Fujisawa Shounandai Hospital. 2345 Takakura, Fujisawa-shi, Kanagawa 251-0802, Japan b Department of Ocular Plastic & Orbital Surgery, Seirei Hamamatsu General Hospital. 2-12-12 Sumiyoshi, Naka-ku, Hamamatsu-shi, Shizuoka 430-8558, Japan c Yokohama Sakuragicho Eye Clinic. 1-200 Hinodecho, Naka-ku Yokohama-shi, Kanagawa 231-0006, Japan d JUN CLINIC, 1402-5 Kitaishidocho, Nagano-shi, Nagano 380-0826, Japan e KO CLINIC for Antiaging. 4-54 Onoecho, Naka-ku Yokohama-shi, Kanagawa 231-0015, Japan f Department of Plastic and Reconstructive Surgery, Yokohama City University Hospital. 3-9 Fukuura, Kanazawa-ku, Yokohama-shi, Kanagawa 236-0004, Japan Received 27 August 2018; accepted 6 January 2019 KEYWORDS Summary Eyebrow descent commonly occurs after ptosis repair or blepharoplasty surgery. Müller’s muscle; The procedures used to correct acquired blepharoptosis are primarily classified into four Eyebrow position; groups. These procedures target the levator aponeurosis, Müller’s muscle, both the aponeu- Blepharoptosis; rosis and Müller’s muscle, or the frontalis muscle. In this study, we used a new technique called MRD; external Müller’s muscle tucking (EMMT) on 51 patients (94 eyelids), which targets the Müller’s Ptosis repair muscle for involutional blepharoptosis. The patients were assessed by comparative analysis us- ing pre- and post-operative digital photographs. -

Conjunctival Flora of Normal Human Eye Which Vary with Age, Sex, Geographical Distribution, Right and Left Eye
Central JSM Ophthalmology Research Article *Corresponding author Purnima Rajkarnikar Sthapit, Department of Ophthalmology, Dhulikhel Hospital, Kathmandu Conjunctival Flora of Normal University Hospital, Dhulikhel, Kavre, Nepal, Tel: 009779813254962; Fax: 0097711490707; Email: Human Eye Submitted: 23 February 2014 Purnima Rajkarnikar Sthapit1* and Nhuchhe Ratna Tuladhar2 Accepted: 03 March 2014 1Department of Ophthalmology, Kathmandu University School of Medical Sciences, Nepal Published: 07 March 2014 2Department of Microbiology, Kathmandu University School of Medical Sciences, Nepal ISSN: 2333-6447 Copyright Abstract © 2014 Sthapit et al. Background: The normal flora of the eye plays an important role in maintaining OPEN ACCESS ocular homeostasis by various mechanisms. They comprise of mainly bacteria which do not cause infection in normal conditions but can be a main source of infection after Keywords ocular surgery, trauma or in immune compromised. The ranges of these microorganisms • Coagulase positive Staphylococcus vary with age, sex and geographical distribution. Therefore it is very important for the • Normal flora ophthalmologist to know the ocular normal flora before giving prophylactic antibiotics • Ocular infection and treating infections. • Ocular trauma Objectives: To describe the conjunctival flora of normal human eye which vary with age, sex, geographical distribution, right and left eye. Methodology: A total of 200 conjunctival swabs from 100 patients with healthy eyes were sent for microbiological evaluation to describe the various microorganisms isolated as normal flora of conjunctiva. Result: The growth of bacteria was seen in 78.5% of patients, the commonest flora isolated was Coagulase negative Staphylocccus in 51%. Greater number of male patients had sterile conjunctiva than females and conjunctiva of old people were found to be increasingly more colonised than young. -

The Complexity and Origins of the Human Eye: a Brief Study on the Anatomy, Physiology, and Origin of the Eye
Running Head: THE COMPLEX HUMAN EYE 1 The Complexity and Origins of the Human Eye: A Brief Study on the Anatomy, Physiology, and Origin of the Eye Evan Sebastian A Senior Thesis submitted in partial fulfillment of the requirements for graduation in the Honors Program Liberty University Spring 2010 THE COMPLEX HUMAN EYE 2 Acceptance of Senior Honors Thesis This Senior Honors Thesis is accepted in partial fulfillment of the requirements for graduation from the Honors Program of Liberty University. ______________________________ David A. Titcomb, PT, DPT Thesis Chair ______________________________ David DeWitt, Ph.D. Committee Member ______________________________ Garth McGibbon, M.S. Committee Member ______________________________ Marilyn Gadomski, Ph.D. Assistant Honors Director ______________________________ Date THE COMPLEX HUMAN EYE 3 Abstract The human eye has been the cause of much controversy in regards to its complexity and how the human eye came to be. Through following and discussing the anatomical and physiological functions of the eye, a better understanding of the argument of origins can be seen. The anatomy of the human eye and its many functions are clearly seen, through its complexity. When observing the intricacy of vision and all of the different aspects and connections, it does seem that the human eye is a miracle, no matter its origins. Major biological functions and processes occurring in the retina show the intensity of the eye’s intricacy. After viewing the eye and reviewing its anatomical and physiological domain, arguments regarding its origins are more clearly seen and understood. Evolutionary theory, in terms of Darwin’s thoughts, theorized fossilization of animals, computer simulations of eye evolution, and new research on supposed prior genes occurring in lower life forms leading to human life. -

Eyelid Conjunctival Tumors
EYELID &CONJUNCTIVAL TUMORS PHOTOGRAPHIC ATLAS Dr. Olivier Galatoire Dr. Christine Levy-Gabriel Dr. Mathieu Zmuda EYELID & CONJUNCTIVAL TUMORS 4 EYELID & CONJUNCTIVAL TUMORS Dear readers, All rights of translation, adaptation, or reproduction by any means are reserved in all countries. The reproduction or representation, in whole or in part and by any means, of any of the pages published in the present book without the prior written consent of the publisher, is prohibited and illegal and would constitute an infringement. Only reproductions strictly reserved for the private use of the copier and not intended for collective use, and short analyses and quotations justified by the illustrative or scientific nature of the work in which they are incorporated, are authorized (Law of March 11, 1957 art. 40 and 41 and Criminal Code art. 425). EYELID & CONJUNCTIVAL TUMORS EYELID & CONJUNCTIVAL TUMORS 5 6 EYELID & CONJUNCTIVAL TUMORS Foreword Dr. Serge Morax I am honored to introduce this Photographic Atlas of palpebral and conjunctival tumors,which is the culmination of the close collaboration between Drs. Olivier Galatoire and Mathieu Zmuda of the A. de Rothschild Ophthalmological Foundation and Dr. Christine Levy-Gabriel of the Curie Institute. The subject is now of unquestionable importance and evidently of great interest to Ophthalmologists, whether they are orbital- palpebral specialists or not. Indeed, errors or delays in the diagnosis of tumor pathologies are relatively common and the consequences can be serious in the case of malignant tumors, especially carcinomas. Swift diagnosis and anatomopathological confirmation will lead to a treatment, discussed in multidisciplinary team meetings, ranging from surgery to radiotherapy. -

A Rare Presentation of Lower Conjunctival Fornix Eyelashes Cyst Dr Mohammad Aldroos (MD)* *Department of Ophthalmology, Jordanian Royal Medical Services
Int J Biol Med Res.2018 ;9(1):6259-6260 Int J Biol Med Res www.biomedscidirect.com Volume 6, Issue 2, April 2015 Contents lists available at BioMedSciDirect Publications International Journal of Biological & Medical Research Journal homepage: www.biomedscidirect.com BioMedSciDirect International Journal of Publications BIOLOGICAL AND MEDICAL RESEARCH Case report A rare presentation of lower conjunctival fornix eyelashes cyst Dr Mohammad Aldroos (MD)* *Department of Ophthalmology, Jordanian Royal Medical Services A R T I C L E I N F O A B S T R A C T Keywords: Purpose: To describe a rare presentation of a right lower conjunctival fornix eyelashes cyst. Case Report: A 56 year-old lady presented to our clinic complaining of blackish mass in the lower conjunctival fornix of the right eye ( see fig.1), with mild conjunctival hyperemia around the mass. There was no history of discharge and difficulty in extraocular muscles movements also there was no history of trauma. A gradually enlarging mass over the past few years with recurrent conjunctivitis. Slit lamp examination of the mass showed normal appearing eyelashes surrounded by capsule only. The mass was surgically excised with good cosmetic appearance and without any complications c Copyright 2010 BioMedSciDirect Publications IJBMR - ISSN: 0976:6685. All rights reserved. Introduction Fig.2 Eyelashes grow on the edge of the eyelid. A normal eyelid has a single row of eyelashes located along its anterior margin. The posterior portion of the lid contains a row of Meibomian glands orifices, which secrete the oily component of the tear film (1). There are approximately 100 eye lashes on the upper lid and approximately 50-75 on the lower lid, they protect the eyeball. -

Dualblink: a Wearable Device to Continuously Detect, Track, and Actuate Blinking for Alleviating Dry Eyes and Computer Vision Syndrome
1 DualBlink: A Wearable Device to Continuously Detect, Track, and Actuate Blinking For Alleviating Dry Eyes and Computer Vision Syndrome ARTEM DEMENTYEV, Microsoft Research, Redmond & MIT Media Lab CHRISTIAN HOLZ, Microsoft Research, Redmond Increased visual attention, such as during computer use leads to less blinking, which can cause dry eyes—the leading cause of computer vision syndrome. As people spend more time looking at screens on mobile and desktop devices, computer vision syndrome is becoming epidemic in today’s population, leading to blurry vision, fatigue, and a reduced quality of life. One way to alleviate dry eyes is increased blinking. In this paper, we present a series of glasses-mounted devices that track the wearer’s blink rate and, upon absent blinks, trigger blinks through actuation: light ashes, physical taps, and small pus of air near the eye. We conducted a user study to evaluate the eectiveness of our devices and found that air pu and physical tap actuations result in a 36% increase in participants’ average blink rate. Air pu thereby struck the best compromise between eective blink actuations and low distraction ratings from participants. In a follow-up study, we found that high intensity, short pus near the eye were most eective in triggering blinks while receiving only low-rated distraction and invasiveness ratings from participants. We conclude this paper with two miniaturized and self-contained DualBlink prototypes, one integrated into the frame of a pair of glasses and the other one as a clip-on for existing glasses. We believe that DualBlink can serve as an always-available and viable option to treat computer vision syndrome in the future. -
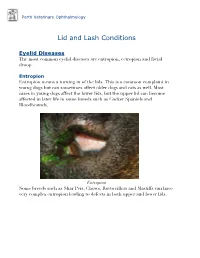
Lid and Lash Conditions
Perth Veterinary Ophthalmology Lid and Lash Conditions Eyelid Diseases The most common eyelid diseases are entropion, ectropion and facial droop. Entropion Entropion means a turning in of the lids. This is a common complaint in young dogs but can sometimes affect older dogs and cats as well. Most cases in young dogs affect the lower lids, but the upper lid can become affected in later life in some breeds such as Cocker Spaniels and Bloodhounds. Entropion Some breeds such as Shar Peis, Chows, Rottweillers and Mastiffs can have very complex entropion leading to defects in both upper and lower lids. A Shar Pei with severe upper and lower lid entropion Entropion is painful and can be potentially blinding. The rolling in of the lid leads to hair coming into contact with the cornea, leading to pain, ulceration and scarring (which can affect vision). In severe cases this can even lead to perforation of the eye. There are many causes of entropion. It can be primary or secondary to other problems affecting the lids (such as ectopic cilia, distichiasis etc. - see below). Some possible causes include the lid being too long, the lid being too tight, instability of the lateral canthus (outer cornea of the eyelids), misdirection of the lateral canthal tendon, brachycephalic anatomy (big eyes and short nose - e.g. Pekingese, Pugs, Shih Tsus, Persian cats etc.), diamond eye defects, loose or too much skin, facial droop etc. Often these cases are referred to a veterinary ophthalmologist for proper assessment and treatment to provide the best outcome. Entropion requires surgical correction. -

Observations Upon the Movements of the Eyelids* by G
Br J Ophthalmol: first published as 10.1136/bjo.35.6.339 on 1 June 1951. Downloaded from Brit. J. Ophthal., 35, 339. OBSERVATIONS UPON THE MOVEMENTS OF THE EYELIDS* BY G. GORDON Laboratory ofPhysiology, Oxford University THE human M. orbicularis oculi takes part in many patterns of movement. Some of these, like the- corneal reflex, the narrowing of the palpebral orifice in bright light, or the adjustments which accompany upward or downward rotation. of the eyeball, are connected in a comprehensible way with the eye itself. The muscle also plays its part in complex movements of the face, such as smiling. A third and particularly interesting type of movement is that of unconscious blinking, the pattern of which is undoubtedly related to visual perception (Hall, 1945), but which nevertheless occurs with about the normal frequency both in the blind, and in subjects in whom the cornea has been made anaesthetic (Ponder and Kennedy, 1928). copyright. It is known from direct observation that there is some functional subdivision between the different anatomical regions ofthe orbicularis (Gad, 1883; Whitnall, 1921), and an attempt is made in this communication to amplify these earlier descriptions by means of electromyographic observations. It was found in the course of another investigation (Gordon and Holbourn, 1948) that the action http://bjo.bmj.com/ potentials of single motor units could easily be recorded by means of wire electrodes placed upon the surface of the eyelids, and in this way one may get definite information about the activity of the motor neurones supplying this muscle. The opportunity has also been taken to investigate the activity of M. -

Nomina Histologica Veterinaria, First Edition
NOMINA HISTOLOGICA VETERINARIA Submitted by the International Committee on Veterinary Histological Nomenclature (ICVHN) to the World Association of Veterinary Anatomists Published on the website of the World Association of Veterinary Anatomists www.wava-amav.org 2017 CONTENTS Introduction i Principles of term construction in N.H.V. iii Cytologia – Cytology 1 Textus epithelialis – Epithelial tissue 10 Textus connectivus – Connective tissue 13 Sanguis et Lympha – Blood and Lymph 17 Textus muscularis – Muscle tissue 19 Textus nervosus – Nerve tissue 20 Splanchnologia – Viscera 23 Systema digestorium – Digestive system 24 Systema respiratorium – Respiratory system 32 Systema urinarium – Urinary system 35 Organa genitalia masculina – Male genital system 38 Organa genitalia feminina – Female genital system 42 Systema endocrinum – Endocrine system 45 Systema cardiovasculare et lymphaticum [Angiologia] – Cardiovascular and lymphatic system 47 Systema nervosum – Nervous system 52 Receptores sensorii et Organa sensuum – Sensory receptors and Sense organs 58 Integumentum – Integument 64 INTRODUCTION The preparations leading to the publication of the present first edition of the Nomina Histologica Veterinaria has a long history spanning more than 50 years. Under the auspices of the World Association of Veterinary Anatomists (W.A.V.A.), the International Committee on Veterinary Anatomical Nomenclature (I.C.V.A.N.) appointed in Giessen, 1965, a Subcommittee on Histology and Embryology which started a working relation with the Subcommittee on Histology of the former International Anatomical Nomenclature Committee. In Mexico City, 1971, this Subcommittee presented a document entitled Nomina Histologica Veterinaria: A Working Draft as a basis for the continued work of the newly-appointed Subcommittee on Histological Nomenclature. This resulted in the editing of the Nomina Histologica Veterinaria: A Working Draft II (Toulouse, 1974), followed by preparations for publication of a Nomina Histologica Veterinaria.